Pediatric Supratentorial Intraventricular Tumors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Risk Factors for Gliomas and Meningiomas in Males in Los Angeles County1
[CANCER RESEARCH 49, 6137-6143. November 1, 1989] Risk Factors for Gliomas and Meningiomas in Males in Los Angeles County1 Susan Preston-Martin,2 Wendy Mack, and Brian E. Henderson Department of Preventive Medicine, University of Southern California School of Medicine, Los Angeles, California 90033 ABSTRACT views with proxy respondents, we were unable to include a large proportion of otherwise eligible cases because they were deceased or Detailed job histories and information about other suspected risk were too ill or impaired to participate in an interview. The Los Angeles factors were obtained during interviews with 272 men aged 25-69 with a County Cancer Surveillance Program identified the cases (26). All primary brain tumor first diagnosed during 1980-1984 and with 272 diagnoses had been microscopically confirmed. individually matched neighbor controls. Separate analyses were con A total of 478 patients were identified. The hospital and attending ducted for the 202 glioma pairs and the 70 meningioma pairs. Meningi- physician granted us permission to contact 396 (83%) patients. We oma, but not glioma, was related to having a serious head injury 20 or were unable to locate 22 patients, 38 chose not to participate, and 60 more years before diagnosis (odds ratio (OR) = 2.3; 95% confidence were aphasie or too ill to complete the interview. We interviewed 277 interval (CI) = 1.1-5.4), and a clear dose-response effect was observed patients (74% of the 374 patients contacted about the study or 58% of relating meningioma risk to number of serious head injuries (/' for trend the initial 478 patients). -

Original Article Outcome of Supratentorial Intraaxial Extra Ventricular Primary Pediatric Brain Tumors
Original Article Outcome of supratentorial intraaxial extra ventricular primary pediatric brain tumors: A prospective study Mohana Rao Patibandla, Suchanda Bhattacharjee1, Megha S. Uppin2, Aniruddh Kumar Purohit1 Department of Neurosurgery, Krishna Institute of Medical Sciences Secunderabad, Departments of 1Neurosurgery and 2Pathology, Nizam’s Institute of Medical Sciences, Hyderabad, Andhra Pradesh, India Address for correspondence: Dr. Mohana Rao Patibandla, Department of Neurosurgery, University of Colorado Denver, 13123, E 16th Ave, Aurora, CO 80045, USA. Email: [email protected] ABSTRACT Introduction: Tumors of the central nervous system (CNS) are the second most frequent malignancy of childhood and the most common solid tumor in this age group. CNS tumors represent approximately 17% of all malignancies in the pediatric age range, including adolescents. Glial neoplasms in children account for up to 60% of supratentorial intraaxial tumors. Their histological distribution and prognostic features differ from that of adults. Aims and Objectives: To study clinical and pathological characteristics, and to analyze the outcome using the Engel’s classification for seizures, Karnofsky’s score during the available follow‑up period of minimum 1 year following the surgical and adjuvant therapy of supratentorial intraaxial extraventricular primary pediatric (SIEPP) brain tumors in children equal or less than 18 years. Materials and Methods: The study design is a prospective study done in NIMS from October 2008 to January 2012. All the patients less than 18 years of age operated for SIEPP brain tumors proven histopathologically were included in the study. All the patients with recurrent or residual primary tumors or secondaries were excluded from the study. Post operative CT or magnetic resonance imaging (MRI) is done following surgery. -

