Child & Adolescent Mental Health Resource Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Best Practice Guides for Behavioral Intervention
Best Practice Guidelines for Behavioral Interventions Developed by PATRICIA BACH, PHD STANLEY G. MCCRACKEN, PHD, LCSW Developed for Behavioral Health Recovery Management Project An Initiative of Fayette Companies, Peoria, IL and Chestnut Health Systems, Bloomington, IL The project is funded by the Illinois Department of Human Services’ Office of Alcoholism and Substance Abuse. Authors: Dr. Bach is a trainer at the University of Chicago Center for Psychiatric Rehabilitation. She received her doctorate in clinical psychology from the University of Nevada, Reno. She has provided mental health services with a behavioral focus to individuals with serious mental illness, substance abuse, and/or developmental disabilities for over 10 years in varied settings. Dr. McCracken is currently Co-Director of Training for the University of Chicago Center for Psychiatric Rehabilitation (CPR) and the Illinois Staff Training Institutes. He holds joint appointments at the University of Chicago as Associate Professor of Clinical Psychiatry and as Senior Lecturer in the School of Social Service Administration. He has conducted research at the CPR and with the University of Chicago Human Behavioral Pharmacology Research Group in a variety of areas, including the influence of mood on drug preference and the effects of training on staff interest and burnout. He has published two books and a number of articles in the areas of psychiatric rehabilitation, chemical dependency, behavioral medicine, staff training, and implementation of evidence based practice. He also is a respected clinician with twenty five years experience providing services to individuals with mental illness, physical illness, and chemical dependence. 1 Behavioral Interventions Several behavioral approaches, when combined with medication, have been shown to reduce symptoms or the impact of symptoms of serious mental illness (Corrigan, 1997). -

Behavioral Health Integration Policy Brief Prepared for the Bipartisan Policy Center Stephanie Gold, MD, Perry Dickinson, MD, Larry Green, MD
Brief 7, April 2020 Behavioral Health Integration Policy Brief Prepared for the Bipartisan Policy Center Stephanie Gold, MD, Perry Dickinson, MD, Larry Green, MD The need for behavioral health integration (BHI): The aim of health care is to help people solve or live with their health-related problems. There are constant and unavoidable interactions of mental, emotional, behavioral and physical problems that require integration of primary care and behavioral health. What is the current landscape of primary care delivery of behavioral health services? • Integrated care is being implemented in practices of all types • Payment and workforce shortages remain significant barriers to scaling implementation of integrated care • More integration in urban, larger practices compared to rural and smaller practices, but rural-urban difference may be mostly explainable by practice size1 o ~ 45% PCPs are co-located with a BH provider (with the rates in urban areas close to twice that of rural areas). No significant change in these numbers 2010 – 2018.2,3 • Some states are more advanced than others. The State Innovation Model (SIM) has been a mechanism for advancing BHI in several states:4 o Practice facilitation and multipayer support for BHI into primary care settings (CO) o Implementation of behavioral health homes (ME, MN) o ACOs requiring or incentivizing BHI (MN, VT, MA) o Inclusion of BH metrics in payment and delivery models (OR, MA, VT, MN, ME) o Invested in technical assistance for BH (OR, ME, MN, VT, MA) How do the delivery of care and challenges -

First Episode Psychosis an Information Guide Revised Edition
First episode psychosis An information guide revised edition Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) i First episode psychosis An information guide Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) A Pan American Health Organization / World Health Organization Collaborating Centre ii Library and Archives Canada Cataloguing in Publication Bromley, Sarah, 1969-, author First episode psychosis : an information guide : a guide for people with psychosis and their families / Sarah Bromley, OT Reg (Ont), Monica Choi, MD, Sabiha Faruqui, MSc (OT). -- Revised edition. Revised edition of: First episode psychosis / Donna Czuchta, Kathryn Ryan. 1999. Includes bibliographical references. Issued in print and electronic formats. ISBN 978-1-77052-595-5 (PRINT).--ISBN 978-1-77052-596-2 (PDF).-- ISBN 978-1-77052-597-9 (HTML).--ISBN 978-1-77052-598-6 (ePUB).-- ISBN 978-1-77114-224-3 (Kindle) 1. Psychoses--Popular works. I. Choi, Monica Arrina, 1978-, author II. Faruqui, Sabiha, 1983-, author III. Centre for Addiction and Mental Health, issuing body IV. Title. RC512.B76 2015 616.89 C2015-901241-4 C2015-901242-2 Printed in Canada Copyright © 1999, 2007, 2015 Centre for Addiction and Mental Health No part of this work may be reproduced or transmitted in any form or by any means electronic or mechanical, including photocopying and recording, or by any information storage and retrieval system without written permission from the publisher—except for a brief quotation (not to exceed 200 words) in a review or professional work. This publication may be available in other formats. For information about alterna- tive formats or other CAMH publications, or to place an order, please contact Sales and Distribution: Toll-free: 1 800 661-1111 Toronto: 416 595-6059 E-mail: [email protected] Online store: http://store.camh.ca Website: www.camh.ca Disponible en français sous le titre : Le premier épisode psychotique : Guide pour les personnes atteintes de psychose et leur famille This guide was produced by CAMH Publications. -

