How Does Arch Height Factor Into Running-Related Injuries?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2016 XTERRA Worlds Guide 10.5 2007 XTERRA Maui Press Guide.Qxd
2016 PRESS GUIDE XTERRA WORLD CHAMPIONSHIP PARTNERS Presented by Paul Mitchell, Maui Visitors Bureau, XTERRA TV on Amazon Video, Outrigger Resorts, Hawaii Tourism Authority, XTERRA Travel, Muscle Milk, Gatorade Endurance, PowerBar, Optic Nerve, XTERRA Wetsuits, XTERRA Fitness, XTERRA Boards, Compex, Greenlayer, The Ritz-Carlton, Kapalua, Kona Brewing Company, and Cycle City. XTERRA, CELEBRATING 20 YEARS OF ADVENTURE IN MAUI When you think of Maui, cascading waterfalls, white sand beaches, and breathtaking sunsets come straight to mind. This magical Hawaiian island is also the birthplace of the most notorious off-road triathlon in the world…XTERRA! From a one-off race held on the most remote island chain in the world XTERRA evolved into an endurance sports lifestyle with worldwide appeal. Over the past 20 years XTERRA transcended its status as 'just a race' to become a bona fide way of life for thousands of intrepid triathletes and trail runners across the globe. A fitting representation of this “XTERRA Tribe” - more than 800 athletes from 46 countries – will gather at Kapalua Resort and on Sunday, October 23, they’ll put their mental and physical toughness up against Mother Nature at the 21st edition (20th anniversary) of XTERRA Worlds. Follow the race online at www.xterramaui.com, on twitter @xterraoffroad and on Facebook.com/xterraplanet starting at 9am Hawaii time. All the action is being filmed for a one- hour TV special to be broadcast across the U.S., Europe, and on ESPN International starting in mid-January, 2017. TABLE OF CONTENTS Press Information . .6 Schedule of Events . .7 How to Watch Guide for Spectators and Quick Facts . -

Itu World Triathlon Series | Auckland | Sandiego | Yokohama | Madrid | Kitzbühel | Hamburg | Stockholm | London
2013 SERIES GUIDE ITU WORLd tRIATHLON SERIES | AUCKLAND | SAN DIEGO | YOKOHAMA | MADRID | KITZBÜHEL | HAMBURG | STOCKHOLM | LONDON ITU WORLD TRIATHLON SERIES | 2013 SERIES GUIDE 2 MEDIA CONTACTS ERIN GREENE MORGAN INGLIS Media Manager, ITU Communications Senior Producer, TV & Broadcast, ITU [email protected] [email protected] Office: + 34 915 421 855 Office: +1 604 904 9248 Mob: +34 645 216 509 Mobile: +1 604 250 4091 CARSTEN RICHTER OLIVER SCHIEK Upsolut Senior Director - TV Rights Upsolut Senior Director - TV Production [email protected] [email protected] Direct: +49 40 88 00 - 73 Direct: +49 40 88 18 00 - 48 Mobile: +49 170 56 39 008 Mobile: +49 170 34 29 886 ITU MEDIA CENTRE | MEDIA.TRIATHLON.ORG ITU’s Online Media Centre has been produced to provide a portal for media to quickly gather all relevant information about ITU, its events and athletes. Media Centre services include: • Latest ITU news and press releases • Up-to-date results, rankings and race statistics • Comprehensive athlete profile database • Rights-free high-resolution photos from all major events • Full audio from athlete interviews • Access to broadcast quality race video highlights For more information, or to register for a Media Centre account, visit media.triathlon.org. 3 2013 SERIES GUIDE | Itu WORLD TRIATHLON SERIES TABLE OF CONTENTS WELCOME TO THE SERIES Welcome from ITU President ..................................................... 04 Series Overview ������������������������������������������������������������������������� 05 -