Charts Chart 1: Benign and Borderline Intracranial and CNS Tumors Chart
Charts Chart 1: Benign and Borderline Intracranial and CNS Tumors Chart Glial Tumor Neuronal and Neuronal‐ Ependymomas glial Neoplasms Subependymoma Subependymal Giant (9383/1) Cell Astrocytoma(9384/1) Myyppxopapillar y Desmoplastic Infantile Ependymoma Astrocytoma (9412/1) (9394/1) Chart 1: Benign and Borderline Intracranial and CNS Tumors Chart Glial Tumor Neuronal and Neuronal‐ Ependymomas glial Neoplasms Subependymoma Subependymal Giant (9383/1) Cell Astrocytoma(9384/1) Myyppxopapillar y Desmoplastic Infantile Ependymoma Astrocytoma (9412/1) (9394/1) Use this chart to code histology. The tree is arranged Chart Instructions: Neuroepithelial in descending order. Each branch is a histology group, starting at the top (9503) with the least specific terms and descending into more specific terms. Ependymal Embryonal Pineal Choro id plexus Neuronal and mixed Neuroblastic Glial Oligodendroglial tumors tumors tumors tumors neuronal-glial tumors tumors tumors tumors Pineoblastoma Ependymoma, Choroid plexus Olfactory neuroblastoma Oligodendroglioma NOS (9391) (9362) carcinoma Ganglioglioma, anaplastic (9522) NOS (9450) Oligodendroglioma (9390) (9505 Olfactory neurocytoma Ganglioglioma, malignant (()9521) anaplastic (()9451) Anasplastic ependymoma (9505) Olfactory neuroepithlioma Oligodendroblastoma (9392) (9523) (9460) Papillary ependymoma (9393) Glioma, NOS (9380) Supratentorial primitive Atypical EdEpendymo bltblastoma MdllMedulloep ithliithelioma Medulloblastoma neuroectodermal tumor tetratoid/rhabdoid (9392) (9501) (9470) (PNET) (9473) tumor -

Central Nervous System Tumors General ~1% of Tumors in Adults, but ~25% of Malignancies in Children (Only 2Nd to Leukemia)
Last updated: 3/4/2021 Prepared by Kurt Schaberg Central Nervous System Tumors General ~1% of tumors in adults, but ~25% of malignancies in children (only 2nd to leukemia). Significant increase in incidence in primary brain tumors in elderly. Metastases to the brain far outnumber primary CNS tumors→ multiple cerebral tumors. One can develop a very good DDX by just location, age, and imaging. Differential Diagnosis by clinical information: Location Pediatric/Young Adult Older Adult Cerebral/ Ganglioglioma, DNET, PXA, Glioblastoma Multiforme (GBM) Supratentorial Ependymoma, AT/RT Infiltrating Astrocytoma (grades II-III), CNS Embryonal Neoplasms Oligodendroglioma, Metastases, Lymphoma, Infection Cerebellar/ PA, Medulloblastoma, Ependymoma, Metastases, Hemangioblastoma, Infratentorial/ Choroid plexus papilloma, AT/RT Choroid plexus papilloma, Subependymoma Fourth ventricle Brainstem PA, DMG Astrocytoma, Glioblastoma, DMG, Metastases Spinal cord Ependymoma, PA, DMG, MPE, Drop Ependymoma, Astrocytoma, DMG, MPE (filum), (intramedullary) metastases Paraganglioma (filum), Spinal cord Meningioma, Schwannoma, Schwannoma, Meningioma, (extramedullary) Metastases, Melanocytoma/melanoma Melanocytoma/melanoma, MPNST Spinal cord Bone tumor, Meningioma, Abscess, Herniated disk, Lymphoma, Abscess, (extradural) Vascular malformation, Metastases, Extra-axial/Dural/ Leukemia/lymphoma, Ewing Sarcoma, Meningioma, SFT, Metastases, Lymphoma, Leptomeningeal Rhabdomyosarcoma, Disseminated medulloblastoma, DLGNT, Sellar/infundibular Pituitary adenoma, Pituitary adenoma, -

Choroid Plexus Tumors: a Review
