Parliament of India Lok Sabha
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

December COMMITTEE on PETITIONS (FIFTEENTH LOK
COMMITTEE ON PETITIONS (FIFTEENTH LOK SABHA) THIRTY-SECOND REPORT LOK SABHA SECRETARIAT NEW DELHI December , 2013 / Agrahayana, 1935 (Saka) THIRTY-SECOND REPORT COMMITTEE ON PETITIONS (FIFTEENTH LOK SABHA) MINISTRY OF RAILWAYS (Presented to Hon'ble Speaker on 04.01.2014) LOK SABHA SECRETARIAT NEW DELHI December , 2013 / Agrahayana, 1935 (Saka) CPB NO. 1 Vol.XXXII Price: Rs……….. (c) 2013 BY LOK SABHA SECRETARIAT Published under Rule 382 of the Rules of Procedure and Conduct of Business in Lok Sabha (Fifteenth Edition) and printed by the General Manager, Government of India Press, Minto Road, New Delhi – 110 092 (ii) CONTENTS Pages COMPOSITION OF THE COMMITTEE ON PETITIONS……………………. (iii) INTRODUCTION………………………….………………………………………. (v) REPORT Representations from Shri Anandrao Adsul and Smt. Bhavana Gawali Patil, MPs, Lok Sabha regarding : Conversion of narrow Gauge Railway Lines Yawatmal-Murtizapur-Achalpur-Pulgaon into Broad Gauge and other related issues. ANNEXURES i) Minutes of the 44 th sitting of the Committee held on 29.05.2012 ii) Minutes of the 54 th sitting of the Committee held on 30.1.2013 iii) Minutes of the 61st sitting of the Committee held on 1.8.2013 iv) Minutes of the 66 th sitting of the Committee held on 17.12.2013 COMPOSITION OF THE COMMITTEE ON PETITIONS (2012-13) Shri Anant Gangaram Geete - Chairman Members 2. Shri Khiladi Lal Bairwa 3. Shri Arvind Kumar Chaudhary 4. Shri Syed Shahnawaz Hussain 5. Shri G. V. Harsha Kumar 6. Shri Bhartruhari Mahtab 7. Shri Vincent H. Pala 8. Shri A. Sai Prathap 9. Shri M.B. Rajesh 10. Prof.(Dr.) Ram Shankar 11. -

Forest Fires and Its Effect on Environment, Forests, Bio-Diversity and Wildlife and Remedial/Preventive Measures”
REPORT NO. 293 PARLIAMENT OF INDIA RAJYA SABHA DEPARTMENT-RELATED PARLIAMENTARY STANDING COMMITTEE ON SCIENCE & TECHNOLOGY, ENVIRONMENT & FORESTS TWO HUNDRED NINETY THIRD REPORT “FOREST FIRES AND ITS EFFECT ON ENVIRONMENT, FORESTS, BIO-DIVERSITY AND WILDLIFE AND REMEDIAL/PREVENTIVE MEASURES” th (Presented to the Rajya Sabha on 16 December, 2016) (Laid on the Table of Lok Sabha on 16th December, 2016) Rajya Sabha Secretariat, New Delhi December, 2016/ Agrahayana, 1938 (Saka) Website : http://rajyasabha.nic.in Email: [email protected] Hindi version of this publication is also available PARLIAMENT OF INDIA RAJYA SABHA DEPARTMENT-RELATED PARLIAMENTARY STANDING COMMITTEE ON SCIENCE & TECHNOLOGY, ENVIRONMENT & FORESTS TWO HUNDRED NINETY THIRD REPORT “FOREST FIRES AND ITS EFFECT ON ENVIRONMENT, FORESTS, BIO-DIVERSITY AND WILDLIFE AND REMEDIAL/PREVENTIVE MEASURES” (Presented to the Rajya Sabha on 16th December, 2016) (Laid on the Table of the Lok Sabha 16th December, 2016) Rajya Sabha Secretariat, New Delhi December, 2016/ Agrahayana, 1938 (Saka) C O N T E N T S PAGES 1. COMPOSITION OF THE COMMITTEE (i) – (ii) 2. INTRODUCTION (iii) *3. ACRONYMS 4. REPORT OF THE COMMITTEE *5. RECOMMENDATIONS/OBSERVATIONS-AT A GLANCE *6. MINUTES OF THE MEETINGS * To be appended at printing stage COMPOSITION OF THE COMMITTEE (2016-17) (Constituted on 1st September, 2016) ---------- 1. Shrimati Renuka Chowdhury –– Chairperson RAJYA SABHA 2. Shri Prasanna Acharya 3. Shri S.R. Balasubramoniyan 4. Shrimati Vandana Chavan 5. Shri C.P. Narayanan 6. Shri Parimal Nathwani 7. Shri Rangasayee Ramakrishna 8. Dr. T. Subbarami Reddy 9. Shri Ronald Sapa Tlau 10. Shri Ch. Sukhram Singh Yadav LOK SABHA 11. -