August 27, 2018 the Bank of America Chicago Marathon Welcomes Strong American Field to Contend for the Crown at the 41St Annual
August 27, 2018 The Bank of America Chicago Marathon Welcomes Strong American Field to Contend for the Crown at the 41st Annual Event Olympic Gold Medalist and Two-Time Triathlon World Champion Gwen Jorgensen Joins Previously Announced Top Americans Galen Rupp, Jordan Hasay, Amy Cragg and Laura Thweatt CHICAGO – The Bank of America Chicago Marathon announced today that defending champion Galen Rupp and American superstars Jordan Hasay, Amy Cragg and Laura Thweatt will be Joined by a strong field of American runners at the 41st annual Bank of America Chicago Marathon. They will also go head-to-head with a mighty contingent of international athletes led by Mo Farah, past champions Abel Kirui and Dickson Chumba, 2017 runner-up Brigid Kosgei, and two- time third-place finisher and sub-2:20 runner Birhane Dibaba. “We are thrilled with this year’s overall elite field,” said Bank of America Chicago Marathon Executive Race Director Carey Pinkowski. “There is an incredible amount of talent and momentum on the American women’s side, and Rupp is leading a resurgence on the men’s side. These athletes are going to put on quite a show in October, and they are going to keep alive Chicago’s legacy of supporting and showcasing top U.S. athletes.” American Men’s Field Elkanah Kibet surprised race commentators during his marathon debut at the 2015 Bank of America Chicago Marathon when he bolted to the front of the elite field with 22 miles to go and put a 15-second gap on the field. The chase pack caught him at mile nine, and many suspected that Kibet’s bold move would spell disaster in the later stages of the race. -

WISCONSIN in the OLYMPICS All-Time List of Individuals from the University of Wisconsin Who Participated As Athletes and Coaches
WISCONSIN IN THE OLYMPICS All-time list of individuals from the University of Wisconsin who participated as athletes and coaches. (through 2014 Winter Olympics) ATHLETES Years at Olympic Years in Name (Country) Institution Sport Olympics (Medals Won) Emil Breitkreutz (USA) 1902, 1904-05 Men’s Track and Field 1904 (bronze) George Poage (USA) 1902-04 Men’s Track and Field 1904 (bronze-2) Frank Waller (USA) Men’s Track and Field 1904 (silver-2) Arlie Mucks, Sr. (USA) 1915-16 Men’s Track and Field 1912 Arlie Schardt (USA) Men’s Track and Field 1920 (gold) Charles McGinnis (USA) 1925-27 Men’s Track and Field 1928 (bronze) Don Gehrmann (USA) 1947-50 Men’s Track and Field 1948 Lloyd LaBeach (PANAMA) 1946 Men’s Track and Field 1948 (bronze-2) Stewart MacDonald (USA) 1967-72 Men’s Rowing 1968, 1972 David Bush (USA) 1971-72 Men’s Diving 1972 Mike Manley (USA) 1963-64 Men’s Track and Field 1972 Paul Jarvie 1973-77 Men’s Swimming 1972, 1976 Ben Peterson (USA)* Wrestling 1972 (gold)-76 (silver)-80 Neil Rogers 1973, 75 Men’s Swimming 1972, 1976 Steve Alley (USA) 1972-77 Men’s Ice Hockey 1976 Bob Espeseth (USA)* 1972-75 Men’s Rowing 1976, 1980, 1984 (bronze), 1988 Carie Graves (USA)* 1974-76 Women’s Rowing 1976 (bronze), 1980, 1984 (gold) Jim Haines (USA) 1973-77 Wrestling 1976 Neil Haleen (USA) 1963-67 Men’s Rowing 1976 Russ Hellickson (USA)* 1968-70 Wrestling 1976 (silver), 1980 Bob Lundeen (USA) 1971-75 Men’s Ice Hockey 1976 Peggy McCarthy (USA)* 1975-78 Women’s Rowing 1976 (bronze), 1980 Alte Melberg 1973-76 Men’s Swimming 1976 Tim Michelson 1966-70 -