UC San Diego UC San Diego Previously Published Works Title Perinatal (fetal and neonatal) choroid plexus tumors: a review. Permalink https://escholarship.org/uc/item/0sm7q5q7 Journal Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery, 35(6) ISSN 0256-7040 Authors Crawford, John R Isaacs, Hart Publication Date 2019-06-01 DOI 10.1007/s00381-019-04135-x Peer reviewed eScholarship.org Powered by the California Digital Library University of California Child's Nervous System (2019) 35:937–944 https://doi.org/10.1007/s00381-019-04135-x REVIEW ARTICLE Perinatal (fetal and neonatal) choroid plexus tumors: a review John R. Crawford1,2,3 & Hart Isaacs Jr3,4 Received: 13 September 2018 /Accepted: 20 March 2019 /Published online: 5 April 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Introduction The object of this review is to describe the choroid plexus tumors (CPTs) occurring in the fetus and neonate with regard to clinical presentation, location, pathology, treatment, and outcome. Materials and methods Case histories and clinical outcomes were reviewed from 93 cases of fetal and neonatal tumors obtained from the literature and our own institutional experience from 1980 to 2016. Results Choroid plexus papilloma (CPP) is the most common tumor followed by choroid plexus carcinoma (CPC) and atypical choroid plexus papilloma (ACPP). Hydrocephalus and macrocephaly are the presenting features for all three tumors. The lateral ventricles are the main site of tumor origin followed by the third and fourth ventricles, respectively. CPTs of the fetus are detected most often near the end of the third trimester of pregnancy by fetal ultrasound. -

Risk-Adapted Therapy for Young Children with Embryonal Brain Tumors, High-Grade Glioma, Choroid Plexus Carcinoma Or Ependymoma (Sjyc07)
SJCRH SJYC07 CTG# - NCT00602667 Initial version, dated: 7/25/2007, Resubmitted to CPSRMC 9/24/2007 and 10/6/2007 (IRB Approved: 11/09/2007) Activation Date: 11/27/2007 Amendment 1.0 dated January 23, 2008, submitted to CPSRMC: January 23, 2008, IRB Approval: March 10, 2008 Amendment 2.0 dated April 16, 2008, submitted to CPSRMC: April 16, 2008, (IRB Approval: May 13, 2008) Revision 2.1 dated April 29, 2009 (IRB Approved: April 30, 2009 ) Amendment 3.0 dated June 22, 2009, submitted to CPSRMC: June 22, 2009 (IRB Approved: July 14, 2009) Activated: August 11, 2009 Amendment 4.0 dated March 01, 2010 (IRB Approved: April 20, 2010) Activated: May 3, 2010 Amendment 5.0 dated July 19, 2010 (IRB Approved: Sept 17, 2010) Activated: September 24, 2010 Amendment 6.0 dated August 27, 2012 (IRB approved: September 24, 2012) Activated: October 18, 2012 Amendment 7.0 dated February 22, 2013 (IRB approved: March 13, 2013) Activated: April 4, 2013 Amendment 8.0 dated March 20, 2014. Resubmitted to IRB May 20, 2014 (IRB approved: May 22, 2014) Activated: May 30, 2014 Amendment 9.0 dated August 26, 2014. (IRB approved: October 14, 2014) Activated: November 4, 2014 Un-numbered revision dated March 22, 2018. (IRB approved: March 27, 2018) Un-numbered revision dated October 22, 2018 (IRB approved: 10-24-2018) RISK-ADAPTED THERAPY FOR YOUNG CHILDREN WITH EMBRYONAL BRAIN TUMORS, HIGH-GRADE GLIOMA, CHOROID PLEXUS CARCINOMA OR EPENDYMOMA (SJYC07) Principal Investigator Amar Gajjar, M.D. Division of Neuro-Oncology Department of Oncology Section Coordinators David Ellison, M.D., Ph.D. -

Malignant CNS Solid Tumor Rules
Malignant CNS and Peripheral Nerves Equivalent Terms and Definitions C470-C479, C700, C701, C709, C710-C719, C720-C725, C728, C729, C751-C753 (Excludes lymphoma and leukemia M9590 – M9992 and Kaposi sarcoma M9140) Introduction Note 1: This section includes the following primary sites: Peripheral nerves C470-C479; cerebral meninges C700; spinal meninges C701; meninges NOS C709; brain C710-C719; spinal cord C720; cauda equina C721; olfactory nerve C722; optic nerve C723; acoustic nerve C724; cranial nerve NOS C725; overlapping lesion of brain and central