Aspects of Solvent Chemistry for Calcium Hydroxide Medicaments
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
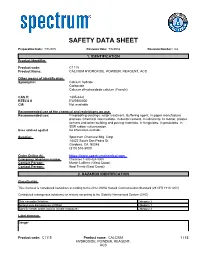
SDS Contains All of the Information Required by the HPR
SAFETY DATA SHEET Preparation Date: 7/7/2015 Revision Date: 7/6/2018 Revision Number: G2 1. IDENTIFICATION Product identifier Product code: C1115 Product Name: CALCIUM HYDROXIDE, POWDER, REAGENT, ACS Other means of identification Synonyms: Calcium hydrate Carboxide Calcium dihydroxidede calcium (French) CAS #: 1305-62-0 RTECS # EW2800000 CI#: Not available Recommended use of the chemical and restrictions on use Recommended use: Fireproofing coatings. water treatment. Buffering agent. In paper manufacture process. Chemical intermediate. In dental cement. In lubricants. In mortar, plaster, cement and other building and paving materials. In fungicides. In pesticides. In SBR rubber vulcanization. Uses advised against No information available Supplier: Spectrum Chemical Mfg. Corp 14422 South San Pedro St. Gardena, CA 90248 (310) 516-8000 Order Online At: https://www.spectrumchemical.com Emergency telephone number Chemtrec 1-800-424-9300 Contact Person: Martin LaBenz (West Coast) Contact Person: Ibad Tirmiz (East Coast) 2. HAZARDS IDENTIFICATION Classification This chemical is considered hazardous according to the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Considered a dangerous substance or mixture according to the Globally Harmonized System (GHS) Skin corrosion/irritation Category 2 Serious eye damage/eye irritation Category 1 Specific target organ toxicity (single exposure) Category 3 Label elements Danger Product code: C1115 Product name: CALCIUM 1 / 13 HYDROXIDE, POWDER, REAGENT, ACS Hazard statements Causes skin irritation Causes serious eye damage May cause respiratory irritation Hazards not otherwise classified (HNOC) Not Applicable Other hazards Not available Precautionary Statements - Prevention Wash face, hands and any exposed skin thoroughly after handling Avoid breathing dust/fume/gas/mist/vapors/spray Use only outdoors or in a well-ventilated area Wear protective gloves Wear eye/face protection Precautionary Statements - Response IF IN EYES: Rinse cautiously with water for several minutes. -

Microstructural and Compressive Strength Analysis for Cement Mortar with Industrial Waste Materials
Available online at www.CivileJournal.org Civil Engineering Journal Vol. 6, No. 5, May, 2020 Microstructural and Compressive Strength Analysis for Cement Mortar with Industrial Waste Materials Zahraa Fakhri Jawad a, Rusul Jaber Ghayyib a, Awham Jumah Salman a* a Al-Furat Al-Awsat Technical University, Najaf, Kufa, Iraq. Received 06 December 2019; Accepted 02 March 2020 Abstract Cement production uses large quantities of natural resources and contributes to the release of CO2. In order to treat the environmental effects related to cement manufacturing, there is a need to improve alternative binders to make concrete. Accordingly, extensive study is ongoing into the utilization of cement replacements, using many waste materials and industrial. This paper introduces the results of experimental investigations upon the mortar study with the partial cement replacement. Fly ash, silica fume and glass powder were used as a partial replacement, and cement was replaced by 0%, 1%, 1.5%, 3% and 5% of each replacement by the weight. Compressive strength test was conducted upon specimens at the age of 7 and 28 days. Microstructural characteristic of the modified mortar was done through the scanning electron microscope (SEM) vision, and X-ray diffraction (XRD) analysis was carried out for mixes with different replacements. The tests results were compared with the control mix. The results manifested that all replacements present the development of strength; this improvement was less in the early ages and raised at the higher ages in comparison with the control specimens. Microstructural analysis showed the formation of hydration compounds in mortar paste for each replacement. This study concluded that the strength significantly improved by adding 5% of silica fume compared with fly ash and glass powder. -