University of Washington Dempsey Indoor Sub-4-Minute Miles
University of Washington Dempsey Indoor Sub-4-Minute Miles Totals: 214 sub-fours by 150 different athletes 2020 2020 MPSF Championships - 2/29/20 George Duggan Portland 3:59.61 2020 UW Last Chance Meet - 2/21/20 Dan Curts Unattached 3:59.29 Jack Anstey Illinois State 3:59.93 2020 Husky Classic - 2/14/20 James West Oregon 3:57.43 Theo Quax Northern Arizona 3:58.13 Takieddi Hedeilli Texas Tech 3:58.88 Charlie Hunter Oregon 3:59.01 Dustin Nading Washington 3:59.25 2020 UW Invitational - 2/1/20 Evan Jager Bowerman Track Club 3:56.50 Sean McGorty Bowerman Track Club 3:57.19 George Kusche Nebraska 3:57.93 Talem Franco BYU 3:58.09 Sam Tanner Washington 3:59.01 Dustin Nading Washington 3:59.77 2020 UW Indoor Preview - 1/18/20 Ben Blankenship Nike OTC Elite 3:57.67 Brannon Kidder Brooks Beasts 3:58.43 Mick Stanovsek Washington 3:59.58 200th sub-four 2019 2019 MPSF Championships - 2/23/19 William Paulson Arizona State 3:58.07 Joe Klecker Colorado 3:58.51 Paul Ryan Washington State 3:58.79 2019 Last Chance College Elite Meet - 2/16/19 Carlos Villarreal Arizona 3:57.27 Charlie Hunter Oregon 3:57.74 James West Oregon 3:57.75 Mick Stanovsek Washington 3:58.64 Blake Haney Oregon 3:58.73 David Ribich Brooks Beasts 3:58.91 Jackson Mestler Oregon 3:59.77 2019 Husky Classic - 2/8/19 Sam Worley Texas 3:57.98 Henry Wynne Brooks Beasts 3:58.00 Reed Brown Oregon 3:58.22 Brannon Kidder Brooks Beasts 3:58.95 2019 UW Invitational - 1/26/19 Neil Gourley Nike OTC 3:58.12 Kasey Knevelbaard Southern Utah 3:58.54 Alex Rogers Texas 3:58.79 Alex Ostberg Stanford 3:59.31 -

IAAF DIAMOND LEAGUE 2013 Eugene (USA) 31 May - 1 June 2013
IAAF DIAMOND LEAGUE 2013 Eugene (USA) 31 May - 1 June 2013 Records Set SA 1 JUN 2013 Record Event Phase Athlete / Team Nat Result Type AR High Jump Men Final BARSHIM Mutaz Essa QAT 2.40 WL Bowerman Mile Final KIPLAGAT Silas KEN 3:49.48 110m Hurdles Men Final PARCHMENT Hansle JAM 13.05 High Jump Men Final BARSHIM Mutaz Essa QAT 2.40 Pole Vault Men Final LAVILLENIE Renaud FRA 5.95 Long Jump Men Final MENKOV Aleksandr RUS 8.39 Discus Men Final HARTING Robert GER 69.75 International Mile Men Final MAGUT James Kiplagat KEN 3:55.24 5000m Men Final SOI Edwin Cheruiyot KEN 13:04.75 10000m Men Final BEKELE Kenenisa ETH 27:12.08 800m Women Final NIYONSABA Francine BDI 1:56.72 5000m Women Final DIBABA Tirunesh ETH 14:42.01 400m Hurdles Women Final HEJNOVÁ Zuzana CZE 53.70 Triple Jump Women Final SALADUKHA Olha UKR 14.85 MR 3000m Steeplechase Men Final KIPRUTO Conseslus KEN 8:03.59 High Jump Men Final BARSHIM Mutaz Essa QAT 2.40 800m Women Final NIYONSABA Francine BDI 1:56.72 Javelin Women Final OBERGFÖLL Christina GER 67.70 1500m Women Final OBIRI Hellen KEN 3:58.58 NR 110m Hurdles Men Final PARCHMENT Hansle JAM 13.05 High Jump Men Final DROUIN Derek CAN 2.36 High Jump Men Final BARSHIM Mutaz Essa QAT 2.40 Legend AR Area Record MR Meeting Record NR National Record WL World Lead INTERNET Service: www.diamondleague-eugene.com Page 1 of 1 Timing, Results Service & Distance Measurement by printed at SAT 1 JUN 2013 15:26 IAAF DIAMOND LEAGUE 2013 Eugene (USA) 31 May - 1 June 2013 REVISED 1 5 JUN 14:13 Results 200m Men 1 JUN 2013 / 14:13 Wind: -0.9 m/s -
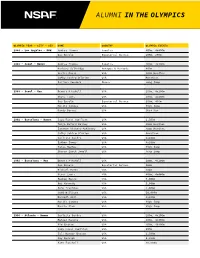
Alumni in the Olympics