nervous system C728; nervous system NOS C729; pituitary gland C751; craniopharyngeal duct C752; pineal gland C753. Note 2: Non-malignant intracranial and CNS tumors have a separate set of rules. Note 3: 2007 MPH Rules and 2018 Solid Tumor Rules are used based on date of diagnosis. • Tumors diagnosed 01/01/2007 through 12/31/2017: Use 2007 MPH Rules • Tumors diagnosed 01/01/2018 and later: Use 2018 Solid Tumor Rules • The original tumor diagnosed before 1/1/2018 and a subsequent tumor diagnosed 1/1/2018 or later in the same primary site: Use the 2018 Solid Tumor Rules. Note 4: There must be a histologic, cytologic, radiographic, or clinical diagnosis of a malignant neoplasm /3. Note 5: Tumors from a number of primary sites metastasize to the brain. Do not use these rules for tumors described as metastases; report metastatic tumors using the rules for that primary site. Note 6: Pilocytic astrocytoma/juvenile pilocytic astrocytoma is reportable in North America as a malignant neoplasm 9421/3. • See the Non-malignant CNS Rules when the primary site is optic nerve and the diagnosis is either optic glioma or pilocytic astrocytoma. -

Impact of Adjuvant Radiotherapy in Patients with Central Neurocytoma: a Multicentric International Analysis
cancers Article Impact of Adjuvant Radiotherapy in Patients with Central Neurocytoma: A Multicentric International Analysis Laith Samhouri 1,†, Mohamed A. M. Meheissen 2,3,† , Ahmad K. H. Ibrahimi 4, Abdelatif Al-Mousa 4, Momen Zeineddin 5, Yasser Elkerm 3,6, Zeyad M. A. Hassanein 2,3 , Abdelsalam Attia Ismail 2,3, Hazem Elmansy 3,6, Motasem M. Al-Hanaqta 7 , Omar A. AL-Azzam 8, Amr Abdelaziz Elsaid 2,3 , Christopher Kittel 1, Oliver Micke 9, Walter Stummer 10, Khaled Elsayad 1,*,‡ and Hans Theodor Eich 1,‡ 1 Department of Radiation Oncology, University Hospital Münster, Münster 48149, Germany; [email protected] (L.S.); [email protected] (C.K.); [email protected] (H.T.E.) 2 Alexandria Clinical Oncology Department, Alexandria University, Alexandria 21500, Egypt; [email protected] (M.A.M.M.); [email protected] (Z.M.A.H.); [email protected] (A.A.I.); [email protected] (A.A.E.) 3 Specialized Universal Network of Oncology (SUN), Alexandria 21500, Egypt; [email protected] (Y.E.); [email protected] (H.E.) 4 Department of Radiotherapy and Radiation Oncology, King Hussein Cancer Center, Amman 11942, Jordan; [email protected] (A.K.H.I.); [email protected] (A.A.-M.) 5 Department of Pediatrics, King Hussein Cancer Center, Amman 11942, Jordan; [email protected] 6 Cancer Management and Research Department, Medical Research Institute, Alexandria University, Alexandria 21500, Egypt 7 Military Oncology Center, Royal Medical Services, Amman 11942, Jordan; [email protected] 8 Princess Iman Research Center, King Hussein Medical Center, Royal Medical Services, Amman 11942, Jordan; Citation: Samhouri, L.; Meheissen, [email protected] 9 M.A.M.; Ibrahimi, A.K.H.; Al-Mousa, Department of Radiotherapy and Radiation Oncology, Franziskus Hospital Bielefeld, A.; Zeineddin, M.; Elkerm, Y.; 33699 Bielefeld, Germany; [email protected] 10 Department of Neurosurgery, University Hospital Münster, 48149 Münster, Germany; Hassanein, Z.M.A.; Ismail, A.A.; [email protected] Elmansy, H.; Al-Hanaqta, M.M.; et al. -

Central Neurocytoma in the Posterior Fossa Pranav Rai, Raghavendra Nayak, Debish Anand, Girish Menon
