Role of the Genral Practitioner/Family
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Geriatric Medicine and Why We Need Geriatricians! by Juergen H
Geriatric Medicine and why we need Geriatricians! by Juergen H. A. Bludau, MD hat is geriatric medicine? Why is there a need for 1. Heterogeneity: As people age, they become more Wthis specialty? How does it differ from general heterogeneous, meaning that they become more and more internal medicine? What do geriatricians do differently when different, sometimes strikingly so, with respect to their they evaluate and treat an older adult? These are common health and medical needs. Imagine for a moment a group questions among patients and physicians alike. Many of 10 men and women, all 40 years old. It is probably safe internists and family practitioners argue, not unjustifiably, to say that most, if not all, have no chronic diseases, do not that they have experience in treating and caring for older see their physicians on a regular basis, and take no long- patients, especially since older adults make up almost half of term prescription medications. From a medical point of all doctors visits. So do we really need another type of view, this means that they are all very similar. Compare this physician to care for older adults? It is true that geriatricians to a group of 10 patients who are 80 years old. Most likely, may not necessarily treat older patients differently per se. But you will find an amazingly fit and active gentleman who there is a very large and important difference in that the focus may not be taking any prescription medications. On the of the treatment is different. In order to appreciate how other end of the spectrum, you may find a frail, memory- significant this is, we need to look at what makes an older impaired, and wheelchair-bound woman who lives in a adult different from a younger patient. -

General Practice Or Primary Health Care? J~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~.M
- * ..t *;-gW -~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~..._wP..;!-t . .ik. General practice or primary health care? J~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~.M.........;~~~~~~~~~~~~~~~~~~~~~~~~.........j: .-: . J. M. ,uam-.u.,. 'sr. PRIMARY health care in the UK is undergoing a period of extensive review. The 1980s have seen the publication of the green' and white papers,2 the CbeitR. *- icor - -m- --- Cumberlege review of community nursing3 and the Griffiths report on community care.4 Over the same period, the scope of primary medical care has widened, and with the setting up of independent family practitioner committees in 1985, a management framework for family practitioner services is now being created. These recent reports have reflected, rather than resolved, three major tensions in .............. primary care: between individual and population-based approaches, between employed staff and independent contractors and between broad and narrow I ~~~~~i5oms~~~~~~~~~~~~~~mcw~~~~~W-Ff.mw -W definitions of primary health care. These tensions are maintained by the way primary care services are currently provided - by family practitioner committees, district health authorities, local authorities and voluntary organizations, each with different JL i:'.;JicaPjl ways of working. .Dit.X.1 Pemra Gra . ....i Recent policy documents have done little to promote a strategic policy for primary care as a whole.5 In the green' and white ...s papers,2 primary care was reduced to the .~~~~~~ ~~~~~~~~~~~~~~~ activities of those providing family practitioner and community nursing services, with the emphasis on the former, while the Cumberlege report3 made community nursing the mainstay of primary care. Little attempt has been made to balance the .. '': :'!i.! .-".!.. Ei!.!!;-S!5.!Fl! !l'Ili.:. I~~~~.~....! -i .....J ...j.;:l........;i.. -