Government of India Ministry of Home Affairs Lok Sabha
GOVERNMENT OF INDIA MINISTRY OF HOME AFFAIRS LOK SABHA UNSTARRED QUESTION NO. †1232 TO BE ANSWERED ON THE 13th AUGUST, 2013/SRAVANA 22, 1935 (SAKA) INTRUSION ALONG BORDERS †1232. SHRI GORAKHNATH PANDEY: SHRIMATI BHAVANA GAWALI PATIL: ADV. GANESHRAO DUDHGAONKAR: SHRI UDAY SINGH: SHRIMATI SUPRIYA SULE: SHRIMATI ANNU TANDON: SHRI S.S. RAMASUBBU: SHRIMATI JAYSHREEBEN PATEL: SHRI ARJUN MEGHWAL: Will the Minister of HOME AFFAIRS be pleased to state: (a) whether there are reports of frequent intrusion at the Line of Control (LoC) and Line of Actual Control (LAC) by Pakistan and China respectively; (b) if so, whether the said issue has been raised in bilateral meetings, UN and other international agencies; (c) if so, the details and the outcome thereof; (d) whether there is any proposal to install high tension electric fencing and close circuit cameras along the Indo-Pak Border/LoC to check the instances of intrusions and infiltrations; and (e) if so, the details thereof? ANSWER MINISTER OF STATE IN THE MINISTRY OF HOME AFFAIRS (SHRI R.P.N.SINGH) (a) to (e): There is no commonly delineated Line of Actual Control (LAC) between India and China. Due to differing perceptions of LAC and both sides patrolling upto their respective perceptions, transgressions do occur. Government regularly takes up any violation along the LAC with Cont…2/- -2- L.S.U.S.Q.No.1232 for 13.8.2013 the Chinese side through established mechanisms including border personnel meetings, flag meetings, Working Mechanism on Consultation and Coordination on India-China Border Affairs and diplomatic channels. PLA transgression in the past six months is as per established pattern. -

Parliament of India R a J Y a S a B H a Committees
Com. Co-ord. Sec. PARLIAMENT OF INDIA R A J Y A S A B H A COMMITTEES OF RAJYA SABHA AND OTHER PARLIAMENTARY COMMITTEES AND BODIES ON WHICH RAJYA SABHA IS REPRESENTED (Corrected upto 4th September, 2020) RAJYA SABHA SECRETARIAT NEW DELHI (4th September, 2020) Website: http://www.rajyasabha.nic.in E-mail: [email protected] OFFICERS OF RAJYA SABHA CHAIRMAN Shri M. Venkaiah Naidu SECRETARY-GENERAL Shri Desh Deepak Verma PREFACE The publication aims at providing information on Members of Rajya Sabha serving on various Committees of Rajya Sabha, Department-related Parliamentary Standing Committees, Joint Committees and other Bodies as on 30th June, 2020. The names of Chairmen of the various Standing Committees and Department-related Parliamentary Standing Committees along with their local residential addresses and telephone numbers have also been shown at the beginning of the publication. The names of Members of the Lok Sabha serving on the Joint Committees on which Rajya Sabha is represented have also been included under the respective Committees for information. Change of nominations/elections of Members of Rajya Sabha in various Parliamentary Committees/Statutory Bodies is an ongoing process. As such, some information contained in the publication may undergo change by the time this is brought out. When new nominations/elections of Members to Committees/Statutory Bodies are made or changes in these take place, the same get updated in the Rajya Sabha website. The main purpose of this publication, however, is to serve as a primary source of information on Members representing various Committees and other Bodies on which Rajya Sabha is represented upto a particular period. -

