Wednesday, April 8, 2015 4 P.M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endothelin System and Therapeutic Application of Endothelin Receptor
xperim ACCESS Freely available online & E en OPEN l ta a l ic P in h l a C r m f o a c l a o n l o r g u y o J Journal of ISSN: 2161-1459 Clinical & Experimental Pharmacology Research Article Endothelin System and Therapeutic Application of Endothelin Receptor Antagonists Abebe Basazn Mekuria, Zemene Demelash Kifle*, Mohammedbrhan Abdelwuhab Department of Pharmacology, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia ABSTRACT Endothelin is a 21 amino acid molecule endogenous potent vasoconstrictor peptide. Endothelin is synthesized in vascular endothelial and smooth muscle cells, as well as in neural, renal, pulmonic, and inflammatory cells. It acts through a seven transmembrane endothelin receptor A (ETA) and endothelin receptor B (ETB) receptors belongs to G protein-coupled rhodopsin-type receptor superfamily. This peptide involved in pathogenesis of cardiovascular disorder like (heart failure, arterial hypertension, myocardial infraction and atherosclerosis), renal failure, pulmonary arterial hypertension and it also involved in pathogenesis of cancer. Potentially endothelin receptor antagonist helps the treatment of the above disorder. Currently, there are a lot of trails both per-clinical and clinical on endothelin antagonist for various cardiovascular, pulmonary and cancer disorder. Some are approved by FAD for the treatment. These agents are including both selective and non-selective endothelin receptor antagonist (ETA/B). Currently, Bosentan, Ambrisentan, and Macitentan approved -

[Product Monograph Template
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION Kinevac® (Sincalide) For Injection 5 mcg/vial Diagnostic Cholecystokinetic Bracco Imaging Canada Date of Initial Approval: Montreal, Quebec July 2, 1996 Canada, H1J 2Z4 Date of Revision: October 30, 2019 Submission Control No: 231066 Product Monograph Kinevac® Page 1 of 14 TABLE OF CONTENTS TABLE OF CONTENTS ............................................................................................................. 2 PART I: HEALTH PROFESSIONAL INFORMATION ................................................................. 3 1 INDICATIONS ................................................................................................................. 3 Pediatrics ........................................................................................................................ 3 Geriatrics ......................................................................................................................... 3 2 CONTRAINDICATIONS .................................................................................................. 3 3 DOSAGE AND ADMINISTRATION ................................................................................ 4 Recommended Dose and Dosage Adjustment ................................................................ 4 Reconstitution .................................................................................................................. 4 4 OVERDOSAGE .............................................................................................................. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Summary of Appeals & Independent Review Organization
All Other Appeals All other appeals are for drugs not in an inpatient hospital setting that Molina was not able to approve. Sometimes, the clinical information sent to us for these drugs do not meet medical necessity on initial review. When drug preauthorization requests are denied, a member or provider has the right to appeal. Appeals allow time to provide more clinical information. With complete clinical information, we can usually approve the drug. These are considered an appeal overturn. When the denial decision is not overturned, it is considered upheld. Service Code/Drug Name Service Code Description Number of Appeals Number of Appeals Total Appeals Upheld Overturned A9274 EXTERNAL AMB INSULIN DEL SYSTEM DISPOSABLE EA 0 1 1 Abatacept 3 1 4 Abemaciclib 1 0 1 Acalabrutinib 0 1 1 Acne Combination - Two Ingredient 1 0 1 Acyclovir 0 1 1 Adalimumab 7 14 21 Adrenergic Combination - Two Ingredient 1 0 1 Aflibercept 0 2 2 Agalsidase 1 0 1 Alfuzosin 1 0 1 Amantadine 1 0 1 Ambrisentan 0 1 1 Amphetamine 0 1 1 Amphetamine Mixtures - Two Ingredient 1 8 9 Apixaban 7 21 28 Apremilast 12 13 25 Aprepitant 0 1 1 Aripiprazole 5 9 14 ARNI-Angiotensin II Recept Antag Comb - Two Ingredient 6 9 15 Asenapine 0 1 1 Atomoxetine 1 3 4 Atorvastatin 0 1 1 Atovaquone 1 0 1 Axitinib 0 1 1 Azathioprine 0 1 1 Azilsartan 1 0 1 Azithromycin 1 0 1 Baclofen 0 1 1 Baricitinib 1 1 2 Belimumab 0 1 1 Benralizumab 1 0 1 Beta-blockers - Ophthalmic Combination - Two Ingredient 0 2 2 Bimatoprost 0 1 1 Botulinum Toxin 1 4 5 Buprenorphine 4 3 7 Calcifediol 1 0 1 Calcipotriene -