A Crisis in Health Care: a Call to Action on Physician Burnout
A CRISIS IN HEALTH CARE: A CALL TO ACTION ON PHYSICIAN BURNOUT Partnership with the Massachusetts Medical Society, Massachusetts Health and Hospital Association, Harvard T.H. Chan School of Public Health, and Harvard Global Health Institute A Crisis in Health Care: A Call to Action on Physician Burnout Authors About the Massachusetts Medical Society Ashish K. Jha, MD, MPH The Massachusetts Medical Society (MMS) is the state- Director, Harvard Global Health Institute wide professional association for physicians and medical stu- Senior Associate Dean for Research Translation and dents, supporting 25,000 members. The MMS is dedicated Global Strategy to educating and advocating for the physicians and patients K.T. Li Professor, Dept. of Health Policy and Management, of Massachusetts both locally and nationally. As a voice of Harvard T.H. Chan School of Public Health leadership in health care, the MMS provides physician and Professor of Medicine, Harvard Medical School patient perspectives to influence health-related legislation Andrew R. Iliff, MA, JD at both state and federal levels, works in support of public Lead Writer and Program Manager, Harvard Global health, provides expert advice on physician practice manage- Health Institute ment, and addresses issues of physician well-being. Alain A. Chaoui, MD, FAAFP About the Massachusetts Health and President, Massachusetts Medical Society Hospital Association Steven Defossez, MD, EMHL The Massachusetts Health and Hospital Association Vice President, Clinical Integration, Massachusetts Health (MHA) was founded in 1936, and its members include and Hospital Association 71 licensed member hospitals, many of which are organized Maryanne C. Bombaugh, MD, MSc, MBA within 29 member health systems, as well as interested indi- President-Elect, Massachusetts Medical Society viduals and other healthcare stakeholders. -

Guidelines for Developing a Team Physician Services Agreement in the Secondary School
Guidelines for Developing a Team Physician Services Agreement in the Secondary School The following document has been developed by the NATA Secondary School Athletic Trainers’ Committee in an effort to assist secondary school athletic trainers in strengthening and formalizing the relationship with a team physician. The included components for such an agreement have been suggested by the American College of Sports Medicine (ACSM) and NATA (see resources). Guidelines for Developing a Team Physician Agreement in the Secondary School is intended to serve as an overview of those key components as they apply to the secondary school setting. It should be noted that while all components cited have merit, not all may be practical for all situations. Variability with state and local regulations must also be considered. DEVELOPED BY THE SECONDARY SCHOOL ATHLETIC TRAINERS’ COMMITTEE: Larry Cooper, MS, ATC, LAT, Chair Kembra Mathis, MEd, ATC, LAT Bart Peterson, MSS, ATC, Incoming Chair Lisa Walker, ATC Denise Alosa, MS, ATC Stacey Ritter, MS, ATC Casey Christy, ATC Chris Snoddy, ATC, LAT George Wham, EdD, ATC, SCAT Chris Dean, ATC Dale Grooms, ATC Cari Wood, ATC, NATA BOD Liaison Dan Newman, MS, ATC, LAT Amanda Muscatell, NATA Staff Liaison A SPECIAL THANKS TO TEAM PHSYICIAN SERVICES AGREEMENT SUBCOMMITTEE: George Wham, EdD, ATC, SCAT Dale Grooms, ATC Casey Christy, ATC Larry Cooper, MS, ATC, LAT, Chair Bart Peterson, MSS, ATC, Incoming Chair NATA Secondary School Athletic Trainers’ Committee 2016 Disclaimer: The materials and information provided in the National Athletic Trainers’ Association (“NATA”) “Guidelines for Developing a Team Physician Services Agreement in the Secondary School” (the “Guideline”) are educational in nature, and the Guideline is published as a resource for NATA members and is intended solely for personal use/reference in the manner described herein. -
White and Brown Bagging Emerging Practices, Emerging Regulation
White and Brown Bagging Emerging Practices, Emerging Regulation Prepared By The National Association of Boards of Pharmacy White and Brown Bagging Emerging Practices, Emerging Regulation Published April 2018 Copyright 2018 National Association of Boards of Pharmacy 1600 Feehanville Drive Mount Prospect, IL 60056 USA 847/391‐4406 www.nabp.pharmacy Carmen A. Catizone, MS, RPh, DPh Executive Director/Secretary NABP Mission Statement NABP is the independent, international, and impartial Association that assists its member boards and jurisdictions for the purpose of protecting the public health. NABP Vision Statement Innovating and collaborating today for a safer public health tomorrow. ________________________________________________________________________ © 2018 by the National Association of Boards of Pharmacy. All rights reserved. No part of this publication may be reproduced in any manner without the written permission of the executive director/secretary of the National Association of Boards of Pharmacy. The terms “National Association of Boards of Pharmacy,” and “NABP,” are registered trademarks of the National Association of Boards of Pharmacy. Violation of the copyright will lead to prosecution under federal copyright laws. Table of Contents Overview……………………………………………………………………………………………………………………………..2 Results ………………………………………………………………………………………………………………………………..2 Results Background …………………………………………………………………………………………………………….3 Recommendations ………………………………………………………………………………………………………………5 References ………………………………………………………………………………………………………………………….6 -