Resource Document on Social Determinants of Health
APA Resource Document Resource Document on Social Determinants of Health Approved by the Joint Reference Committee, June 2020 "The findings, opinions, and conclusions of this report do not necessarily represent the views of the officers, trustees, or all members of the American Psychiatric Association. Views expressed are those of the authors." —APA Operations Manual. Prepared by Ole Thienhaus, MD, MBA (Chair), Laura Halpin, MD, PhD, Kunmi Sobowale, MD, Robert Trestman, PhD, MD Preamble: The relevance of social and structural factors (see Appendix 1) to health, quality of life, and life expectancy has been amply documented and extends to mental health. Pertinent variables include the following (Compton & Shim, 2015): • Discrimination, racism, and social exclusion • Adverse early life experiences • Poor education • Unemployment, underemployment, and job insecurity • Income inequality • Poverty • Neighborhood deprivation • Food insecurity • Poor housing quality and housing instability • Poor access to mental health care All of these variables impede access to care, which is critical to individual health, and the attainment of social equity. These are essential to the pursuit of happiness, described in this country’s founding document as an “inalienable right.” It is from this that our profession derives its duty to address the social determinants of health. A. Overview: Why Social Determinants of Health (SDOH) Matter in Mental Health Social determinants of health describe “the causes of the causes” of poor health: the conditions in which individuals are “born, grow, live, work, and age” that contribute to the development of both physical and psychiatric pathology over the course of one’s life (Sederer, 2016). The World Health Organization defines mental health as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community” (World Health Organization, 2014). -

AOK Early Childhood Network Mental Health Resource Guide 2016
AOK Early Childhood Network Mental Health Resource Guide 2016 Program Name Description of Services Eligibility Locations Contact Information • General youth Ages 3 – Adult ABC Counseling 7820 N. University Phone: counseling Private insurance Adoption & Family • Youth sexual abuse Suite 101 Peoria office (309) 689-2990 Counseling Services DCFS Medicaid Peoria, IL 61614 counseling Pekin office (309) 349-3866 clients • Adoption services Negotiated fee 359 Margaret St. Website: Pekin, IL 61554 www.abccounseling.org Scholarships available for sexual abuse victims • Coaching AEON • Cognitive Behavioral 0 years – Adult 5016 N University Ste Phone: Social Emotional • EMDR 101 (309) 573-4834 Health Insurance accepted Peoria, Illinois 61614 • Family / Marital • Family Systems Sliding scale fee • Interpersonal • Play Therapy • Relational • Solution Focused Brief • • Counseling Ages 3 – Adult • Play, art, & sand 75 E. Queenwood Rd. Phone: Agape therapy Fees based on each Morton, IL 61550 Counseling • Premarital & marital therapist’s degree Morton office (309) 263-5565 counseling and experience • Dialectal behavior 2001 W. Willow Knolls Peoria office (309) 692-4433 • Eye Movement Accepts most major Rd. Desensitization insurances-no Suite 110 Bloomington office Reprocessing (EMDR) Medicaid Peoria, IL 61614 (309) 663-2229 • Group therapy • Sexual recovery Deductibles and co- Hours: groups pay due at time of 211 N. Veterans 9:00am – 5:00pm • Psychological service Parkway assessments Suite 1 Website: • Forensics evaluation Accept sliding scale Bloomington, IL 61704 www.agapecounselors.net fees for certain • Mediation services therapist • Mental health Open to everyone 405 W. John Gwynn Jr. Phone: American Red Cross services Ave. (309) 677-7272 Crisis Counseling • Blood donations Peoria, IL 61605 Website: • Charity services www.redcross.org/il/peoria • Disaster relief • Education services • Child clinic Ages 0 years – Adult 6615 N. -
Spanish Clinical Language and Resource Guide
SPANISH CLINICAL LANGUAGE AND RESOURCE GUIDE The Spanish Clinical Language and Resource Guide has been created to enhance public access to information about mental health services and other human service resources available to Spanish-speaking residents of Hennepin County and the Twin Cities metro area. While every effort is made to ensure the accuracy of the information, we make no guarantees. The inclusion of an organization or service does not imply an endorsement of the organization or service, nor does exclusion imply disapproval. Under no circumstances shall Washburn Center for Children or its employees be liable for any direct, indirect, incidental, special, punitive, or consequential damages which may result in any way from your use of the information included in the Spanish Clinical Language and Resource Guide. Acknowledgements February 2015 In 2012, Washburn Center for Children, Kente Circle, and Centro collaborated on a grant proposal to obtain funding from the Hennepin County Children’s Mental Health Collaborative to help the agencies improve cultural competence in services to various client populations, including Spanish-speaking families. These funds allowed Washburn Center’s existing Spanish-speaking Provider Group to build connections with over 60 bilingual, culturally responsive mental health providers from numerous Twin Cities mental health agencies and private practices. This expanded group, called the Hennepin County Spanish-speaking Provider Consortium, meets six times a year for population-specific trainings, clinical and language peer consultation, and resource sharing. Under the grant, Washburn Center’s Spanish-speaking Provider Group agreed to compile a clinical language guide, meant to capture and expand on our group’s “¿Cómo se dice…?” conversations. -

