Progressive Visual Loss in Adults with Retinopathy of Prematurity (Rop)*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ASOPRS 2015 New Members
ASOPRS 2015 New MeMbeRS Imtiaz A. Chaudhry, MD, PhD, brett Davies, MD FACS LOCATION: San Antonio, TX LOCATION: Houston, TX Company/InstituTION: United States Company/InstituTION: Houston Air Force Oculoplastics Associates uNDergrADuate: BA, Harding University, TITLe: Physician Searcy, AR uNDergrADuate: Weber University, Salt Lake City, UT Medical SChool: Uniformed Services University, Bethesda, MD Medical SChool: Yale Medical School, Salt Lake City, UT reSIDeNCy: San Antonio Uniformed Services Health Education Consortium, San Antonio, TX reSIDeNCy: Yale Medical School, CT FeLLOwShIP: Vikram D. Durairaj, MD, University of Colorado, FeLLOwShIP: Baylor College of Medicine, Houston, TX Denver, CO OTher MeMberShIP SocieTIeS: American Academy of Craig Czyz, DO Ophthalmology, Society of Military Ophthalmologists, Association for Research in Vision and Ophthalmology, LOCATION: Columbus, OH Society of Air Force Clinical Surgeons, Christian Medical and Dental Association Company/InstituTION: Ohio University NotabLe AChIeveMeNTS: Beat Vik in 1 on 1 basketball TITLe: Chair, Division of Ophthalmology, Section Head, Oculofacial Plastic & My wife Stacy and I have been married since 1999. We have Reconstructive Surgery three kids — Sidney, Caleb, and Tyler. I am currently deployed to Afghanistan, but look forward to getting home to my family UndergrADuate: Wake Forest University, Winston-Salem, NC in San Antonio soon. We enjoy getting outside as much as Medical SChool: Philadelphia College of Osteopathic Medicine, possible — swimming, hiking, and riding -
MEMORIAL RESOLUTION for WILLIAM TASMAN, MD 1 2 Introduced By
1 MEMORIAL RESOLUTION FOR WILLIAM TASMAN, MD 2 3 Introduced by: Cadence A. Kim, MD, FACS on behalf of the Philadelphia County Medical Society 4 Author: Cadence A. Kim, MD, FACS 5 6 WHEREAS, William Tasman, MD, passed away on March 28, 2017 at his Chestnut Hill home in 7 Philadelphia, PA at the age of 88; and 8 9 WHEREAS, Dr. Tasman graduated from Temple University School of Medicine; completed a residency in 10 Ophthalmology at the Wills Eye Hospital; completed a Retina fellowship at the Massachusetts Eye and 11 Ear Infirmary before returning to Philadelphia and Wills Eye Hospital to begin his tenure; and 12 13 WHEREAS, Dr. Tasman was an active member of the Philadelphia County Medical Society (PCMS) and 14 the Pennsylvania Medical Society (PAMED) for 58 years; was a Fellow in the American College of 15 Surgeons; contributed to many key organizations with leadership as Ophthalmologist-in-Chief of Wills 16 Eye Hospital; served as Professor and Chair of Ophthalmology at Jefferson Medical College of Thomas 17 Jefferson University; was the Founder of Mid-Atlantic Retina; served as President of the American 18 Academy of Ophthalmology and Chair of the American Board of Ophthalmology as well as President of 19 the American Ophthalmological Society; and was a founding member and President of the Retina 20 Society; and 21 22 WHEREAS, Dr. Tasman, whose almost 300 studies in peer-reviewed literature and 64 book chapter 23 contributions spanned the field of retina, notably retinal detachment and diabetic retinopathy; and 24 whose most transformational work was in pediatric retina and specifically, retinopathy of prematurity; 25 and 26 27 WHEREAS, Dr. -
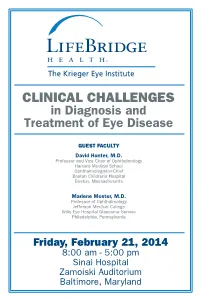
CLINICAL CHALLENGES in Diagnosis and Treatment of Eye Disease