Chapter 12 Monographs of 99Mtc Pharmaceuticals 12
Chapter 12 Monographs of 99mTc Pharmaceuticals 12 12.1 99mTc-Pertechnetate I. Zolle and P.O. Bremer Chemical name Chemical structure Sodium pertechnetate Sodium pertechnetate 99mTc injection (fission) (Ph. Eur.) Technetium Tc 99m pertechnetate injection (USP) 99m ± Pertechnetate anion ( TcO4) 99mTc(VII)-Na-pertechnetate Physical characteristics Commercial products Ec=140.5 keV (IT) 99Mo/99mTc generator: T1/2 =6.02 h GE Healthcare Bristol-Myers Squibb Mallinckrodt/Tyco Preparation Sodium pertechnetate 99mTc is eluted from an approved 99Mo/99mTc generator with ster- ile, isotonic saline. Generator systems differ; therefore, elution should be performed ac- cording to the manual provided by the manufacturer. Aseptic conditions have to be maintained throughout the operation, keeping the elution needle sterile. The total eluted activity and volume are recorded at the time of elution. The resulting 99mTc ac- tivity concentration depends on the elution volume. Sodium pertechnetate 99mTc is a clear, colorless solution for intravenous injection. The pH value is 4.0±8.0 (Ph. Eur.). Description of Eluate 99mTc eluate is described in the European Pharmacopeia in two specific monographs de- pending on the method of preparation of the parent radionuclide 99Mo, which is generally isolated from fission products (Monograph 124) (Council of Europe 2005a), or produced by neutron activation of metallic 98Mo-oxide (Monograph 283) (Council of Europe 2005b). Sodium pertechnetate 99mTc injection solution satisfies the general requirements of parenteral preparations stated in the European Pharmacopeia (Council of Europe 2004). The specific activity of 99mTc-pertechnetate is not stated in the Pharmacopeia; however, it is recommended that the eluate is obtained from a generator that is eluted regularly, 174 12.1 99mTc-Pertechnetate every 24 h. -

(12) United States Patent (10) Patent No.: US 6,803,046 B2 Metcalfe Et Al
USOO6803046B2 (12) United States Patent (10) Patent No.: US 6,803,046 B2 Metcalfe et al. (45) Date of Patent: Oct. 12, 2004 (54) SINCALIDE FORMULATIONS OTHER PUBLICATIONS (75) Inventors: Edmund C. Metcalfe, Hillsborough, NJ Sitzmann, et al., “Cholecystokinin Prevents Parenteral (US); Jo Anna Monteferrante, Raritan Nutrition Induced Biliary Sludge in Humans.” Surgery, Township, NJ (US); Margaret Gynecology & Obstetrics, vol. 170, Jan. 1990, pp. 25-31. Newborn, Hamilton Township, NJ Teitelbaum et al., “Treatment of Parenteral Nutrition-ASSo (US); Irene Ropiak, Lawrenceville, NJ ciated Cholestasis with Cholecystokinin-Octapeptide,” (US); Ernst Schramm, North Journal of Pediatric Surgery, vol. 30, No. 7, Jul. 1995, pp. Brunswick, NJ (US); Gregory W. 1082-1085. White, Monmouth Junction, NJ (US); Moss and Amii, “New Approaches to Understanding the Julius P. Zodda, Mercerville, NJ (US) Etiology and Treatment of Total Parenteral Nutrition-ASSo ciated Cholestasis,” Seminars in Pediatric Surgery, vol. 8, (73) Assignee: Bracco International B.V., Amsterdam No. 3, Aug. 1999, pp. 140–147. (NL) Teitelbaum, "Parenteral Nutrition-ASSociated Cholestasis,” c: - Current Opinion in Pediatrics, vol. 9, 1997, pp. 270–275. (*) Notice: Subject to any State the SME, tly Teitelbaum and Tracy, “Parenteral Nutrition-Associated patent is extended or adjusted under Cholestasis,” Seminars in Pediatric Surgery, vol. 10, No. 2, U.S.C. 154(b) by 0 days. May 2001, pp. 72–80. Strickley, “Parenteral Formulations of Small Molecules (21) Appl. No.: 10/222,540 Therapeutics Marketed in the United States (1999) -Part (22) Filed: Aug. 16, 2002 1, PDA Journal of Pharmaceutical Science & Technology, e - Vs vol. 53, No. 6, Nov.-Dec. 1999, pp. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Drugs and Biologicals Fee Schedule