ALUMNI IN THE OLYMPICS OLYMPIC YEAR - CITY - SEX NAME COUNTRY OLYMPIC EVENTS 1984 - Los Angeles - M&W Andrea Thomas Jamaica 400m, 4x400m Gus Envela Equatorial Guinea 100m, 200m 1988 - Seoul - Women Andrea Thomas Jamaica 400m, 4x400m Barbara Selkridge Antigua & Barbuda 400m Leslie Maxie USA 400m Hurdles Cathy Schiro O'Brien USA Marathon Juliana Yendork Ghana Long Jump 1988 - Seoul - Men Dennis Mitchell USA 100m, 4x100m Steve Lewis USA 400m, 4x400m Gus Envela Equatorial Guinea 200m, 400m Hollis Conway USA High Jump Randy Barnes USA Shot Put 1992 - Barcelona - Women Suzy Favor Hamilton USA 1,500m Tonja Buford Bailey USA 400m Hurdles Janeene Vickers-McKinney USA 400m Hurdles Cathy Schiro O'Brien USA Marathon Carlette Guidry USA 4x100m Esther Jones USA 4x100m Tanya Hughes USA High Jump Sharon Couch-Jewell USA Long Jump 1992 - Barcelona - Men Dennis Mitchell USA 100m, 4x100m Gus Envela Equatorial Guinea 100m Michael Bates USA 200m Steve Lewis USA 400m, 4x400m Reuben Reina USA 5,000m Bob Kennedy USA 5,000m John Trautman USA 5,000m Todd Williams USA 10,000m Darnell Hall USA 4x400m Hollis Conway USA High Jump Darrin Plab USA High Jump 1996 - Atlanta - Women Carlette Guidry USA 200m, 4x100m Maicel Malone USA 400m, 4x400m Kim Graham USA 400m, 4X400m Suzy Favor Hamilton USA 800m Juli Henner Benson USA 1,500m Amy Rudolph USA 5,000m Kate Fonshell USA 10,000m ALUMNI IN THE OLYMPICS OLYMPIC YEAR - CITY - SEX NAME COUNTRY OLYMPIC EVENTS Ann-Marie Letko USA Marathon Tonja Buford Bailey USA 400m Hurdles Janeen Vickers-McKinney USA 400m Hurdles Shana Williams -

Teen Sensation Athing Mu
• ALL THE BEST IN RUNNING, JUMPING & THROWING • www.trackandfieldnews.com MAY 2021 The U.S. Outdoor Season Explodes Athing Mu Sets Collegiate 800 Record American Records For DeAnna Price & Keturah Orji T&FN Interview: Shalane Flanagan Special Focus: U.S. Women’s 5000 Scene Hayward Field Finally Makes Its Debut NCAA Formchart Faves: Teen LSU Men, USC Women Sensation Athing Mu Track & Field News The Bible Of The Sport Since 1948 AA WorldWorld Founded by Bert & Cordner Nelson E. GARRY HILL — Editor JANET VITU — Publisher EDITORIAL STAFF Sieg Lindstrom ................. Managing Editor Jeff Hollobaugh ................. Associate Editor BUSINESS STAFF Ed Fox ............................ Publisher Emeritus Wallace Dere ........................Office Manager Teresa Tam ..................................Art Director WORLD RANKINGS COMPILERS Jonathan Berenbom, Richard Hymans, Dave Johnson, Nejat Kök SENIOR EDITORS Bob Bowman (Walking), Roy Conrad (Special AwaitsAwaits You.You. Projects), Bob Hersh (Eastern), Mike Kennedy (HS Girls), Glen McMicken (Lists), Walt Murphy T&FN has operated popular sports tours since 1952 and has (Relays), Jim Rorick (Stats), Jack Shepard (HS Boys) taken more than 22,000 fans to 60 countries on five continents. U.S. CORRESPONDENTS Join us for one (or more) of these great upcoming trips. John Auka, Bob Bettwy, Bret Bloomquist, Tom Casacky, Gene Cherry, Keith Conning, Cheryl Davis, Elliott Denman, Peter Diamond, Charles Fleishman, John Gillespie, Rich Gonzalez, Ed Gordon, Ben Hall, Sean Hartnett, Mike Hubbard, ■ 2022 The U.S. Nationals/World Champion- ■ World Track2023 & Field Championships, Dave Hunter, Tom Jennings, Roger Jennings, Tom ship Trials. Dates and site to be determined, Budapest, Hungary. The 19th edition of the Jordan, Kim Koffman, Don Kopriva, Dan Lilot, but probably Eugene in late June. -
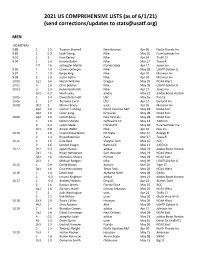
06-01-21 Us Comprehensive Lists