CLINICAL CHALLENGES in Diagnosis and Treatment of Eye Disease GUEST FACULTY David Hunter, M.D. Professor and Vice Chair of Ophthalmology Harvard Medical School Ophthalmologist-in-Chief Boston Children’s Hospital Boston, Massachusetts Marlene Moster, M.D. Professor of Ophthalmology Jefferson Medical College Wills Eye Hospital Glaucoma Service Philadelphia, Pennsylvania Friday, February 21, 2014 8:00 am - 5:00 pm Sinai Hospital Zamoiski Auditorium Baltimore, Maryland CLINICAL CHALLENGES in Diagnosis and Treatment of Eye Disease Date, Time & Location Date: Friday, February 21, 2014 Time: 8:00 am - 5:00 pm Location: Sinai Hospital of Baltimore - Zamoiski Auditorium 2401 West Belvedere Avenue Baltimore, Maryland 21215 Phone (410) 601-6200 Registration / Information Registration Fee: $95 Residents and Fellows: No charge Includes all program materials, continental breakfast, luncheon and refreshments. Advance registration is required. Please make checks payable to: The Krieger Eye Institute CME Program. Registration must be received no later than February 14, 2014. Program Coordinator: Wendy Schnitzer (410) 601-5931 Free Parking (with validation) is available in the new Belvedere Avenue parking garage directly in front of Zamoiski Auditorium. Accreditation LifeBridge Health is accredited by MedChi, the Maryland State Medical Society, to sponsor continuing medical education for physicians. LifeBridge Health designates this educational activity for a maximum of 7.0 AMA PRA Category 1 Credit(s)TM. Physicians should only claim credit commensurate with the extent of their participation in the activity. The Maryland Board of Optometry has designated this educational activity for 7.0 TPA credit hours (Approval code 2014-023 PS). This program has been awarded 7.0 Group B JCAHPO (Joint Commission on Allied Health Personnel in Ophthalmology) continuing education credits (CECs) Conference Objectives Participants will be exposed to new strategies in the diagnosis and management of uveitis, glaucoma, cataracts, corneal disease, retinal pathology and pediatric disease. -

The Foundation of the American Academy of Ophthalmology Museum of Vision & Ophthalmic Heritage Conversation Between Paul
The Foundation of the American Academy of Ophthalmology Museum of Vision & Ophthalmic Heritage Conversation Between Paul Lichter, MD and William Tasman, MD In Partnership with StoryCorps, San Francisco CA, October 24, 2009 Drs. Paul Lichter and William Tasman recorded this conversation on October 24, 2009 during the Annual Meeting of the American Academy of Ophthalmology, in San Francisco CA. Dr. Lichter is a glaucoma specialist from Michigan and Dr. Tasman is a retina specialist living in Pennsylvania. You are invited now to listen to excerpts and read the complete transcript below. Here Dr. Lichter describes his first glaucoma patient. In this excerpt Dr. Tasman describes his time working with Gerd Meyer-Schwickerath, MD and photo coagulation. The Foundation of the American Academy of Ophthalmology Museum of Vision & Ophthalmic Heritage Conversation Between Paul Lichter, MD and William Tasman, MD In Partnership with StoryCorps, San Francisco CA, October 24, 2009 DR. PAUL LICHTER: I’m Paul Lichter. I’m 70 years old. It’s October 24th, 2009. We’re in San Francisco, California, and I’m talking to Bill Tasman, who has been a long-time friend and colleague and fellow department chair for many, many years, and fellow officer of the American Academy of Ophthalmology in the past, and we’re here to have a conversation. DR. BILL TASMAN: I’m Bill Tasman. I wish I was a kid like Dr. Lichter. I’m 80. Today’s date is October 24th, 2009. We’re in San Francisco, and my relationship with Dr. Lichter is friend and colleague. As he just said, we have served together on the American Academy of Ophthalmology Board, the American Board of Ophthalmology and the AOS. -

In Memoriam: William Tasman, MD (1929-2017)
OBITUARY In Memoriam: William Tasman, MD (1929-2017) Julia A. Haller, MD illiam Tasman, MD, whose tall distinguished fig- Dr Tasman was a recipient of many of our specialty’s ure cast a physical and metaphorical shadow highest honors, including the Wills Eye Hospital Alumni W across global ophthalmology, died peacefully at Society’s Silver Tray Award, the College of Physicians of his Chestnut Hill home in Philadelphia, Pennsylvania, sur- Philadelphia’s Zentmayer Award, the American Academy of rounded by his family on March 28. He had fought back cou- Ophthalmology’s Lifetime Achievement Award, the Stritt- rageously from a fall that broke his hip some weeks earlier but matter Award of the Philadelphia County Medical Society, ultimately died of congestive heart failure. It was the only time the Marshall Parks Award of the American Association for his great