The General Practitioner and the Problems of Battered Women
of medical ethics, 1979, 5, I17-123 journal J Med Ethics: first published as 10.1136/jme.5.3.117 on 1 September 1979. Downloaded from The general practitioner and the problems of battered women Jan Pahl Research Fellow, University ofKent Author's abstract occur in the 'average' practice, and a summary of This paper discusses the responsibility ofgeneral these estimates was presented by the Royal College practitioners who are consulted by women who have of General Practitioners.2 It was suggested that in been physically injured by the men with whom they an average population of 2,500 there would be live. The paper draws on a study of 50 women likely to be about I50 households living on supple- who were interviewed at a refuge for battered mentary benefit, 6o one-parent families, 25 women, and considers the help which they alcoholics, and 3-4 divorces in any one year. Such received, or did not receive, from their general estimates, of course, take no account of variations practitioners. Such women are likely to face from place to place, nor over time: the I970S have many difficulties: it is perhaps the essence of seen a great increase in the numbers of households their problem that, because it is potentially the living on supplementary benefit, and in the numbers concern of so many people, it can so easily of divorces and, consequently, of one parent families.3 Jefferys estimated that 36 - 4 per cent of all become the concern of nobody-except of the those consulting their general practitioners did so woman herself. -

The Naturalist Tradition in General Practice
The Naturalist Tradition in General Practice I, r, McWhinney, MD London, Ontario For me there have been two great satisfactions of medical practice. One has been the depth of human experience which, as physicians, we are privileged to have. The other has been the satisfaction of observing patients with illnesses of all kinds, in their own habitat, and over long periods of time. This is the kind of satisfaction experienced by all naturalists. I would claim that observation of prognosis and to rational therapeutics. The clinician, then, has much in the natural history of disease is the Suppose, for example, people with common with the naturalist. “Natu basic science of medicine. Nowadays schizophrenia were found to have a ralists,” wrote John Ryle,1 “hold cer we use the term “basic science” for biochemical abnormality. This dis tain attributes in common, notably the what Abraham Flexner called the la covery would have no significance desire to establish the truth of things boratory sciences. There is no harm in without the clinical description of a by observing and recording, by classifi this as long as we do not mean that the category called schizophrenia, and a cation and analysis.” Like the natural laboratory sciences are more funda knowledge of its natural course and ist, the clinician makes careful observa mental and more scientific than the outcome. tions of his/her patients, classifies their science of clinical observation. Chemis Medicine, like other branches of illnesses into categories, then follows try and physics can explain ill health biology, is predominantly an observa them to their conclusion. -

Practitioner Acronym Table
Practitioner Acronym Table AAP American Academy of Pediatrics ABAI American Board of Allergy and Immunology ABFP American Board of Family Practitioners ABO American Board of Otolaryngology ABPN American Board of Psychiatry and Neurology AK Acupuncturist (Pennsylvania) AOBFP American Osteopathic Board of Family Physicians American Osteopathic Board of Special Proficiency in Osteopathic Manipulative AOBSPOMM Medicine AP Acupuncture Physician ASG Affiliated Study Group BHMS Bachelor of Homeopathic Medicine and Surgery BSN Bachelor of Science, Nursing BVScAH Bachelor of Veterinary Science and Animal Husbandry CA Certified Acupuncturist CAAPM Clinical Associate of the American Academy of Pain Management CAC Certified Animal Chiropractor CCH Certified in Classical Homeopathy CCSP Certified Chiropractic Sports Physician CRNP Certified Registered Nurse Practitioner CRRN Certified Rehabilitation Registered Nurse CSPOMM Certified Specialty of Proficiency in Osteopathic Manipulation Medicine CVA Certified Veterinary Acupuncturist DAAPM Diplomate of American Academy of Pain Management DABFP Diplomate of the American Board of Family Practice DABIM Diplomate of the American Board of Internal Medicine DAc Diplomate in Acupuncture DAc (RI) Doctor of Acupuncture, Rhode Island DAc (WV) Doctor of Acupuncture, West Virginia DACBN Diplomate of American Chiropractic Board of Nutrition DACVD Diplomate of the American College of Veterinary Dermatology DC Doctor of Chiropractic DDS Doctor of Dentistry DHANP Diplomate of the Homeopathic Academy of Naturopathic -