ACUMER™ 9000 Mineral Slurry Dispersant
Technical Data ACUMER™ 9000 Mineral Slurry Dispersant Description ACUMER™ 9000 is a sodium salt of an acrylic acid-based polymer. It is a highly effective dispersant for aqueous calcium hydroxide and magnesium hydroxide slurries. Features and • Controlling phase separation Benefits • Reducing caking and clogging of equipment • Aiding the remixing of slurries after settling Typical Properties Property Typical Value Appearance Clear, light amber solution Total solids, % 44 pH 7.5 Density (lb/gal, @ 25°C) 10.8 Brookfield viscosity, (mPa.s/cps @ 25°C) 500 These properties do not constitute specifications. Performance Many problems can be encountered in producing calcium hydroxide or magnesium hydroxide slurries, including: • Wettability • Phase separation • Caking • Pumping • Pipe clogging • Remixing after setting • Slurry viscosity Calcium Hydroxide Figure 1 shows the efficiency of ACUMER 9000 as a dispersant for 30% calcium hydroxide slurry. Figure 1. ACUMER 9000 Dosage vs. Viscosity (30% Lime Slurry) Page 1 of 4 ®™Trademark of The Dow Chemical Company (“Dow”) or an affiliated company of Dow Form No. 812-00352-0216BBI ACUMER™ 9000 / Dow Oil, Gas & Mining The following table shows the positive effect of ACUMER™ 9000 dosage on lime slurry stability. Lower dosage (0.2%) gives higher slurry viscosity and lower syneresis (liquid phase separation). The desired slurry properties can be controlled by optimizing the dispersant dosage. Effect of ACUMER 9000 Dispersant on 30% Lime Slurry1 Stability After 8 Days at Room Temperature Initial Make-Down Dosage, % (solids basis) Syneresis Gel3 Flowed4 Viscosity2 0.2 2080 1.7 98.3 93.3 0.4 810 12.0 88.0 97.1 0.6 382 16.5 83.5 96.3 130% lime slurry was prepared by mixing 210 grams of slaked lime with 490 grams of deionized water (including additives) for five minutes in a Waring blender at high speed. -

The Effect of Various Hydroxide and Salt Additives on the Reduction of Fluoride Ion Mobility in Industrial Waste
sustainability Article The Effect of Various Hydroxide and Salt Additives on the Reduction of Fluoride Ion Mobility in Industrial Waste Tadas Dambrauskas 1,* , Kestutis Baltakys 1, Agne Grineviciene 1 and Valdas Rudelis 2 1 Department of Silicate Technology, Kaunas University of Technology, LT-50270 Kaunas, Lithuania; [email protected] (K.B.); [email protected] (A.G.) 2 JSC “Lifosa”, LT-57502 Kedainiai, Lithuania; [email protected] * Correspondence: [email protected] Abstract: In this work, the influence of various hydroxide and salt additives on the removal of F− ions from silica gel waste, which is obtained during the production of AlF3, was examined. The leaching of the mentioned ions from silica gel waste to the liquid medium was achieved by the application of different techniques: (1) leaching under static conditions; (2) leaching under dynamic conditions by the use of continuous liquid medium flow; and (3) leaching in cycles under dynamic conditions. It was determined that the efficiency of the fluoride removal from this waste depends on the w/s ratio, the leaching conditions, and the additives used. It was proven that it is possible to reduce the concentration of fluorine ions from 10% to <5% by changing the treatment conditions and by adding alkaline compounds. The silica gel obtained after the leaching is a promising silicon dioxide source. Keywords: fluorine ions; silica gel waste; leaching; hydroxide additives Citation: Dambrauskas, T.; Baltakys, K.; Grineviciene, A.; Rudelis, V. The 1. Introduction Effect of Various Hydroxide and Salt Waste management and the reduction of pollution are the priority areas of environ- Additives on the Reduction of mental protection in the World [1–4]. -

