Magnetic Resonance Urethrography Versus Conventional Retrograde Urethrography in the Evaluation of Urethral Stricture: Comparison with Surgical findings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RUG Vs MR Urethrography 3
“COMPARATIVE STUDY BETWEEN RETROGRADE URETHROGRAPHY AND MAGNETIC RESONANCE URETHROGRAPHY IN EVALUATING MALE URETHRAL STRICTURE DISEASE” Dissertation submitted for partial fulfilment of requirements of M.Ch DEGREE EXAMINATION BRANCH 1V – UROLOGY KILPAUK MEDICAL COLLEGE & HOSPITAL CHENNAI – 600 010 THE TAMIL NADU DR.M.G.R MEDICAL UNIVERSITY CHENNAI – 600 032 AUGUST-2013 CERTIFICATE This is to certify that Dr.R.Sukumar has been a post graduate student during the period August 2010 to July 2013 at Department of Urology, Govt Kilpauk Medical College, & Hospital, Chennai. This Dissertation titled “COMPARATIVE STUDY BETWEEN RETROGRADE URETHROGRAPHY AND MAGNETIC RESONANCE URETHROGRAPHY IN EVALUATING MALE URETHRAL STRICTURE DISEASE” is a bonafide work done by him during the study period and is being submitted to the Tamilnadu Dr. M.G.R. Medical University in a partial fulfilment of the MCh Branch IV Urology Examination. Prof.C.Ilamparuthi,M.S,MCh,DNB Prof.P.Vairavel,D.G.O,M.S,MCh, Professor & Head of the Department, Department of Urology,Govt.Royappettah Hospital Govt Kilpauk Medical College Department of Urology, Govt Kilpauk Medical College & Chennai - 600 010. Hospital Chennai - 600 010. Prof.P.Ramakrishnan, MD,DLO Dean Govt Kilpauk Medical College & Hospital Chennai - 600 010 CERTIFICATE This is to certify that Dr.R.Sukumar has been a post graduate student during the period August 2010 to July 2013 at Department of Urology, Govt Kilpauk Medical College, & Hospital, Chennai. This Dissertation titled “COMPARATIVE STUDY BETWEEN RETROGRADE URETHROGRAPHY AND MAGNETIC RESONANCE URETHROGRAPHY IN EVALUATING MALE URETHRAL STRICTURE DISEASE” is a bonafide work done by him during the study period under my guidance. -

ACR–SPR Practice Parameter for the Performance of Voiding
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2019 (Resolution 10)* ACR–SPR PRACTICE PARAMETER FOR THE PERFORMANCE OF FLUOROSCOPIC AND SONOGRAPHIC VOIDING CYSTOURETHROGRAPHY IN CHILDREN PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

12.1 Radiology
12.1 Radiology Southwest Medical Associates (SMA) provides radiology services at multiple locations. The facility located at 888 S. Rancho Drive offers extended hours for urgent situations. SMA offers additional facilities, which operate during normal business hours (please call the individual facility for office hours). Special radiology studies such as CT, Ultrasound, Fluoroscopy, and IVP’s require appointments. Appointments can be made by contacting the scheduling department at (702) 877-5390. Plain film studies do not require a referral or an appointment; however, they do require an order signed by a physician. Contact the Radiology Department at (702) 877-5125 option 5 with any questions. NAME/LOCATION PHONE HOURS PROCEDURES Rancho/Charleston (702) 877-5125 S-S 24 hours Scheduled procedures 888 S. Rancho Dr. 24 hours for emergencies STAT, Expedited Ultrasounds, CT Scans Diagnostic Mammography DEXA Scans N. Tenaya Satellite (702) 243-8500 S-S 7 a.m. - 7 p.m. Plain film studies 2704 N. Tenaya Way Screening Mammography Routine Ultrasounds Routine CT Scans S. Eastern Satellite (702) 737-1880 S-S 7 a.m. - 7 p.m. Plain film studies 4475 S. Eastern Ave. Screening Mammography DEXA Scans Routine Ultrasounds STAT, Expedited, Routine CT Scans Siena Heights Satellite (702) 617-1227 S-S 7 a.m. – 7 p.m. Plain film studies 2845 Siena Heights Screening Mammography Routine Ultrasounds Montecito Satellite (702) 750-7424 S-S 7 a.m. – 7 p.m. Plain Film Studies 7061 Grand Montecito Pkwy Routine Ultrasounds Sunrise Satellite (702) 459-7424 M-F 8 a.m. - 5 p.m. Plain film studies 540 N. -