Payment Allowance Limits for PEIA Effective January 1, 2013 through December 31, 2013 The absence or presence of a HCPCS code does not indicate PEIA coverage. Similarily, the inclusion of a payment limit does not indicate coverage by PEIA. processing the claim. Vaccine Infusion DME Infusion Blood Clotting HCPCS Code Short Description HCPCS Code Dosage Payment Limit AWP% Vaccine Limit AWP% Limit AWP% Blood limit Factor Notes 90371 Hep b ig, im 1 ML$ 104.73 90375 Rabies ig, im/sc 150 IU$ 206.47 90376 Rabies ig, heat treated 150 IU$ 197.46 90385 Rh ig, minidose, im 50 MCG$ 24.62 90585 Bcg vaccine, percut 50 MG$ 120.87 90586 Bcg vaccine, intravesical 1 EACH$ 120.87 90632 Hep a vaccine, adult im 1 ML$ 50.93 90654 Flu vaccine, intradermal, no preserv 0.1 ML$ 18.98 95 18.981 90655 Flu vaccine no preserv 6-35m, im 0.25 ML$ 16.46 95 16.456 90656 Flu vaccine no preserv 3 yo & >, im 0.50 ML$ 12.40 95 12.398 90657 Flu vaccine, 6-35 mo, im 0.25 ML$ 6.02 95 6.023 90660 Flu vaccine, nasal 0.2 ML$ 23.46 95 23.456 90662 Flu vacc prsv free inc antig 0.5 ML$ 30.92 95 30.923 90669 Pneumococcal vacc, 7 val im 0.5 ML$ 95.48 95 95.481 90670 Pneumococcal vacc, 13 val im 0.5 ML$ 137.03 95 137.028 90675 Rabies vaccine, im 1 ML$ 190.40 90691 Typhoid vaccine, im 0.5 ML$ 68.27 90703 Tetanus vaccine, im 0.5 ML$ 35.41 90714 Td vaccine no prsrv >/= 7 yo, im 0.5 ML$ 19.93 90715 Tdap => 7 yo, im 0.5 ML$ 33.35 90717 Yellow fever vaccine, sc 0.5 ML$ 71.49 90732 Pneumococcal vaccine 0.5 ML$ 65.77 95 65.774 90733 Meningococcal vaccine, sc 0.5 ML$ 106.49 90735 Encephalitis -

Foi-276-1213-02.Pdf
Application Date Application Drug Name Generic Drug Name Indication Status Approved neovascular age-related macular degeneration (AMD) as per the Novartis Lucentis ranibizumab APPROVED 27/11/2012 Pharmaceuticals Australia Pty Ltd protocol cholecalciferol moderate to severe Vitamin D deficiency APPROVED 2/07/2012 Cholecystokinin for imaging of the biliary tract APPROVED 12/09/2011 cholecystokinin Kinevac/ Sincalide imaging of the biliary tract APPROVED 12/09/2011 cholecystokinin Kinevac/ Sincalide for use in nuclear medicine biliary studies APPROVED 12/09/2011 Melatonin sleep disturbance in children with severe disabilities APPROVED 25/08/2011 Indocyanine Green retinal angiography APPROVED 13/09/2011 Cholecystokinin Sincalide, Kinevac for imaging of the biliary tract. APPROVED 13/09/2011 cholecystekinin Kinevac/ Sincalide use in imaging of the biliary tract APPROVED 13/09/2011 during vitreo-retinal surgery and for intravenous injection to perform ICG Indocyanine Green APPROVED 12/09/2011 angiography during vitreo-retinal surgery and for intravenous injection to perform ICG Indocyanine Green APPROVED 12/09/2011 angiography. during vitreo-retinal suegery and for intravenous injection to perform ICG Indocyanine Green APPROVED 12/09/2011 angiography during vitreo-retinal surgery and for intravenous injection to perform ICG Indocyanine Green APPROVED 8/11/2011 angiography. Cholecystokinin Sincalide, Kinevac for nuclear medicine biliary studies. APPROVED 14/11/2011 Mafenide 5% Sulfamylon for wound management of deep partial and full thickness -

Drugs Used As Interventional Agents in Nuclear Medicine
THE UNIVERSITY OF NEW MEXICO HEALTH SCIENCES CENTER COLLEGE OF PHARMACY ALBUQUERQUE, NEW MEXICO The University of New Mexico Correspondence Continuing Education Courses for Nuclear Pharmacists and Nuclear Medicine Professionals VOLUMEVII, NUMBER2 Drugs Used as Interventional Agents in Nuclear Medicine by: Vivian S.bveless, PharmD, RPh, BCNP o The Univemi~ of New Mexico Health Sciencw Center Collcg. of ~armacy is mpprovd by the American Council on Pharmaceutical Wucation ~ a provider m@ of continuing pharmaceutical ducacion. Program No. 039-000-98-001 -HM. 2,5 Contnct Hours or .25 CWS Coorditi”ng Wifor and Director of Phrmacy Co&”nuing Educ&”on William B. Hladik III, MS, RPh College of Pharmacy University of New Mexico Health Sciences Center Assoctie ~tior and Production Spectitit Sharon 1. Magers Ramirez, Administrative Assistant II College of Pharmacy University of New Mexico Health Sciences Center Witotial Board George H Hinkle, MS, RPh, BCNP William B. Hladik III, MS, RPh Jeffrey P. Norenbtirg, MS, RPh, BCNP Laura L. Boles Ponto, PhD, RPh Timothy M. Quinton, PharmD, MS, RPh, BCNP Guwt Reviewer Sam C. Augustine, PharmD, RPh, BCNP While the advice