2021 US COMPREHENSIVE LISTS (as of 6/1/21) (send corrections/updates to [email protected]) MEN 100 METERS 9.88 1 1.5 Trayvon Bromell New Balance Apr 30 North Florida Inv 9.89 1 0.2 Isiah YounG Nike May 30 Pure Summer Inv 9.91 1 2 Fred Kerley Nike Apr 24 TruFit Cl 9.94 1 1.4 Ronnie Baker Nike Mar 27 Texas R 1f2 1.6 JoVauGhn Martin Florida State Apr 17 Jones Inv 9.96 1 1.9 Cravon Gillespie Nike May 09 USATF Golden G 9.97 1 1.9 Kyree KinG Nike Apr 10 Miramar Inv 9.98 2 1.9 Justin Gatlin Nike Apr 10 Miramar Inv 10.00 1q1 1.6 Micah Williams OreGon May 29 NCAA West 10.01 3 1.9 Chris Belcher Nike May 09 USATF Golden G 10.03 3 1.4 Kenny Bednarek Nike Apr 17 Jones Inv 1h2 0.3 Noah Lyles adidas May 23 adidas Boost Boston 10.05 1 1.4 Davonte Burnett USC May 16 Pac-12 10.06 1 1.7 Terrance Laird LSU Apr 17 Garland Inv 10.08 3h2 2 Marvin Bracy unat Apr 10 Miramar Inv 2q2 1.6 Javonte HardinG North Carolina A&T May 28 NCAA East 3q2 1.6 Lance LanG Kentucky May 28 NCAA East 10.09 4q2 1.6 Ismael Kone New Orleans May 28 NCAA East 1 1.6 Nolton Shelvin Coffeyville CC May 13 JUCO Ch 3 0.2 Jaylen Slade Florida HS May 30 Pure Summer Inv 1h1 0.8 Ameer Webb Nike Apr 16 Clay Inv 10.10 1 1.6 Cravont Charleston NC State Mar 27 Raleigh R 2 1.4 Bryce Robinson Asics Mar 27 Texas R 10.11 1 1.6 Cole Beck Virginia Tech May 15 ACC 2 1.6 Denzell FeaGin Barton CC May 13 JUCO Ch 10.12 2h2 0.3 Jaylen Bacon adidas May 23 adidas Boost Boston 2q1 1.6 Bryan Henderson Sam Houston May 29 NCAA West 5q2 1.6 Marcellus Moore Purdue May 28 NCAA East 2h2 1 Michael RodGers Nike May 09 USATF -

Varsity Magazine
CONTENTS APRIL 16, 2015 ■ VOLUME 5, ISSUE 34 BRIAN MASON COVER STORY TWO IS ONE He’s already been named the Badgers’ No. 1 quarterback, but Joel Stave is no stranger to competition and knows he isn’t the only one the QB room with eyes on the starting job. FEATURES WIDE RECEIVERS IN [FOCUS] CATCHING UP The week's best photos LUCAS AT LARGE BRIAN MASON Ted Gilmore likes the potential of Chryst’s crew catches on his wide receivers group, but the Badgers’ first-year coach is ready for BY THE NUMBERS some playmakers to step forward. Facts and figures on UW WHAT TO WATCH Quest for the Cup begins LUCAS AT LARGE ASK THE BADGERS Favorite gulity pleasure TV? CHRYST’S CREW BADGERING Steve Berg (Men’s Rowing) New head coach Paul Chryst looks BRIAN MASON INSIDE WOMEN’S HOCKEY at spring practice as an opportuni Ammerman justly honored ty to set the stage for his first sea INSIDE TRACK & FIELD son at the helm of his alma mater. UW alums star on big stages -SCROLL FOR MORE INSIDE SOFTBALL Stewart doing it all for UW Wisconsin Athletic Communications Kellner Hall, 1440 Monroe St., Madison, WI 53711 VIEW ALL ISSUES Brian Lucas Director of Athletic Communications Julia Hujet Editor/Designer Brian Mason Managing Editor Mike Lucas Senior Writer Matt Lepay Columnist Drew Scharenbroch Video Production Amy Eager Advertising Drew Pittner-Smith Distribution Contributors Paul Capobianco, Tam Flarup, Kelli Grashel, A.J. Harrison, Brandon Harrison, Patrick Herb, Diane Nordstrom Photography David Stluka, Neil Ament, Greg Anderson, Bob Campbell, Pam Ruschell, Cal Sport Media, Icon Sportswire Cover Photo: David Stluka Problems or Accessibility Issues? [email protected] © 2015 Board of Regents of the University of Wisconsin System. -

Thursday, April 16, 2015