How to Make Concrete More Sustainable Harald Justnes1
Journal of Advanced Concrete Technology Vol. 13, 147-154, March 2015 / Copyright © 2015 Japan Concrete Institute 147 Scientific paper How to Make Concrete More Sustainable Harald Justnes1 A selected paper of ICCS13, Tokyo 2013. Received 12 November 2013, accepted 16 February 2015 doi:10.3151/jact.13.147 Abstract Production of cement is ranking 3rd in causes of man-made carbon dioxide emissions world-wide. Thus, in order to make concrete more sustainable one may work along one or more of the following routes; 1) Replacing cement in con- crete with larger amounts of supplementary cementing materials (SCMs) than usual, 2) Replacing cement in concrete with combinations of SCMs leading to synergic reactions enhancing strength, 3) Producing leaner concrete with less cement per cubic meter utilizing plasticizers and 4) Making concrete with local aggregate susceptible to alkali silica reaction (ASR) by using cement replacements, thus avoiding long transport of non-reactive aggregate. 1 Introduction SCMs, also uncommon ones like calcined marl 2. Replacing cement in concrete with combinations of The cement industry world-wide is calculated to bring SCMs leading to synergic reactions enhancing about 5-8% of the total global anthropogenic carbon strength dioxide (CO2) emissions. The general estimate is about 3. Producing leaner concrete with less cement per cubic 1 tonne of CO2 emission per tonne clinker produced, if meter utilizing plasticizers. fossil fuel is used and no measures are taken to reduce it. 4. Making concrete with local aggregate susceptible to The 3rd rank is not because cement is such a bad mate- alkali silica reaction (ASR) by using cement re- rial with respect to CO2 emissions, but owing to the fact placements, thus avoiding long transport of non- that it is so widely used to construct the infrastructure reactive aggregate and buildings of modern society as we know it. -

Consolidation of Natural Stone with Calcium Hydroxide Nanosuspension in Ethanol and Verification of Surface Hardening Rate
Structural Studies, Repairs and Maintenance of Heritage Architecture XVI 359 CONSOLIDATION OF NATURAL STONE WITH CALCIUM HYDROXIDE NANOSUSPENSION IN ETHANOL AND VERIFICATION OF SURFACE HARDENING RATE KLÁRA KROFTOVÁ1, DAVID ŠKODA2, JIŘÍ WITZANY3 & TOMÁŠ ČEJKA3 1Department of Architecture, Faculty of Civil Engineering, Czech Republic 2Centre of Polymer Systems, Tomas Bata University in Zlin, Czech Republic 3Department of Building Structures, Faculty of Civil Engineering, Czech Republic ABSTRACT The modern consolidating agents, used in the care of cultural heritage for the past 20 years, include dispersion and colloid systems of not only organic consolidants, but also mineral systems with particle sizes in nano-dimensions. Among these materials, calcium hydroxide nanodispersion plays an important role. The compatibility of the consolidant with the lime-based original building material, deep penetration due to the particle size, and no mobilisation of soluble salts are advantages attributed to alcoholic lime nanodispersions. The assessment of the consolidating efficiency of the tested products are based on performance of both the destructive and the non-destructive laboratory tests. The penetration depth, thermal and moisture expansion, material strength, abrasion, modulus of elasticity, vapor permeability, microstructure (porosity, pore distribution and interconnection) and density can be listed as monitored criteria. For historical material is also important to monitor the change of color or texture on visible surface of the material. The paper presents a partial result of the NAKI II DG16P02M005 research project dealing with the verification of potential use of selected lime nanosuspensions (newly prepared calcium hydroxide nanosuspensions in alcohols and market available lime-nanodispersion CaLoSiL®) for the consolidation of historic lime based materials. -