and information in thi~ publication are believd to be true and accurate at press time, neither the author(s) nor the editor nor the publisher can accept any legat responsibility for my errom or omissions tbt may be made. Thc publisher makes no warranty, express or implied, with res~t to the material contained herein. Copyright 1998 University of New Mexico Health Sciences Center Pharmacy Continuing Hucation Albuquerque, New Mexico DRUGS USED AS INTERVENTIONAL AGENTS IN NUCLEAR MEDICINE STATEMENT OF OBJECTIVES The primary purpose of this lesson is to provide a basic understanding of drugs used as interventional agents in the practice of nuclear medicine. -

Ambrisentan (Letairis®) Issued by PHA’S Scientific Leadership Council Information Is Based on the United States Food and Drug Administration Drug Labeling
Ambrisentan (Letairis®) Issued by PHA’s Scientific Leadership Council Information is based on the United States Food and Drug Administration drug labeling Last Updated November 2013 WHAT IS AMBRISENTAN? Ambrisentan is an oral medication classified as an endothelin receptor antagonist (ERA) which is approved for the treatment of pulmonary arterial hypertension (PAH) in World Health Organization (WHO) Group 1 patients. The goal of this therapy is to improve exercise ability and slow progression of the disease. Ambrisentan was approved for PAH by the United States Food and Drug Administration (FDA) in 2007. HOW DOES AMBRISENTAN WORK? Ambrisentan works by blocking endothelin, a substance made by the body. Endothelin causes blood vessels to narrow (constrict). It also causes abnormal growth of the muscle in the walls of the blood vessels in the lungs. This narrowing increases the pressure required to push the blood through the lungs to get oxygen. By blocking the action of endothelin, causing vessels to relax, ambrisentan decreases the pulmonary blood pressure to the heart and improves its function. This generally results in the ability to be more active. Research studies have verified this improvement. HOW IS AMBRISENTAN GIVEN? Ambrisentan is taken orally, with or without food. There are two FDA approved doses; 5 mg (pale pink and square) or 10 mg (dark pink and oval). Patients’ physicians will decide which strength is right for them. HOW IS AMBRISENTAN SUPPLIED? Ambrisentan comes in 5 and 10 mg, film-coated, unscored tablets. The 5 mg tablet is pale pink and square. The 10 mg tablet is deep pink and oval. -
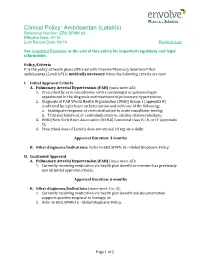
Ambrisentan (Letairis) Reference Number: ERX.SPMN.84 Effective Date: 07/16 Last Review Date: 06/16 Revision Log
Clinical Policy: Ambrisentan (Letairis) Reference Number: ERX.SPMN.84 Effective Date: 07/16 Last Review Date: 06/16 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Policy/Criteria It is the policy of health plans affiliated with Envolve Pharmacy Solutions® that ambrisentan (Letairis®) is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Pulmonary Arterial Hypertension (PAH) (must meet all): 1. Prescribed by or in consultation with a cardiologist or pulmonologist experienced in the diagnosis and treatment of pulmonary hypertension; 2. Diagnosis of PAH World Health Organization (WHO) Group 1 (appendix B) confirmed by right heart catheterization and with one of the following: a. Inadequate response or contraindication to acute vasodilator testing; b. Trial and failure of, or contraindication to, calcium channel blockers; 3. WHO/New York Heart Association (NYHA) functional class II, III, or IV (appendix C); 4. Prescribed dose of Letairis does not exceed 10 mg once daily. Approval Duration: 3 months B. Other diagnoses/indications: Refer to ERX.SPMN.16 - Global Biopharm Policy. II. Continued Approval A. Pulmonary Arterial Hypertension (PAH) (must meet all): 1. Currently receiving medication via health plan benefit or member has previously met all initial approval criteria. Approval Duration: 6 months B. Other diagnoses/indications (must meet 1 or 2): 1. Currently receiving medication via health plan benefit and documentation supports positive response to therapy; or 2. Refer to ERX.SPMN.16 - Global Biopharm Policy. Page 1 of 5 CLINICAL POLICY Ambrisentan Background Description/Mechanism of Action: Letairis is the brand name for ambrisentan, an endothelin receptor antagonist that is selective for the endothelin type-A (ETA) receptor.