heart ever failed him. Pediatric Ophthalmology and Strabismus, the Lucien Howe His loyalties ran deep. A Philadelphia gentleman, he Medal of the American Oph- graduated from Germantown Friends School, Haverford Col- thalmological Society, the lege (where he played single-wing football), and Temple Uni- Gold Medal of the Kingdom versity School of Medicine. He served his country as a of Saudi Arabia, the Heed captain in the 7100th US Air Force Hospital in Wiesbaden, Award, and the Charles Germany, before returning to complete his residency in oph- Schepens Award of the thalmology at the Wills Eye Hospital. Following residency, Retina Society. His remark- he pursued a retina fellowship at the Massachusetts Eye and able career continued active Ear Infirmary, Boston, returning to Philadelphia and Wills to the very end. -

Retina Times
RETINA TIMESThe Official Publication of the American Society of Retina Specialists Fall 2012 Issue 46 46 RETINA TIMES <Wbb(&'(?iik[*, Organizational Staff Jeffrey S. Heier, MD Clinical Trials: Future Pathways Section Editor Lebkc[)&"DkcX[h* J. Michael Jumper, MD Boston, MA Retina Times (ISSN 2164-4411) is published 5 times a year Editor-in-Chief Suber S. Huang, MD, MBA by the American Society of Retina Specialists (ASRS) San Francisco, CA [email protected] President, Foundation of the ASRS as a service to its membership. Cleveland, OH Susan Raef, MSMC Managing Editor G. Baker Hubbard, III, MD The mission of the publication is to strive to be the definitive Chicago, IL Pediatric Retina Section Co-Editor information source for ASRS members on Society news, [email protected] Atlanta, GA meeting plans, socioeconomic topics, international news, and Ana Schedler J. Michael Jumper, MD other relevant information on issues, instruments, and study Graphic Designer PAT Survey Section Editor San Francisco, CA updates for the practicing retinal specialist. Toby Zallman Production Artist Peter K. Kaiser, MD Schedler Brennan Design + Consulting ASRS-AAO Councilor Representative Articles published herein are reviewed by the editor-in-chief Chicago, IL Cleveland, OH and managing editor for editorial content only. The accuracy Oonagh Petrizzi Stacy Kiff of information contained is the responsibility of the individual Proofreader Annual Meeting Section Editor author. Letters and other unsolicited material are assumed to be Stamford, CT Chicago, IL intended for publication and are subject to rejection or editing. John T. Thompson, MD William T. Koch, COA, COE, CPC ASRS President Coding Pitfalls Section Editor Baltimore, MD St. -

The Sesquicentennial of the American Ophthalmological Society
YEARS The Sesquicentennial of the American Ophthalmological Society The Sesquicentennial of the American Ophthalmological Society OUR MISSION CONTINUES Daniel M. Albert, MD, MS, and Sarah L. Atzen, MA Editor of Photography Ralph C. Eagle, Jr., MD THE AMERICAN OPHTHALMOLOGICAL SOCIETY San Francisco © 2014 American Ophthalmological Society All rights reserved. No part of this publication may be reproduced in any form without written permission from the copyright owner. First edition published 2014. Printed in the United States of America. 10 9 8 7 6 5 4 3 2 1 This book is dedicated to Charles “Pat” Wilkinson, MD, 17th Secretary-Treasurer, and Thomas J. Liesegang, MD, Dr. Wilkinson’s successor and the first Executive Vice President of the American Ophthalmological Society Table of Contents 1 The First 125 Years: 1864–1989 ................................1 What’s Past Is Prologue: The Sesquicentennial of the American Ophthalmological Society ............................1 The American Ophthalmological Society: The First 125 Years, by Frank W. Newell ���������������������������������������������������4 2 Vision and Mission of the AOS and the Challenges They Present ...............................................15 3 Accomplishments of the AOS 1989–2014 ......................17 The Ophthalmologist of the Future................................17 Continuing a 150-Year Tradition .................................19 The Most Cited Papers of the Transactions of the Society.............20 Table 1. Top Ten Most-Cited Papers, Sorted by Year (1990–2013).....20 -