New Approaches to Biodiesel Production by Ethanolysis with Calcium Hydroxide Catalyst Using Thermal Pretreatment with Glycerol
562 J. Jpn. Inst. Energy, Vol.Journal 89, No. of 6, the 2010 Japan Institute of Energy, 89, 562-566 (2010) Original Paper New Approaches to Biodiesel Production by Ethanolysis with Calcium Hydroxide Catalyst Using Thermal Pretreatment with Glycerol Hendrex KAZEMBE-PHIRI * 1, Yukihiko MATSUMURA * 1, and Tomoaki MINOWA * 2 (Received February 10, 2010) This was a study to pursue new sustainable sources of power in Malawi and other developing countries of Sub-Saharan Africa by investigating a novel approach for biodiesel production via ethanolysis of pre- treated oil feedstock with calcium hydroxide using thermal pretreatment with glycerol. 0.5 g of Groundnut (Arachis hypogaea) oil feedstock premixed with glycerol and Ca(OH)2 was thermally pretreated at 100℃ and stirred at 1000 rpm for 1-3 h. The triglycerides (TG) decomposed into diglycerides (DG) and monoglycerides (MG), which are reactive intermediates of the ethanolysis. This effect of pretreatment was investigated in comparison with the effect of other catalyst. Then, the pretreated oil was reacted under the following conditions: 100℃, 12-to-1 ethanol (EtOH)-to-oil molar ratio, stirring at 1000 rpm, catalyst load of 2 wt%, time from 0.5-2 h. Thermal pretreatment with glycerol achieved a significant fatty acid ethyl ester (FAEE) yield of 76 wt% (comparable to the yields obtained with calcium oxide (h-CaO) and surface-modified calcium oxide (s-CaO)). In tests on the reuse of the Ca(OH)2 catalyst in repeated reactions, the yield did not decrease sharply with repetitive use. Given that all of the materials tested in our experiments are available renewably in Sub- Saharan Africa, we believe that biodiesel production via ethanolysis has the potential to provide a sustain- able source of power in that region. -
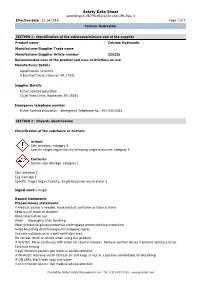
Sds.Com Safety Data Sheet According to 29CFR1910/1200 and GHS Rev
Safety Data Sheet according to 29CFR1910/1200 and GHS Rev. 3 Effective date : 12.14.2014 Page 1 of 7 Calcium Hydroxide, SECTION 1 : Identification of the substance/mixture and of the supplier Product name : Calcium Hydroxide, Manufacturer/Supplier Trade name: Manufacturer/Supplier Article number: S25225 Recommended uses of the product and uses restrictions on use: Manufacturer Details: AquaPhoenix Scientific 9 Barnhart Drive, Hanover, PA 17331 Supplier Details: Fisher Science Education 15 Jet View Drive, Rochester, NY 14624 Emergency telephone number: Fisher Science Education Emergency Telephone No.: 800-535-5053 SECTION 2 : Hazards identification Classification of the substance or mixture: Irritant Skin irritation, category 2 Specific target organ toxicity following single exposure, category 3 Corrosive Serious eye damage, category 1 Skin Irritation 2 Eye Damage 1 Specific Target Organ Toxicity, Single Exposure (respiratory) 3 Signal word :Danger Hazard statements: Precautionary statements: If medical advice is needed, have product container or label at hand Keep out of reach of children Read label before use Wash … thoroughly after handling Wear protective gloves/protective clothing/eye protection/face protection Avoid breathing dust/fume/gas/mist/vapours/spray Use only outdoors or in a well-ventilated area Do not eat, drink or smoke when using this product IF IN EYES: Rinse cautiously with water for several minutes. Remove contact lenses if present and easy to do. Continue rinsing If eye irritation persists get medical advice/attention IF INHALED: Remove victim to fresh air and keep at rest in a position comfortable for breathing IF ON SKIN: Wash with soap and water If skin irritation occurs: Get medical advice/attention Created by Global Safety Management, Inc. -