Rajya Sabha —— Revised List of Business
RAJYA SABHA —— REVISED LIST OF BUSINESS Friday, August 6, 2010 11 A.M. ——— QUESTIONS QUESTIONS entered in separate lists to be asked and answers given. ———— PAPERS TO BE LAID ON THE TABLE I. Following Ministers to lay papers on the Table entered in the separate list: — 1. SHRI SRIKANT JENA for Ministry of Chemicals and Fertilizers; 2. SHRIMATI D. PURANDESWARI for Ministry of Human Resource Development; and 3. PROF. K.V. THOMAS for Ministry of Agriculture and Ministry of Consumer Affairs, Food and Public Distribution. II. SHRI NAMO NARAIN MEENA to lay on the Table, under clause (1) of article 151 of the Constitution, a copy each (in English and Hindi) of the following Reports:— (i) Report of the Comptroller and Auditor General of India for the year ended March, 2009: Report No.11 of 2010-11: Union Government (Indirect Taxes Central Excise) (Performance Audit) - Performance Audit on Excise Duty on Pharmaceutical Products. (ii) Report of the Comptroller and Auditor General of India for the year ended March, 2009: Report No.12 of 2010-11: Union Government (Defence Services) Army and Ordnance Factories; and (iii) Report of the Comptroller and Auditor General of India for the year ended March, 2009: Report No.15 of 2009-10: Union Government (Indirect Taxes - Customs) (Performance Audit) - Performance Audit on natural or cultured pearls, precious or semi-precious stones, precious metals, metals clad with precious metal and articles thereof, imitation jewellery, coin (Chapter 71 of Customs Tariff Heading). ———— 83 MOTION FOR ELECTION TO THE COURT -
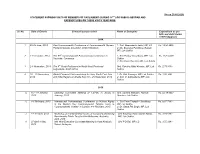
(As on 28.05.2020) STATEMENT SHOWING VISITS of MEMBERS of PARLIAMENT (DURING 16TH LOK SABHA) ABROAD and EXPENDITURES on THESE VISITS YEAR-WISE
(As on 28.05.2020) STATEMENT SHOWING VISITS OF MEMBERS OF PARLIAMENT (DURING 16TH LOK SABHA) ABROAD AND EXPENDITURES ON THESE VISITS YEAR-WISE Sl. No. Date of Events Events/Country visited Name of Delegates Expenditure as per bills and debit claims settled (Approx.) 2014 1 25-29 June, 2014 Pan-Commonwealth Conference of Commonwealth Women 1. Smt. Meenakashi Lekhi, MP, LS Rs. 14,90,882/- Parliamentarians in London, United Kingdom 2. Ms. Bhavana Pundikrao Gawali, MP, Lok Sabha 2 2-10 October, 2014 The 60th Commonwealth Parliamentary Conference in 1. Shri Pankaj Choudhary, MP, Lok Rs. 16,81,447/- Yaounde, Cameroon Sabha 2. Shri Prem Das Rai, MP, Lok Sabha 3 2-8 November, 2014 The 6th Youth Parliament in North West Provincial Smt. Raksha Nikhil Khadse, MP, Lok Rs. 2,78,000/- Legislature, South Africa Sabha 4 18 – 20 November, Global Financial Crisis workshop for Asia, South East Asia 1. Dr. Kirit Somaiya, MP, Lok Sabha Rs. 1,58,369/- 2014 and India Regions in Dhaka from 18 – 20 November, 2014 2. Smt. V. Sathyabama MP, Lok Sabha 2015 5. 15 – 18 January, Standing Committee Meeting of CSPOC in Jersey in Smt. Sumitra Mahajan, Hon’ble Rs. 55,48,005/- 2015 January, 2015 Speaker, Lok Sabha 6. 4-6 February, 2015 International Parliamentary Conference on Human Rights 1. Shri Prem Prakash Chaudhary, Rs. 9,87,784/- in the Modern Day Commonwealth “Magna Carta to MP, Lok Sabha Commonwealth Charter” in London, 4-6 February, 2015 2. Dr. Satya Pal Singh, MP, Lok Sabha 7. 8 – 10 April, 2015 Workshop on Parliamentary Codes of Conduct-Establishing Shri Kinjarapu Ram Mohan Naidu, Rs. -

MP Deepender Singh Hooda MP Arjun Ram Meghwal