Team Physician Consensus Statement
Team Physician Consensus Statement SUMMARY QUALIFICATIONS OF A TEAM PHYSICIAN The objective of the Team Physician Consensus Statement is to provide The primary concern of the team physician is to provide physicians, school administrators, team owners, the general public, and the best medical care for athletes at all levels of participa- individuals who are responsible for making decisions regarding the medical tion. To this end, the following qualifications are necessary care of athletes and teams with guidelines for choosing a qualified team physician and an outline of the duties expected of a team physician. for all team physicians: Ultimately, by educating decision makers about the need for a qualified • Have an M.D. or D.O. in good standing, with an team physician, the goal is to ensure that athletes and teams are provided unrestricted license to practice medicine the very best medical care. • The Consensus Statement was developed by the collaboration of six Possess a fundamental knowledge of emergency care major professional associations concerned about clinical sports medicine regarding sporting events issues: American Academy of Family Physicians, American Academy of • Be trained in CPR Orthopaedic Surgeons, American College of Sports Medicine, American • Have a working knowledge of trauma, musculoskeletal Medical Society for Sports Medicine, American Orthopaedic Society for injuries, and medical conditions affecting the athlete Sports Medicine, and the American Osteopathic Academy of Sports Med- icine. These organizations have committed to forming an ongoing project- In addition, it is desirable for team physicians to have based alliance to “bring together sports medicine organizations to best clinical training/experience and administrative skills in serve active people and athletes.” some or all of the following: • Specialty Board certification EXPERT PANEL • Continuing medical education in sports medicine • Formal training in sports medicine (fellowship train- Stanley A. -