Multimodality Imaging of the Male Urethra: Trauma, Infection, Neoplasm, and Common Surgical Repairs
Abdominal Radiology (2019) 44:3935–3949 https://doi.org/10.1007/s00261-019-02127-8 SPECIAL SECTION: UROTHELIAL DISEASE Multimodality imaging of the male urethra: trauma, infection, neoplasm, and common surgical repairs David D. Childs1 · Ray B. Dyer1 · Brenda Holbert1 · Ryan Terlecki2 · Jyoti Dee Chouhan2 · Jao Ou1 Published online: 22 August 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Objective The aim of this article is to describe the indications and proper technique for RUG and MRI, their respective image fndings in various disease states, and the common surgical techniques and imaging strategies employed for stricture correction. Results Because of its length and passage through numerous anatomic structures, the adult male urethra can undergo a wide array of acquired maladies, including traumatic injury, infection, and neoplasm. For the urologist, imaging plays a crucial role in the diagnosis of these conditions, as well as complications such as stricture and fstula formation. While retrograde urethrography (RUG) and voiding cystourethrography (VCUG) have traditionally been the cornerstone of urethral imag- ing, MRI has become a useful adjunct particularly for the staging of suspected urethral neoplasm, visualization of complex posterior urethral fstulas, and problem solving for indeterminate fndings at RUG. Conclusions Familiarity with common urethral pathology, as well as its appearance on conventional urethrography and MRI, is crucial for the radiologist in order to guide the treating urologist in patient management. Keywords Urethra · Retrograde urethrography · Magnetic resonance imaging · Stricture Introduction respectively. While the urethral mucosa is well depicted with these radiographic examinations, the periurethral soft tis- Medical imaging plays a crucial role in the diagnosis, treat- sues are not. -

Retrograde Urethrogram/ RUG
Patient Exam Preparation Instructions: Retrograde Urethrogram/ RUG We look forward to seeing you for your appointment. Bring relevant studies Please follow these instructions: and reports to your appointment • Arrive at least 15 minutes prior to your test. University Radiology is able to obtain electronic images and reports for you • This test takes images of your urethra while it is filling with contrast. if the previous studies were performed at our imaging centers or at one of our affiliated hospitals located across • A small urinary catheter will be partially inserted into the tip of your New Jersey. Please visit our website for penis. A small balloon which is located at the tip of the catheter will a full listing: UniversityRadiology.com be inflated. This ensures the catheter stays in place during the exam. Bring your prescription, • The radiologist will then instill contrast through the catheter to outline insurance card, and your urethra during which time x-rays will be taken. photo ID They are required for this procedure. • The catheter will be removed at the end of the exam. Glucose Monitoring Devices Devices such as the ‘FreeStyle Libre’ must be removed before any MRI, CT scan, PET/CT scan, Mammogram, DEXA, or X-ray. The exposure may damage the device and cause incorrect readings. Payment You will be expected to pay your estimated co-payment, co-insurance and/or deductible at the time of your appointment. Call your insurance provider if you have questions about your plan or coverage. Questions? Call 800-758-5545 URG0455 07/26/21 V4. -

Posterior Urethral Disruption in 12 Year Old Boy with Late Urethroplasty After
CaSe report posterior urethral disruption in 12 year old boy with late urethroplasty after multi-organ injury Michał wolnicki, wiesław urbanowicz, Janusz Sulisławski Department of Pediatric, Urology Collegium Medicum, Jagiellonian University, Cracow, Poland key wordS Probability of urethral disruption. On the day of admission, the patient was operated on: wound suture, colostomy, fracture reduc- prostate urethral disruption » children » urethral tions. Suprapubic cystostomy intubation was performed. In the first reconstruction » strictures days after admission, the patient was in a critical condition with blood loss. X Ray investigations revealed: VCUG (voiding cystoure- abStraCt throgram) with contrast feeding by cystostomy and moreover cys- toscopy which confirmed complete disruption of urethra. Function Management of posterior urethral disruption in children of anal sphincter was preserved. Colostomy was closed in January with multiorganic injuries can be quite challenging. 2007. In May 2007, after 6 months, an anastomotic urethral realign- We report the case of a 12 year old male with urethral ment was planned. Before surgery, by additional RUG/VCUG /retro- disruption. We present our experience of the staged grade urethrogram and voiding cystourethrogram/, were confirmed treatment of this patient with delayed anastomotic complete lack of urethral continuity, site and length more than 2 cm urethroplasty after traumatic posterior urethral disrup- between ends of the disrupted urethra (Fig. 1). Access was perineal tion. The patient suffered from a motor vehicle accident to bulbar and posterior urethra. First was performed catheteriza- and sustained multiple organic injures. We performed tion of the anterior urethra, and after catheterization by dilatators late realignment of the urethra 6 months after the through vesica colli to prostatic urethra. -