Transactions of the American Ophthalmological Society Volume CXV
Transactions of the American Ophthalmological Society Volume CXV One Hundred and Fifty-Third Annual Meeting The Homestead Hot Springs, Virginia 2017 Published for the American Ophthalmological Society San Francisco, California 2017 TABLE OF CONTENTS THE AMERICAN OPHTHALMOLOGICAL SOCIETY 2017 OFFICERS AND COUNCIL vi PRESIDENTS OF THE SOCIETY vii RECIPIENTS OF THE LUCIEN HOWE MEDAL x FREDERICK H. VERHOEFF LECTURERS xii BLODI LECTURERS xiii MEMBERS xiv EDITORIAL BOARD xvii NECROLOGY IN MEMORIUM Necrology 1 MINUTES OF THE PROCEEDINGS INTRODUCTION Proceedings 1 PAPERS: FRIDAY, MAY 20 1 EXECUTIVE SESSION 1 REPORT OF THE EXECUTIVE VICE-PRESIDENT 1 REPORT OF THE CHAIR OF THE COUNCIL 2 REPORT OF THE AUDIT COMMITTEE 2 REPORT OF THE COMMITTEE ON THESES 3 REPORT OF THE EDITOR 3 REPORT OF THE COMMITTEE ON PROGRAMS 4 REPORT OF THE COMMITTEE ON MEMBERSHIP 4 REPORT OF THE ARCHIVIST / PHOTOGRAPHER 5 REPORT OF THE REPRESENTATIVE TO THE COUNCIL OF THE AMERICAN ACADEMY OF 7 OPHTHALMOLOGY REPORT OF THE REPRESENTATIVE TO THE AMERICAN COLLEGE OF SURGEONS 8 REPORT OF THE REPRESENTATIVES TO THE AMERICAN ORTHOPTIC COUNCIL 9 PAPERS: SATURDAY, MAY 21 12 BANQUET 12 REPORT OF THE COMMITTEE ON ATHLETICS 15 PAPERS: SUNDAY, MAY 22 18 MEMBERS IN ATTENDANCE 19 PAPER ABSTRACTS 21 IMPACT OF RESIDENT AND FELLOW TRAINEES ON PATIENT ENCOUNTER LENGTH IN AN ACADEMIC OPHTHALMOLOGY CENTER MICHAEL CHIANG, ISAAC GOLDSTEIN, SARAH READ-BROWN, MICHELLE HRIBAR GENETIC ANALYSIS OF 1000 CONSECUTIVELY ASCERTAINED FAMILIES WITH INHERITED RETINAL DISEASE EDWIN STONE, JEANEEN ANDORF, ADAM DELUCA, SCOTT WHITMORE, JOSEPH GIACALONE, LUAN STREB, TERRY BRAUN, ROBERT MULLINS, TODD SCHEETZ, VAL SHEFFIELD, BUDD TUCKER CONJUNCTIVAL TUMORS IN CHILDREN IN 806 CASES. -

Number 2 2011-02 OPS Second Quarter Newsletter with LARGE
Vol. 41 No. 2 Second Quarter 2011 Volume 41■Issue2 Second Quarter 2011 www.opsweb.org Ophthalmic Photographers’ Society 1887 West Ranch Road Nixa, MO 65714-8262 Inside this Issue USA Tel: 800-403-1677 International Tel: 01-417-725-0181 Email: [email protected] Call for Orlando Speakers 4 Executive Director Editor’s Thoughts 4 Barbara McCalley The President’s Niche 5 Newsletter Editor William Anderson, CRA, FOPS OPS Exhibit at ASCRS 6 [email protected] Your Membership 6 President: OPS Paula Morris, CRA, FOPS Johnny Justice Jr. Scholarship Award 7 [email protected] ICOP 2011 7 Chair: Board of Certification Beth Ann Benetz, CRA, FOPS New Course for Annual Program 8 [email protected] 2011 Annual Program Team Members 9 Chair: Board of Education Kirsten G. Locke, CRA, FOPS Donald Gass Memorial Lecture 10 [email protected] Preview of the 2011 Annual Timeline 11 Advertising : Barbara McCalley Tips, Tricks & Techniques 12 Career Opportunities 13 2011 Newsletter Deadlines BOE Survey Results 14 First Quarter Jan 14, 2011 Second Quarter Apr 1, 2011 Third Quarter Jul 1, 2011 Fourth Quarter Sep 9, 2011 Cover Photo: Kasi Sandhanam “Pinpoint Posterior Synechia”. 2 Newsletter/Membership Membership Historical Archives: The archives began over 20 years If you are not an OPS member and ago as a legacy project by one of the OPS founding fathers, Mr. would like to join, select "New Member- Don Wong. The archives represent a permanent collection of ship" on the OPS web page under newsletters, programs, board minutes and photos going back to membership. You will first be asked to 1969. -

J-A10023-17 2017 PA Super 380 RETINA ASSOCIATES of GREATER PHILADELPHIA