INDIAN LEADERS PROGRAM, FOURTH EDITION ‐ MEMBERS OF PARLIAMENT May 31st to June 5th 2015, Madrid and Barcelona SPAIN‐INDIA COUNCIL FOUNDATION MP Deepender Singh Hooda Deepender Singh Hooda is a third term Member of Parliament for Rohtak in Haryana State constituency, whip of Indian National Congress in Lok Sabha (Lower House of Parliament), National Spokesperson of Indian National Congress. He actively serves as Member of the Parliamentary Standing Committee on Energy; and Member of the Ad hoc Committee on Absenteeism of Members in the Parliament. He also leads INC’s Social Media Communications Team. Deepender was first elected to the thirteenth Lok Sabha (in 2005) as an MP from Rohtak (Haryana) at the young age of 27. His unwavering commitment earned him a victory by a record margin (of about 4 and a half Lakh votes) when he sought re‐election to Lok‐ Sabha for the second term in 2009. He continued his winning streak for the third time in 2014 even when his party faced strong anti‐incumbency. Areas of agriculture, energy, India’s economic growth and employment potentials find Deepender's passionate involvement, both in his constituency and at a broader national level. Hooda is a third‐generation Parliamentarian from a family with a rich political heritage extending over four generations. His father, Bhupinder Singh Hooda, was the Chief Minister of Haryana for two terms from Mar 2005 ‐ Oct 2014. Deepender's grandfather, Ranbir Singh was a noted freedom fighter, an eminent parliamentarian and one of the founding fathers of India (by virtue of him being a member of the Constituent Assembly of India (1946‐1950) which was responsible for drafting the Constitution of India). -

Women in Detention and Access to Justice'
10 PARLIAMENT OF INDIA LOK SABHA COMMITTEE ON EMPOWERMENT OF WOMEN (2016-2017) (SIXTEENTH LOK SABHA) TENTH REPORT ‘WOMEN IN DETENTION AND ACCESS TO JUSTICE' LOK SABHA SECRETARIAT NEW DELHI August, 2017/Bhadrapada,1939 (Saka) TENTH REPORT COMMITTEE ON EMPOWERMENT OF WOMEN (2016-2017) (SIXTEENTH LOK SABHA) ‘WOMEN IN DETENTION AND ACCESS TO JUSTICE' Presented to Hon’ble Speaker on 30.08.2017 Presented to Lok Sabha on 22.12.2017 Laid in Rajya Sabha on 22.12.2017 LOK SABHA SECRETARIAT NEW DELHI August, 2017/Bhadrapada, 1939 (Saka) E.W.C. No. 101 PRICE: Rs._____ © 2017 BY LOK SABHA SECRETARIAT Published under ……………………………………… CONTENTS Page Nos. Composition of the Committee on Empowerment of Women (2014-2015)...................................................................................................... (iii) Composition of the Committee on Empowerment of Women (2015-2016)...................................................................................................... (iv) Composition of the Committee on Empowerment of Women (2016-2017)...................................................................................................... (v) Introduction....................................................................................................... (vi) REPORT PART I NARRATION ANALYSIS I. Introductory………………………………………………………………..... 1 II. Policing Related Issues…..…………..................................................... 4 III. Overcrowding of Jails..................................…………………………….. 4 IV. The Issue of Undertrails................................…………………………. -

List of Successful Candidates