BMJ Case Rep: first published as 10.1136/bcr-2019-231626 on 16 September 2019. Downloaded from Images in… Central neurocytoma in the posterior fossa Pranav Rai, Raghavendra Nayak, Debish Anand, Girish Menon Neurosurgery, Kasturba Medical DESCRIPTION College Manipal, Manipal Central neurocytomas (CNs) are rare, benign Academy of Higher Education neoplasms arising from a neuronal lineage and (MAHE), Manipal, Karnataka, account for 0.1%–0.5% of all central nervous India system tumours. Typical location of CNs is the lateral ventricle touching the foramen of Correspondence to 1 Dr Raghavendra Nayak, Munro. Occurrence of the tumours in the poste- drnayakneuro@ gmail. com rior fossa is extremely rare; till now only seven cases (table 1) have been reported to the best of Figure 2 H&E staining showing (A) isomorphic 2 Accepted 21 August 2019 our knowledge. cells with clear cytoplasm, speckled chromatin and An 8-year-old girl was presented to us with fibrillar matrix. (B) Synaptophysin positivity on early morning headache and blurring of vision immunohistochemical study. for 1 month and gait instability for 15 days. These symptoms were gradually progressive. Since 3 The patient underwent a midline suboccipital days, she started having intractable nausea and craniotomy and complete excision of the tumour. vomiting. Neurological examinations showed Histopathology showed the isomorphic cells with mild papilledema and bilateral sixth nerve paresis, clear cytoplasm, speckled chromatin and fibrillar indicating raised intracranial pressure. She had matrix, suggesting oligodendroglioma or ependy- an ataxic gait. CT scan was showing an ill-de- moma. But, immunohistochemical study was posi- fined, lobulated, heterogeneously enhancing and tive for synaptophysin and neuron-specific enolase hypodense intraventricular lesion arising from and negative for glial fibrillar acidic protein, the floor of the fourth ventricle. -
Sudden Unexpected Death from Extraventricular Neurocytoma. a Case Report and Review of the Literature
Case Report J Forensic Sci & Criminal Inves Volume-3 Issue -1 April 2017 Copyright © All rights are reserved by Panagiotis Mylonakis DOI: 10.19080/JFSCI.2017.03.555603 Sudden Unexpected Death from Extraventricular Neurocytoma. A Case Report and Review of the Literature Panagiotis Mylonakis1, Stefanos Milias2, Dimitrios Pappas3 and Antigony Mitselou4* 1Medical Examiner’s Office of Thessaloniki, Greece 2Department of Pathology, 424 Military Hospital of Thessaloniki, Greece 3Department of Pathology, 401 Military Hospital of Athens, Greece 4Department of Forensic Pathology and Toxicology, University of Ioannina, Greece Submission: April 06, 2017; Published: April 19, 2017 *Corresponding author: Panagiotis Mylonakis, MD, Medical Examiner’s Office of Thessaloniki, Thessaloniki 54012, P.O.BOX: 19757, Greece, Tel: Email: Abstract Fatal brain tumors are often diagnosed well before death. Rarely, they are associated to sudden and unexpected death and encountered in medico legal autopsy practice. Neurocytomas are unusual neuronal tumors especially affecting young people and commonly arise in the ventricles with a benign outcome. Currently, these tumors have been well recognized outside the limits of the cerebral ventricules and in these unexpectedly due to a previously undiagnosed extra ventricular neurocytoma. instances, have been called “exta ventricular neurocytomas” (EVNs). The authors present the case of a 35 year-old male who died suddenly and Keywords: Brain tumors; Neurocytoma; Extra ventricular neurocytoma; Sudden death; Autopsy Introduction due to a clinically undiagnosed extra ventricular neurocytoma Central neurocytomas (CNs) are benign tumors which located on the midbrain. usually arise from the lateral ventricles [1,2]. Extra ventricular neurocytomas (EVNs) refer to tumors with similar or identical Case Report biological and histopathological characteristics to CNs, but History which arise from extra ventricular parenchymal tissue [2]. -

Low-Grade Central Nervous System Tumors