Structuring Physician-Pharmacy Ventures
Presenting a live 90-minute webinar with interactive Q&A Structuring Physician-Pharmacy Ventures: Minimizing Regulatory Risks, Ensuring Reimbursement Navigating Corporate Practice of Medicine/Pharmacy, Anti-Kickback and Stark Laws, and State Regulation WEDNESDAY, MAY 3, 2017 1pm Eastern | 12pm Central | 11am Mountain | 10am Pacific Today’s faculty features: Reesa N. Handelsman, Partner, Wachler & Associates, Royal Oak, Mich. Rick L. Hindmand, Member, McDonald Hopkins, Chicago Todd A. Nova, Shareholder, Hall Render Killian Heath & Lyman, Milwaukee The audio portion of the conference may be accessed via the telephone or by using your computer's speakers. Please refer to the instructions emailed to registrants for additional information. If you have any questions, please contact Customer Service at 1-800-926-7926 ext. 10. Tips for Optimal Quality FOR LIVE EVENT ONLY Sound Quality If you are listening via your computer speakers, please note that the quality of your sound will vary depending on the speed and quality of your internet connection. If the sound quality is not satisfactory, you may listen via the phone: dial 1-866-819-0113 and enter your PIN when prompted. Otherwise, please send us a chat or e-mail [email protected] immediately so we can address the problem. If you dialed in and have any difficulties during the call, press *0 for assistance. Viewing Quality To maximize your screen, press the F11 key on your keyboard. To exit full screen, press the F11 key again. Continuing Education Credits FOR LIVE EVENT ONLY In order for us to process your continuing education credit, you must confirm your participation in this webinar by completing and submitting the Attendance Affirmation/Evaluation after the webinar. -
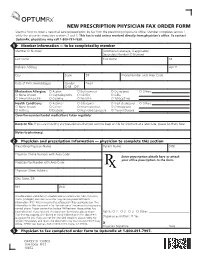
NEW PRESCRIPTION PHYSICIAN FAX ORDER FORM Use This Form to Order a New Mail Service Prescription by Fax from the Prescribing Physician’S Office
NEW PRESCRIPTION PHYSICIAN FAX ORDER FORM Use this form to order a new mail service prescription by fax from the prescribing physician’s office. Member completes section 1, while the physician completes sections 2 and 3. This fax is void unless received directly from physician’s office. To contact OptumRx, physicians may call 1-800-791-7658. 1 Member information — to be completed by member Member ID Number (Additional coverage, if applicable) Secondary Member ID Number Last Name First Name MI Delivery Address Apt. # City State ZIP Phone Number with Area Code Date of Birth (mm/dd/yyyy) Gender Email { M { F Medication Allergies: { Aspirin { Erythromycin { Quinolones { Others: { None known { Cephalosporins { NSAIDs { Sulfa { Amoxil/Ampicillin { Codeine { Penicillin { Tetracyclines Health Conditions: { Asthma { Glaucoma { High cholesterol { Others: { None known { Cancer { Heart condition { Osteoporosis { Arthritis { Diabetes { High blood pressure { Thyroid Disease Over-the-counter/herbal medications taken regularly: Keep on file. If you are including any prescriptions that you want to keep on file for shipment at a later date, please list them here: Notes to pharmacy: 2 Physician and prescription information — physician to complete this section Prescribing Physician Name Patient Name DOB Physician Phone Number with Area Code Enter prescription details here or attach your office prescription to the form. Physician Fax Number with Area Code Physician Street Address City, State, ZIP NPI DEA This document and others if attached contain information from OptumRx that is privileged, confidential and/or may contain protected health information (PHI). We are required to safeguard PHI by applicable law. The information in this document is for the sole use of the person(s) or company named above. -

Changes to the Reimbursement for Physician Pathology, Medicine and Surgical Services with a Professional (26) and Technical (TC) Component
Connecticut Medical Assistance Program Provider Bulletin 2015-62 Policy Transmittal 2015-28 August 2015 Effective Date: September 7, 2015 Roderick L. Bremby, Commissioner Contact: Nina Holmes @ 860-424-5486 TO: Physicians, Physician Assistants, Advanced Practice Registered Nurses, Certified Nurse Midwives, Optometrists, and Podiatrists RE: Changes to the Reimbursement for Physician Pathology, Medicine and Surgical Services with a Professional (26) and Technical (TC) Component This policy transmittal is being sent to notify providers Accessing the Fee Schedules that, effective for dates of service September 7, 2015 Fee schedules can be accessed and downloaded by and forward, the Department of Social Services is going to the Connecticut Medical Assistance Web site: revising the reimbursement for the professional and www.ctdssmap.com. From this Web page, go to technical components of select pathology, medicine “Provider”, then to “Provider Fee Schedule and surgical services to 57.5% of the 2007 Medicare Download”, click on the “I accept” button and then Physician Fee Schedule. The Department is proceed to the “Physician Office and Outpatient Fee implementing this change in order to establish a pricing Schedule” or “Physician Surgical Fee Schedule”. To methodology consistent with Medicare, where, for a access the CSV file, press the control key while given service that includes a professional and technical clicking the CSV link, then select “Open”. component, the fee for the professional component, added together with the fee for the technical For questions about billing or if further assistance is component, equals the global fee. needed to access the fee schedule on the Connecticut Medical Assistance Program Web site, please contact The services impacted include select pathology the HP Provider Assistance Center, Monday through services billed under the LAB rate type off of the Friday from 8:00 a.m.