Interventions Targeting HIV-Infected Risky Drinkers
33.3_9.1.10.qxd:32(1).qxp 9/8/10 11:44 AM Page 267 Interventions Targeting HIVInfected Risky Drinkers Drops in the Bottle Jeffrey H. Samet, M.D., M.A., M.P.H., and Alexander Y. Walley, M.D., M.Sc. Alcohol use is common among people infected with HIV and may contribute to adverse consequences such as reduced adherence to treatment regimens and increased likelihood of risky sexual behaviors. Therefore, researchers and clinicians are looking for treatment approaches to reduce harmful alcohol consumption in this population. However, clinical trials of existing treatment models are scarce. A literature review identified only 11 studies that included HIVinfected patients with past or current risky alcohol use and which targeted alcohol use and other health behaviors. Four studies focusing on HIVinfected participants with alcohol problems found mixed effects on adherence and on alcohol use. Five clinical trials included at least 10 percent of HIVinfected subjects who use alcohol; of these, only one reported significant evidence of a favorable impact on alcohol consumption. Finally, two trials targeting alcohol users at high risk for HIV infection identified treatment effects that were not sustained. Taken together, these findings provide limited evidence of the benefit of behavioral interventions in this population. Nevertheless, these studies give some guidance for future interventions in HIVinfected patients with alcohol problems. KEY WORDS: Alcohol and other drug use; alcohol consumption; alcohol use disorder; human immunodeficiency virus; HIVinfected patients; sexually transmitted disease; unsafe sex; treatment method; treatment outcome; intervention; clinical trial; literature review n the United States, people infected • Lack of a health care provider for the 1 According to the National Institute on Alcohol Abuse and HIV infection (Metsch et al. -

Eating Disorders: About More Than Food
Eating Disorders: About More Than Food Has your urge to eat less or more food spiraled out of control? Are you overly concerned about your outward appearance? If so, you may have an eating disorder. National Institute of Mental Health What are eating disorders? Eating disorders are serious medical illnesses marked by severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may be signs of an eating disorder. These disorders can affect a person’s physical and mental health; in some cases, they can be life-threatening. But eating disorders can be treated. Learning more about them can help you spot the warning signs and seek treatment early. Remember: Eating disorders are not a lifestyle choice. They are biologically-influenced medical illnesses. Who is at risk for eating disorders? Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Although eating disorders often appear during the teen years or young adulthood, they may also develop during childhood or later in life (40 years and older). Remember: People with eating disorders may appear healthy, yet be extremely ill. The exact cause of eating disorders is not fully understood, but research suggests a combination of genetic, biological, behavioral, psychological, and social factors can raise a person’s risk. What are the common types of eating disorders? Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. If you or someone you know experiences the symptoms listed below, it could be a sign of an eating disorder—call a health provider right away for help. -
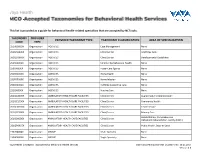
This List Is Provided As a Guide for Behavioral Health-Related Specialties That Are Accepted by Nctracks
This list is provided as a guide for behavioral health-related specialties that are accepted by NCTracks. TAXONOMY PROVIDER PROVIDER TAXONOMY TYPE TAXONOMY CLASSIFICATION AREA OF SPECIALIZATION CODE TYPE 251B00000X Organization AGENCIES Case Management None 261QA0600X Organization AGENCIES Clinic/Center Adult Day Care 261QD1600X Organization AGENCIES Clinic/Center Developmental Disabilities 251S00000X Organization AGENCIES Community/Behavioral Health None 253J00000X Organization AGENCIES Foster Care Agency None 251E00000X Organization AGENCIES Home Health None 251F00000X Organization AGENCIES Home Infusion None 253Z00000X Organization AGENCIES In-Home Supportive Care None 251J00000X Organization AGENCIES Nursing Care None 261QA3000X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Augmentative Communication 261QC1500X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Community Health 261QH0100X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Health Service 261QP2300X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Primary Care Rehabilitation, Comprehensive 261Q00000X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Outpatient Rehabilitation Facility (CORF) 261QP0905X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Public Health, State or Local 193200000X Organization GROUP Multi-Specialty None 193400000X Organization GROUP Single-Specialty None Vaya Health | Accepted Taxonomies for Behavioral Health Services Claims and Reimbursement | Content rev. 10.01.2017 Version -