J-A10023-17 2017 PA Super 380 RETINA ASSOCIATES OF GREATER IN THE SUPERIOR COURT OF PHILADELPHIA, LTD., JONATHAN B. PENNSYLVANIA BELMONT, M.D., ROBERT C. KLEINER, M.D. Appellant v. RETINOVITREOUS ASSOCIATES, LTD. D/B/A MID ATLANTIC RETINA, WILLIAM BENSON, M.D., JAY L. FEDERMAN, M.D., GARY C. BROWN, M.D., MITCHELL S. FINEMAN, M.D., DAVID H. FISCHER, M.D., SUNIR J. GARG, M.D., ALLEN C. HO, M.D., RICHARD KAISER, M.D., ALFRED C. LUCIER, M.D., JOSEPH I. MAGUIRE, M.D., J. ARCH MCNAMARA, M.D., CARL H. PARK, M.D., CARL D. REGILLO, M.D., ARUNAN SIVALINGAM, M.D., WILLIAM TASMAN, M.D., JAMES F. VANDER, M.D., AND JASON HSU, M.D. No. 3265 EDA 2016 Appeal from the Order Dated July 2, 2010 In the Court of Common Pleas of Montgomery County Civil Division at No(s): 09-32182 BEFORE: DUBOW, J., SOLANO, J., and FORD ELLIOTT, P.J.E. OPINION BY SOLANO, J.: FILED DECEMBER 07, 2017 Appellants Retina Associates of Greater Philadelphia, Ltd. (“Retina”), and two of its physicians — its President, Jonathan B. Belmont, M.D. and Vice President, Robert C. Kleiner, M.D. (together, “Retina Physicians”) — appeal from the order sustaining preliminary objections in the nature of a demurrer filed by Appellees William Benson, M.D., Jay L. Federman, M.D., J-A10023-17 Gary C. Brown, M.D., Mitchell S. Fineman, M.D., David H. Fischer, M.D., Sunir J. Garg, M.D., Allen C. Ho, M.D., Richard Kaiser, M.D., Alfred C. Lucier, M.D., Joseph I. -

Academic Calendar
ACADEMIC CALENDAR 2020Programs for Ophthalmologists, Residents, Fellows, and Allied Health Professionals 2021 JULIA A. HALLER, MD Changing the world for the better is our goal every day at Wills Eye Hospital. We are inspired to emulate Ophthalmologist-in-Chief great educators and leaders like King and Mandela, seeking to discover and impart knowledge, and moreover to simplify and transmute that raw material by some special Wills alchemy into wisdom. Lofty goals, even in the best of times, and this 2020 “Year of the Eye” have already given us many challenges. We are proud of the way our medical education program has risen to them all! Many of our didactic offerings have been and will continue to be converted to virtual, and we are pleased to find our widely broadcast webinars, rounds and symposia finding larger and more diverse global audiences. The Wills Eye Hospital 2020-2021 Academic Calendar features an exciting lineup of topics and formats, all targeted towards practical clinical updates for those committed to cutting-edge eye care. This year, we add to our offerings a simulated surgical training curriculum from our new state-of-the-art William Maul Measey Ophthalmic Surgical Training (MOST) Laboratory, and launch a video-based Wills Eye Surgical Library featuring our renowned surgeons tackling a panoply of procedures from the basic to the most novel and complex, highlighting targeted learnings for both trainees and experienced physicians. We look forward to joining you in new and innovative ways as we kick off the 188th year in which Wills Eye Hospital has partnered with you and with generations of eye physicians and surgeons to change the world. -
2010 a N N U a L R E P O R T Cecil Rix, Phd
RETINA RESEARCH FOUNDATION 2010 a n n u a l r e p o r t Cecil Rix, PhD Emmett Humble and Jacquelyn Royce Alice McPherson, MD, and Shara Fryer James Key, MD, and Arthur Willis, MD Cecil Rix, PhD, Bernard Hicks, MD, and Ben Orman, MD Retina Research Foundation Annual Report 2010 Table of Contents Chairman Emeritus Message ................................................................................. 1 Overview of Research ........................................................................................2 - 3 Collaborating Organizations ..............................................................................4 - 5 Named and Basic Research Projects ................................................................6 - 10 Grant Recipient From the Macula Society ............................................................ 11 Established Research Awards .........................................................................11 - 13 Research Chairs and Professorships ..............................................................14 - 16 International Fellowships ......................................................................................17 Research Initiatives and Special Recognition Awards ...................................18 - 19 Financial Summary ........................................................................................20 - 21 Officers and Boards ........................................................................................22 - 23 Contributors ...................................................................................................24