11 - LIST OF SUCCESSFUL CANDIDATES CONSTITUENCY WINNER PARTY Andhra Pradesh 1 Nagarkurnool Dr. Manda Jagannath INC 2 Nalgonda Gutha Sukender Reddy INC 3 Bhongir Komatireddy Raj Gopal Reddy INC 4 Warangal Rajaiah Siricilla INC 5 Mahabubabad P. Balram INC 6 Khammam Nama Nageswara Rao TDP 7 Aruku Kishore Chandra Suryanarayana INC Deo Vyricherla 8 Srikakulam Killi Krupa Rani INC 9 Vizianagaram Jhansi Lakshmi Botcha INC 10 Visakhapatnam Daggubati Purandeswari INC 11 Anakapalli Sabbam Hari INC 12 Kakinada M.M.Pallamraju INC 13 Amalapuram G.V.Harsha Kumar INC 14 Rajahmundry Aruna Kumar Vundavalli INC 15 Narsapuram Bapiraju Kanumuru INC 16 Eluru Kavuri Sambasiva Rao INC 17 Machilipatnam Konakalla Narayana Rao TDP 18 Vijayawada Lagadapati Raja Gopal INC 19 Guntur Rayapati Sambasiva Rao INC 20 Narasaraopet Modugula Venugopala Reddy TDP 21 Bapatla Panabaka Lakshmi INC 22 Ongole Magunta Srinivasulu Reddy INC 23 Nandyal S.P.Y.Reddy INC 24 Kurnool Kotla Jaya Surya Prakash Reddy INC 25 Anantapur Anantha Venkata Rami Reddy INC 26 Hindupur Kristappa Nimmala TDP 27 Kadapa Y.S. Jagan Mohan Reddy INC 28 Nellore Mekapati Rajamohan Reddy INC 29 Tirupati Chinta Mohan INC 30 Rajampet Annayyagari Sai Prathap INC 31 Chittoor Naramalli Sivaprasad TDP 32 Adilabad Rathod Ramesh TDP 33 Peddapalle Dr.G.Vivekanand INC 34 Karimnagar Ponnam Prabhakar INC 35 Nizamabad Madhu Yaskhi Goud INC 36 Zahirabad Suresh Kumar Shetkar INC 37 Medak Vijaya Shanthi .M TRS 38 Malkajgiri Sarvey Sathyanarayana INC 39 Secundrabad Anjan Kumar Yadav M INC 40 Hyderabad Asaduddin Owaisi AIMIM 41 Chelvella Jaipal Reddy Sudini INC 1 GENERAL ELECTIONS,INDIA 2009 LIST OF SUCCESSFUL CANDIDATE CONSTITUENCY WINNER PARTY Andhra Pradesh 42 Mahbubnagar K. -

Agriculture Marketing and Role of Weekly Gramin Haats"
STANDING COMMITTEE ON AGRICULTURE (2018-2019) 62 SIXTEENTH LOK SABHA MINISTRY OF AGRICULTURE AND FARMERS WELFARE (DEPARTMENT OF AGRICULTURE, COOPERATION AND FARMERS WELFARE) SIXTY SECOND REPORT "AGRICULTURE MARKETING AND ROLE OF WEEKLY GRAMIN HAATS" LOK SABHA SECRETARIAT NEW DELHI January, 2019/Pausha, 1940 (Saka) Page 1 of 81 SIXTY SECOND REPORT STANDING COMMITTEE ON AGRICULTURE (2018-2019) (SIXTEENTH LOK SABHA) MINISTRY OF AGRICULTURE AND FARMERS WELFARE (DEPARTMENT OF AGRICULTURE, COOPERATION AND FARMERS WELFARE) "Agriculture Marketing and Role of Weekly Gramin Haats" Presented to Lok Sabha on 03.01.2019 Laid on the Table of Rajya Sabha on 03.01.2019 LOK SABHA SECRETARIAT NEW DELHI January, 2019/Pausha, 1940 (Saka) Page 2 of 81 COA No. 392 Price : Rs. © 2018 By Lok Sabha Secretariat Published under Rule 382 of the Rules of Procedure and Conduct of Business in Lok Sabha (Fourteenth Edition) and Printed by Page 3 of 81 <CONTENTS> PAGE No. COMPOSITION OF THE COMMITTEE (2016-17)………………………… (iii) COMPOSITION OF THE COMMITTEE (2017-18)………………………… (iv) COMPOSITION OF THE COMMITTEE (2018-19)………………………… (v) INTRODUCTION…………………………………………………………… (vi) REPORT PART- I Chapter - I Introduction A Procurement vis a vis Production of Agriculture Produce B Marketing Platform for Agriculture Produce C Functioning of Agriculture Produce Marketing Committee (APMCs) D Reform in Agriculture Produce Marketing sector E Relevance of Gramin Haat as Platform for Agriculture Marketing F Implementation of GrAM Scheme G Implementation of e-NAM scheme PART-II RECOMMENDATIONS AND OBSERVATIONS OF THE COMMITTEE ANNEXURES I. Status of Adoption of Marketing Reforms as on 18.06.2018 II. Major Recommendations of the Committee. APPENDICES I. -

The Journal of Parliamentary Information