Eating Disorders
Eating Disorders NDSCS Counseling Services hopes the following information will help you gain a better understanding of eating disorders. If you believe you or someone you know is experiencing related concerns and would like to visit with a counselor, please call NDSCS Counseling Services for an appointment - 701.671.2286. Definition There is a commonly held view that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that cause severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may also signal an eating disorder. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. Signs and Symptoms Anorexia nervosa People with anorexia nervosa may see themselves as overweight, even when they are dangerously underweight. People with anorexia nervosa typically weigh themselves repeatedly, severely restrict the amount of food they eat, and eat very small quantities of only certain foods. Anorexia nervosa has the highest mortality rate of any mental disorder. While many young women and men with this disorder die from complications associated with starvation, others die of suicide. In women, suicide is much more common in those with anorexia than with most other mental disorders. Symptoms include: • Extremely restricted eating • Extreme thinness (emaciation) • A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight • Intense fear of gaining weight • Distorted body image, a self-esteem -

Understanding Mental Health
UNDERSTANDING MENTAL HEALTH WHAT IS MENTAL HEALTH? Our mental health directly influences how we think, feel and act: it also affects our physical health. Work, in fact, is actually one of the best things for protecting our mental health, but it can also adversely affect it. Good mental health and well-being is not an on-off A person’s mental health moves back and forth along this range during experience. We can all have days, weeks or months their lifetime, in response to different stressors and circumstances. At where we feel resilient, strong and optimistic, the green end of the continuum, people are well; showing resilience regardless of events or situations. Often that can and high levels of wellbeing. Moving into the yellow area, people be mixed with or shift to a very different set of may start to have difficulty coping. In the orange area, people have thoughts, feelings and behaviours; or not feeling more difficulty coping and symptoms may increase in severity and resilient and optimistic in just one or two areas of frequency. At the red end of the continuum, people are likely to be our life. For about twenty-five per cent of us, that experiencing severe symptoms and may be at risk of self-harm or may shift to having a significant impact on how suicide. we think, feel and act in many parts of our lives, including relationships, experiences at work, sense of connection to peer groups and our personal sense of worth, physical health and motivation. This could lead to us developing a mental health condition such as anxiety, depression, substance misuse. -

Columbia University School of Nursing
Psychiatric Care: What America Can Learn from Jamaican Practices Gabrielle Ranger-Murdock, MSN, RN, Andrea McDade, MSN, RN Columbia University School of Nursing Introduction & Purpose Where are Psychiatric Patients Being Treated? Mental health disorders continue to be a leading cause of disability in the United States. United States Jamaica Thus, the improvement of psychiatric care is imperative. An immersive experience in the Jamaican psychiatric system incited research to compare and contrast mental health care in both countries. • Where is America lacking in psychiatric care? ▹ Continuing difficulty with patient autonomy and community based treatment following discharge ▹ Deinstitutionalization has failed to provide adequate access to patient-centered mental healthcare8 ▹ High mental health care expenditures that include correctional services funding5 • What has Jamaica done differently? ▹ Collectivist values to promote patient centered care ▹ Community mental healthcare has expanded access, expenditures have been reduced, and inpatient hospital stays are shorter5 How can we use global perspectives to guide improvement to patient centered care in the US mental health system? Conclusions & Future Directions Mental Healthcare Facilities Collectivist values promote holistic support of psychiatric patients, as well as community reintegration. Investing in this integration, educating communities on severe mental illness, and Jamaica promoting family-centered care contributes to improved patient outcomes and reduces need United States for