Effect of Water Losses by Evaporation and Chemical Reaction in an Industrial Slaker Reactor
339 Vol.50, n. 2 : pp.339-347, March 2007 ISSN 1516-8913 Printed in Brazil BRAZILIAN ARCHIVES OF BIOLOGY AND TECHNOLOGY AN INTERNATIONAL JOURNAL Effect of Water Losses by Evaporation and Chemical Reaction in an Industrial Slaker Reactor Ricardo Andreola 1, Osvaldo Vieira 2, Onélia Aparecida Andreo dos Santos 1 and Luiz Mario de Matos Jorge 1* 1Departamento de Engenharia Química; Universidade Estadual de Maringá; Av. Colombo, 5790 - Bloco D90; [email protected], 87020-900; Maringá - PR - Brasil. 2Klabin Paraná Papéis; Fazenda Monte Alegre; Bairro Harmonia; 84275-000; Telêmaco Borba - PR - Brasil ABSTRACT A dynamic model of the slaker reactor was developed and validated for Klabin Paraná Papéis causticizing system, responsable for white liquor generation used by the plant. The model considered water losses by evaporation and chemical reaction. The model showed a good agreement with the industrial plant measures of active alkali, total titratable alkali and temperature, without the need of adjustment of any parameter. The simulated results showed that the water consumption by the slaking reaction and evaporation exerted significant influence on the volumetric flow rate of limed liquor, which imposed a decrease of 4.6% in the amount of water in reactor outlet. Key words: Slaker reactor, modeling and simulation, white liquor INTRODUCTION Ca(OH) 2(s) . In turn, green liquor is a liquid solution with a large quantity of sodium carbonate that The causticizing reactor system from Klabin reacts with calcium hydroxide producing sodium Paraná Papéis produce white liquor used in hydroxide and calcium carbonate, according to the cellulose digesters. This system is composed by causticizing reaction: Na 2CO 3(aq) + Ca(OH) 2(s) → 2 one slaker reactor followed by nine causticizing NaOH (aq) + CaCO 3(s) . -
The Prospective Approach for the Reduction of Fluoride Ions Mobility in Industrial Waste by Creating Products of Commercial Value
sustainability Article The Prospective Approach for the Reduction of Fluoride Ions Mobility in Industrial Waste by Creating Products of Commercial Value Valdas Rudelis 1, Tadas Dambrauskas 2 , Agne Grineviciene 2 and Kestutis Baltakys 2,* 1 JSC “Lifosa”, Juodkiskio g. 50, LT-57502 Kedainiai, Lithuania; [email protected] 2 Department of Silicate Technology, Kaunas University of Technology, Radvilenu 19, LT-50270 Kaunas, Lithuania; [email protected] (T.D.); [email protected] (A.G.) * Correspondence: [email protected]; Tel.: +370-730-0163; Fax: +370-730-0152 Received: 20 December 2018; Accepted: 23 January 2019; Published: 25 January 2019 Abstract: In this work, we present the possibility to reduce the amount of fluoride ions in silica gel waste by using different techniques or to immobilize these ions by creating products of commercial value. The leaching of fluoride ions from silica gel waste to the liquid medium was done under static and dynamic conditions. It was determined that the removal of fluoride ions from this compound depends on various factors, such as dissociation, solubility, the w/s ratio, reaction temperature, leaching conditions, the adsorption properties of silica gel waste, and others. The obtained results showed that, by applying different techniques, the quantity of fluoride ions can be reduced by 60%, while obtained water was neutralized by calcium hydroxide. Additionally, it was determined that silica gel waste is a promising raw material for the hydrothermal synthesis of a stable compound containing fluoride ions–cuspidine. Keywords: fluoride ions; silica gel waste; leaching; hydrothermal synthesis; cuspidine 1. Introduction The disposal of industrial by-products is becoming an increasing concern for many industries due to the large amounts of wastes generated and increasing costs of operating landfills in combination with the scarcity of landfill sites [1–8]. -