The Journal of Parliamentary Information VOLUME LIX NO. 1 MARCH 2013 LOK SABHA SECRETARIAT NEW DELHI CBS Publishers & Distributors Pvt. Ltd. 24, Ansari Road, Darya Ganj, New Delhi-2 EDITORIAL BOARD Editor : T.K. Viswanathan Secretary-General Lok Sabha Associate Editors : P.K. Misra Joint Secretary Lok Sabha Secretariat Kalpana Sharma Director Lok Sabha Secretariat Assistant Editors : Pulin B. Bhutia Additional Director Lok Sabha Secretariat Parama Chatterjee Joint Director Lok Sabha Secretariat Sanjeev Sachdeva Joint Director Lok Sabha Secretariat © Lok Sabha Secretariat, New Delhi THE JOURNAL OF PARLIAMENTARY INFORMATION VOLUME LIX NO. 1 MARCH 2013 CONTENTS PAGE EDITORIAL NOTE 1 ADDRESSES Addresses at the Inaugural Function of the Seventh Meeting of Women Speakers of Parliament on Gender-Sensitive Parliaments, Central Hall, 3 October 2012 3 ARTICLE 14th Vice-Presidential Election 2012: An Experience— T.K. Viswanathan 12 PARLIAMENTARY EVENTS AND ACTIVITIES Conferences and Symposia 17 Birth Anniversaries of National Leaders 22 Exchange of Parliamentary Delegations 26 Bureau of Parliamentary Studies and Training 28 PARLIAMENTARY AND CONSTITUTIONAL DEVELOPMENTS 30 PRIVILEGE ISSUES 43 PROCEDURAL MATTERS 45 DOCUMENTS OF CONSTITUTIONAL AND PARLIAMENTARY INTEREST 49 SESSIONAL REVIEW Lok Sabha 62 Rajya Sabha 75 State Legislatures 83 RECENT LITERATURE OF PARLIAMENTARY INTEREST 85 APPENDICES I. Statement showing the work transacted during the Twelfth Session of the Fifteenth Lok Sabha 91 (iv) iv The Journal of Parliamentary Information II. Statement showing the work transacted during the 227th Session of the Rajya Sabha 94 III. Statement showing the activities of the Legislatures of the States and Union Territories during the period 1 October to 31 December 2012 98 IV. -
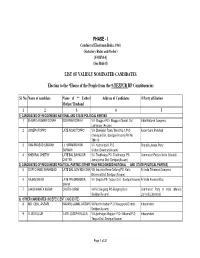
List of Validly Nominated Candidate Phase
PHASE - I Conduct of Electiomn Rules, 1961 (Statutory Rules and Order) [FORM 4] (See Rule 8) LIST OF VALIDLY NOMINATED CANDIDATES Election to the *House of the People from the 9-TEZPUR HP Constituencies Sl. No. Name of candidate Name of ** Father/ Address of Candidates @Party affiliation Mother/ Husband 1 2 3 4 5 1) CANDIDATES OF RECOGNISED NATIONAL AND STATE POLITICAL PARTIES 1 BHUPEN KUMAR BORAH BOGIRAM BORAH Vill- Bhogpur PO:- Bhogpur Chariali Dist. India National Congress Lakhimpur (Assam) 2 JOSEPH TOPPO LATE NOAS TOPPO Vill- Dhekiajuli Town, Ward No.1, P.O- Asom Gana Parishad Dhekiajuli Dist.-Sonitpur(Assam) Pin No. 784110 3 RAM PRASAD SARMAH Lt. HARINARAYAN Vill- Kacharibasti, P.O - Bharatia Janata Party SARMAH Ulubari,Guwahati(Assam) 4 KHEMRAJ CHETRY LATE BAL BAHADUR Vill- Toubhanga PO- Toubhanga PS- Communist Party of India (Marxist) CHETRY Jamugurihat Dist: Sonitpur(Assam) 2) CANDIDATES OF RECOGNISED POLITICAL PARTIES (OTHER THAN RECOGNISED NATIONAL AND STATE POLITICAL PARTIES) 5 GOPI CHAND SHAHABADI LATE BAL GOVINDA SHA Vill- Industrial Area Gotlong PO- Kalia All India Trinamool Congress Bhomora Dist. Sonitpur (Assam) 6 RAJEN SAIKIA LATE PREMANANDA Vill- Depota PS- Tezpur Dist.- Sonitpur(Assam) All India Forward Bloc SAIKIA 7 LAKSHIKANTA KURMI CHUTU KURMI Vill-NC Bargang PO-Bargang Dist.- Communist Party of India (Marxist- Sonitpur(Assam) Laninst)(Liberation) 3) OTHER CANDIDATES (INDEPENDENT CANDIDATE) 8 MD. IQBAL ANSARI KAMARU JAMAL ANSARI Vill-Medhi chuburi P.O-Rangapara District- Independent Sonitpur(Assam) 9 ELIAS KUJUR LATE JOSEPH KUJUR Vill-Jyotinagar Majgaon P.O- Nilkamal P.S- Independent Tezpur Dist. Sonitpur(Assam) Page 1 of 21 Sl.