Uroradiology Tutorial for Medical Students Lesson 3: Cystography & Urethrography – Part 1
Uroradiology Tutorial For Medical Students Lesson 3: Cystography & Urethrography – Part 1 American Urological Association Introduction • Conventional radiography of the urinary tract includes several diagnostic studies: – Cystogram – Retrograde urethrogram – Voiding cystourethrogram • All of these studies answer questions that are essential to urologic patient management Voiding Cystourethrogram (VCUG) • The voiding cystourethrogram is a dynamic test used to define the anatomy and, in part, the function of the lower urinary tract. It is performed by placing a catheter through the urethra into the bladder, filling the bladder with contrast material and then taking x-rays while the patient voids. You can imagine how popular it is among children. Scout Film • Several films are taken when performing a VCUG. The first image is a KUB called the scout film. On this film one can evaluate the bones of the spine and pelvis (injury or congenital anomaly such as spina bifida) and the soft tissues (calcifications, foreign bodies, etc.). • Normal scout image • What gender? Scout Film • Patients with urologic problems (urine infection or incontinence) may have a spinal abnormality that results in abnormal innervation of the bladder. Such anomalies are commonly associated with anomalies of the vertebral column. Let’s look at some spines. • Here is a spine from a normal KUB or scout film. Notice that the posterior processes of all the vertebrae are intact. You can see the posterior process behind and below each vertebral body. • Here is another scout film. Notice that the posterior processes are absent below L-4. This patient has lower lumbar spina bifida. Read This Scout Film • The bones are normal • What about soft tissues (bowel, etc.)? • This child has significant constipation. -

Role of Magnetic Resonance Urethrography in Evaluation of Male Urethral Stricture Against Conventional Retrograde Urethrography
Review Article Clinician’s corner Images in Medicine Experimental Research Case Report Miscellaneous Letter to Editor DOI: 10.7860/JCDR/2018/26988.11648 Original Article Postgraduate Education Role of Magnetic Resonance Case Series Urethrography in Evaluation of Male Radiology Section Urethral Stricture Against Conventional Short Communication Retrograde Urethrography VIJAYA KARTHIKEYAN MURUGESAN1, PADHMINI BALASUBRAMANIAN2 ABSTRACT with surgical findings than RUG in strictures less than 3 cm Introduction: Magnetic Resonance Urethrography (MRU) is a and the RUG showed better correlation with surgical findings new and less widely used technique in the evaluation of male than MRU in strictures longer than 3 cm, even though there urethral strictures. was no significant statistical difference between the two. Stricture lengths in four cases of long penile urethral strictures Aim: This study intends to establish the role of MRU in the with submeatal extension were underestimated by MRU. evaluation of male urethral strictures and to compare the efficacy RUG overestimated the length of four cases of penile urethral with that of conventional Retrograde Urethrography (RUG). stricture. Both RUG and MRU slightly overestimated the severity Materials and Methods: A total of 32 patients with symptoms of strictures in the 2 to 4 mm diameter range. RUG detected all of poor urinary stream and straining during micturition underwent the false tracts, whereas MRU failed to detect one of the false conventional RUG followed by MRU. The parameters studied by tracts. Accuracy in the detection of spongiofibrosis in MRU was RUG and MRU such as stricture site, number, length, diameter directly proportional to the severity, with no false negatives in and associated false tracts or diverticulum were compared with moderate to severe degrees of spongiofibrosis. -
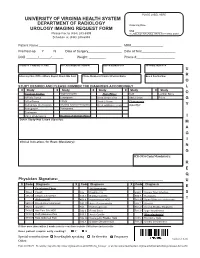
030371 Urologyimagingrequest
PLACE LABEL HERE UNIVERSITY OF VIRGINIA HEALTH SYSTEM DEPARTMENT OF RADIOLOGY Ordering Date____________ UROLOGY IMAGING REQUEST FORM SS# ____________________ Please Fax to (434) 243-6999 IF LABEL NOT AVAILABLE, WRITE IN PT NAME & MR# Schedule at (434) 243-6888 Patient Name:_________________________________________________ MR#___________________ Pre/Post-op Y N Date of Surgery____________________ Date of Test____________________ DOB _______/_______/_______ Weight: __________ Phone #_______________________ Insurance Company & Plan Pre Authorization Number Attending MD/Pic # Ordering MD/Pic # U Referring Clinic/Office Where Report Should Be Sent Phone Number of Contact Person Name Box & Fax Number R O STUDY DESIRED AND PLEASE NUMBER THE DIAGNOSIS ACCORDINGLY L X Study X Study X Study X Study X Study O Contrast Studies Nephrostogram Plain Films: KUB Lumbar Spine IVP w/o Tomos Loopogram Chest Single View Abd 2 views Pelvis G IVP w/Tomos VCUG Chest 2 Views Fluoroscopy Retrograde Urethrogram (Voiding cystourethrogram) Chest w/Oblique views (Specify): Y Retrogrades Tomograms Cystogram Video Urodynamics Reading of Outside Films I Other Study-Not Listed (Specify): M A G I Clinical Indications for Exam (Mandatory): N G ICD-9 Dx Code(Mandatory): R E Q Physician Signature:____________________________________________________ U X Code Diagnosis X Code Diagnosis X Code Diagnosis E Esophagus/Chest GU Symptoms 786.2 Cough 185 Prostate CA 599.0 Urinary Tract Infection S 786.50 Unspec Chest Pain 188.8 Bladder CA NEC 599.7 Hematuria T Abdomen/GI 401.9 Hypertension -