Thermodynamic Properties of the Alkaline Earth Metal Hydroxides (MOH) L Literature Citations
NBS PUBLICATIONS A111D5 7SaflT^ NATL INST OF STANDARDS & TECH R.I.C. F COMMERCE A1 11 02752899 Chase, Malcolm W/Thermodynamic propertle ndards QC100 .U5753 N0.1243 1987 V198 C.I NBS-P NBS Technical Note 1243 Thermodynamic Properties of the Altcaline Earth Metal Hydroxides (MOH) L Literature Citations Malcolm W. Chase NBb NBS NBS NBS NBS NBS NBS NBS NBS NBS ^BS NBS NBS NBS NBS NBS NBS NBS NBS NBS NBS NBS V/?^ NR<=i WBS NBS NP"^ NBS NBS NBS^ W:^ NBS NBS NBS NBS NBS NBS NBS NBS NB: 'BS NBS NBS NBS NBS NBS NBS NBS NBS /vi. M National Bureau ofStandards NBS NBS NRS \ f?^: v/?9 WBS NP"^ NBS ^ BS NB: !\t NB^ .'BS NBS NBS i\BS NBS NBS '^-^ NB NB'-' ^ \BS NBS NBS NBS NB^ .% Center for Radiation Research The Center for Radiation Research is a major component of the National Measurement Laboratory in the National Bureau of Standards. The Center provides the Nation with standards and measurement services for ionizing radiation and for ultraviolet, visible, and infrared radiation; coordinates and furnishes essential support to the National Measurement Support Systemfor ionizing radiation; conducts research in radiation related fields to develop improved radiation measurement methodology; and generates, conpiles, and critically evaluates data to meet major national needs. The Center consists of five Divisions and one Group. Atomic and Plasma Radiation Division Carries out basic theoretical and experimental research into the • Atomic Spectroscopy spectroscopic and radiative properties of atoms and highly ionized • Atomic Radiation Data species; develops well-defined atomic radiation sources as radiometric • Plasma Radiation or wavelength standards; develops new measurement techniques and methods for spectral analysis and plasma properties; and collects, compiles, and critically evaluates spectroscopic data. -

Calcium Hydroxide As a Highly Alkaline Ph Standard Roger G
Journal of Research of the National Bureau of Standards Vol. 56, No.6, June 1956 Research Paper 2680 Calcium Hydroxide as a Highly Alkaline pH Standard Roger G . Bates/ Vincent E. Bower/ and Edgar R. Smith The National Bureau of Standards conventional activity scale of pH is defin ed by a series of standard buffer solutions prepared from certified materials issued as N BS Standard Samples. The five standards thus far established cover the pH range 1.68 to 9.18 at 25° . In order to increa e t he accuracy of measurements at high pH, a highly alkaline standard is needed. A solution of calci um hydroxide saturated at 25° C is recommended as the sixth pH standard. K 0 weighing is necessary, for the solution is easily prepared by shaking fin cly granular calcium hydroxide with water. The material must not be contaminated with soluble alkalies, but the presence of insoluble carbonate is of no co ncern. The filtered solution supersaturates readily and can usually be used from 0° to 60° C without the separa t ion of solid phase. E lectromotive-force measurements of 29 cells containing mixtures of calcium hydroxide and potassi um chloride were made in the range 0° to 60° C, and standard pH values were [ assigned to 0.0203-, 0.02- 0.019-, 0.0175-, and 0.015-M solutions of calcium hydroxide I_ without added chloride. the saturated solution is about 0.0203 M and has a pH of 12.45 at 25 ° C. The buffer capacity is high (0.09 mole/pH).