collegiate/elite/high school division thursday, april 16, 2015 historic hilmer lodge stadium mt. san antonio college walnut, california THURSDAY; APRIL 16, 2015 RUNNING EVENT SCHEDULE TIME EVENT# GENDER EVENT SECTION 6:00 PM 110 M 3,000M Steeplechase C 6:11 PM 111 M 3,000M Steeplechase B 6:22 PM 210 W 3,000M Steeplechase C 6:35 PM 211 W 3,000M Steeplechase B 6:48 PM 212 W 3000M Steeplechase A 7:01 PM 112 M 3,000M Steeplechase A thursday running events running thursday 7:15 PM 121 M 10,000M A 7:45 PM 221 W 10,000M A 8:27 PM 222 W 10,000M INV B 9:04 PM 223 W 10,000M INV A 9:46 PM 122 M 10,000M INV B 10:16 PM 123 M 10,000M INV A 10:44 PM 120 M 10,000M B 11:15 PM 220 W 10,000M B DISCLAIMER: AN ATHLETES/TEAMS HEAT AND LANE (within an event#) ARE SUBJECT TO CHANGE. Changes may occur due to scratches, verification of marks, etc. At the Mt. SAC Relays we try our best to create fair, equitable and exciting FULL FIELD races. We thank you for your cooperation. UPDATED ON APRIL 15, 2015 @ 10:00 PM Mt. San Antonio College Hy-Tek's MEET MANAGER 9:53 PM 4/15/2015 Page 1 57th ANNUAL MT. SAC RELAYS "Where the world's best athletes compete" Hilmer Lodge Stadium, Walnut, California - 4/16/2015 to 4/18/2015 Meet Program - Thursday Track Event 110 Men's 3000 Meter Steeplechase C C/O Event 111 Men's 3000 Meter Steeplechase B C/O Thursday 4/16/2015 - 6:00 PM Thursday 4/16/2015 - 6:11 PM World Record: 7:53.63 2004 Saif Shaheen World Record: 7:53.63 2004 Saif Shaheen American Rec: 8:04.71 2014 Evan Jager American Rec: 8:04.71 2014 Evan Jager Meet Record: 8:26.14 -

2016TN02 Mlist
Volume 15, No. 02 January 06, 2016 version i — 2015 U.S. Men’s Lists — KEY TO LISTS compiled by Glen McMicken These lists give the top 40 U.S. performers (and top 10 per- formances, denoted by a ——) of the 2015 season, with an appending of those foreign collegians whose marks fall into 100 METERS that range. In the wind-aided category, the domestics and 9.74 ............ Justin Gatlin (Nike) .................. 5/15 ............. Doha DL foreign collegians are commingled (' after name = foreigner 9.75 ............ ——Gatlin ................................ 6/04 ............ Rome DL on windy list). Relay teams may contain non-U.S. nationals. ................... ——Gatlin ................................ 7/09 ...... Lausanne DL 9.77 ............ ——Gatlin ................................ 8/23 ............ World Ch Athletes who change nationality during the season are listed 9.78 ............ ——Gatlin ................................ 7/17 .........Monaco DL with their nationality as of the date of the mark, so marks 9.80 ............ ——Gatlin ................................ 8/23 ............ World Ch here may not be their actual best of the year. 9.84 ............ **Trayvon Bromell (Bay) ........... 6/25 ................ USATF Open athletes and high schoolers have no notation before 9.86 ............ Mike Rodgers (Nike) ................ 8/23 ............ World Ch their name. Collegians are noted by class: - = senior; * = 9.87 ............ Tyson Gay (Nike) ..................... 6/26 ................ USATF junior; **=soph; *** = frosh. 9.88 ............ ——Gay................................... 5/30 ..........Eugene DL (A) = altitude over 1000m (in affected events only). Wind-aided ................... ——Rodgers ........................... 7/11 ........ Madrid IWC marks are those of greater than 2.0mps. Windy marks are **11 performances by 4 performers** listed only if superior to the best legal mark (windy perfor- 9.93 ............ Ryan Bailey (Nike) ................... 5/09 ..... Kingston IWC mances listed to level of legal performances).