Neurosurg Focus 12 (2):Article 1, 2002, Click here to return to Table of Contents Low-grade central nervous system tumors M. BEATRIZ S. LOPES, M.D., AND EDWARD R. LAWS, JR., M.D. Departments of Pathology (Neuropathology) and Neurological Surgery, University of Virginia Health Sciences Center, Charlottesville, Virginia Low-grade tumors of the central nervous system constitute 15 to 35% of primary brain tumors. Although this cate- gory of tumors encompasses a number of different well-characterized entities, low-grade tumors constitute every tumor not obviously malignant at initial diagnosis. In this brief review, the authors discuss the pathological classification, diagnostic procedures, treatment, and possible pathogenic mechanisms of these tumors. Emphasis is given in the neu- roradiological and pathological features of the several entities. KEY WORDS • glioma • astrocytoma • treatment outcome Low-grade gliomas of the brain represent a large pro- toses. The pilocytic (juvenile) astrocytoma is a character- portion of primary brain tumors, ranging from 15 to 35% istic, more circumscribed lesion occurring primarily in in most reported series.1–5 They include a remarkable di- childhood and with a predilection for being located in the versity of lesions, all of which have been lumped together cerebellum. It usually appears as a cystic tumor with a under the heading of "low-grade glioma." This category mural nodule. The tumor tissue itself may have features of includes virtually every tumor of glial origin that is not microcystic degeneration and Rosenthal fibers which are overtly malignant at the time of initial diagnosis. degenerative structures in the astrocytic processes. Other reasonably common types of low-grade gliomas include CLASSIFICATION OF GLIOMAS the low-grade oligodendroglioma and the low-grade ependymoma, which is usually anatomically related to the Table 1 provides a classification of low-grade tumors of ventricular ependymal lining. -
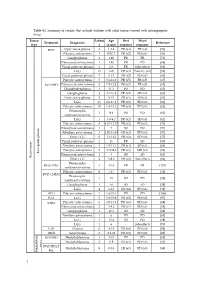
Table S1. Summary of Studies That Include Children with Solid Tumors Treated with Antiangiogenic Drugs
Table S1. Summary of studies that include children with solid tumors treated with antiangiogenic drugs. Tumor Patient Age Best Worst Treatment Diagnostic Reference type s (years) response response BVZ Optic nerve glioma 4 1.2-4 PR (x4) PR (x4) [56] Pilocytic astrocytoma 3 0.92-7 PR (x2) PD (x1) [56] Ganglioglioma 1 1.92 PR PR [56] Pilomyxoid astrocytoma 1 1.92 PR PD [68] Visual pathway glioma 1 2.6 PR Side effects [66] LGG 15 1-20 CR (x3) Toxicity (x1) [58] Visual pathway glioma 3 6-13 PR (x2) PD (x1) [60] Pilocytic astrocytoma 5 3.1-11.2 PR (x5) PR (x5) [65] BVZ+IRO Pilomyxoid astrocytoma 2 7.9-12.2 PR (x2) PR (x2) [65] Oligodendroglioma 1 11.1 PD PD [65] Ganglioglioma 3 4.1-16.8 PR (x2) SD (x1) [65] Optic nerve glioma 2 9-15 PR (x1) SD (x1) [63] LGG 35 0.6-17.6 PR (x2) PD (x8) [61] Pilocytic astrocytoma 10 1.8-15.3 PR (x4) PD (x1) [62] Pleomorphic 1 9.4 PD PD [62] xanthoastrocytoma LGG 5 3.9-9.2 PR (x2) SD (x3) [62] Pilocytic astrocytoma 4 4.67-12.17 PR (x2) PD (x3) [57] Pilomyxoid astrocytoma 1 3 SD PD [57] Fibrillary astrocytoma 3 1.92-11.08 CR (x1) PD (x3) [57] Other LGG 6 1-13.42 PR (x2) PD (x6) [57] Visual pathway glioma 1 11 PR SD [60] Fibrillary astrocytoma 3 1.5-11.1 CR (x1) SD (x1) [64] Pilocytic astrocytoma 2 3.75-9.8 PR (x1) MR (x1) [64] Low-grade glioma Pilomyxoid astrocytoma 1 3 SD SD [64] Brain tumor Brain tumor Other LGG 4 3-9.6 PR (x2) Side effects [64] Pleomorphic BVZ+TMZ 1 13.4 PR PR [153] xanthoastrocytoma Pilocytic astrocytoma 9 5-17 PR (x3) PD (x3) [59] BVZ+CHEM Pleomorphic 1 18 SD PD [59] xanthoastrocytoma Ganglioglioma