Obstruction of the Urinary Tract 2567
Chapter 540 ◆ Obstruction of the Urinary Tract 2567 Table 540-1 Types and Causes of Urinary Tract Obstruction LOCATION CAUSE Infundibula Congenital Calculi Inflammatory (tuberculosis) Traumatic Postsurgical Neoplastic Renal pelvis Congenital (infundibulopelvic stenosis) Inflammatory (tuberculosis) Calculi Neoplasia (Wilms tumor, neuroblastoma) Ureteropelvic junction Congenital stenosis Chapter 540 Calculi Neoplasia Inflammatory Obstruction of the Postsurgical Traumatic Ureter Congenital obstructive megaureter Urinary Tract Midureteral structure Jack S. Elder Ureteral ectopia Ureterocele Retrocaval ureter Ureteral fibroepithelial polyps Most childhood obstructive lesions are congenital, although urinary Ureteral valves tract obstruction can be caused by trauma, neoplasia, calculi, inflam- Calculi matory processes, or surgical procedures. Obstructive lesions occur at Postsurgical any level from the urethral meatus to the calyceal infundibula (Table Extrinsic compression 540-1). The pathophysiologic effects of obstruction depend on its level, Neoplasia (neuroblastoma, lymphoma, and other retroperitoneal or pelvic the extent of involvement, the child’s age at onset, and whether it is tumors) acute or chronic. Inflammatory (Crohn disease, chronic granulomatous disease) ETIOLOGY Hematoma, urinoma Ureteral obstruction occurring early in fetal life results in renal dys- Lymphocele plasia, ranging from multicystic kidney, which is associated with ure- Retroperitoneal fibrosis teral or pelvic atresia (see Fig. 537-2 in Chapter 537), to various -

Diagnostic Accuracy of Sonourethrography for Anterior Urethral Stricture Taking Retrograde Urethrogram As Gold Standard
ORIGINAL ARTICLE Diagnostic Accuracy of Sonourethrography for Anterior Urethral Stricture Taking Retrograde Urethrogram as Gold Standard USMAN HASSAN1, RAHAM BACHA 2, MUHAMMAD FAROOQ KHAN 3, TALHA LAIQUE4 1Department of Radiology, Hanif Medical Centre, Vehari-Pakistan 2Department of Radiology, University of Lahore, Lahore-Pakistan 3Department of Radiology, Bakhtawar Amin Hospital, Multan-Pakistan 4Department of Pharmacology, Lahore Medical and Dental College, Lahore-Pakistan Correspondence to Dr. Talha Laique, Email: [email protected] Tel:+92-331-0346682 ABSTRACT Background: Diagnostic accuracy can be improved by using sonourethrography (high-resolution ultrasound) for male anterior urethra. Aim: To find the diagnostic accuracy of sonourethrography for diagnosis of anterior urethral stricture taking retrograde urethrogram as gold standard. Study design: Cross-sectional study. Methodology: Patients (n=102) presented with lower urinary tract symptoms. All enrolled patients had first retrograde urethrogram followed by sonourethrography in the Department of Radiology, Family Care Diagnostic Center Multan-Pakistan for 6 months by keeping confidence interval 95%. Informed consent was taken from all of them. Data analyzed by SPSS 24.0v. Mean ± SD for age whereas frequency and percentages were given for stricture and site of stricture. Significant p-value was of ≤0.05. Results: The mean age of patients was 37.41 ± 10.96 years with range (20-66 years). Stricture was observed in 23.5% (24 patients) by SUG whereas it was in 24.5% (25 patients) by RUG. Sensitivity of sonourethrography as a diagnostic tool of anterior urethral stricture among males in our study was 96% whereas specificity was 100%. Conclusion: It gives more accurate information about periurethral fibrosis associated with strictures and other abnormalities thus it can be a useful as well as effective modality for diagnosis of anterior urethral pathologies. -

Imaging and Other Investigations
CHAPTER 13 Committee 9 Imaging and other Investigations Chairman A. TUBARO (ITALY) Members W. ARTIBANI (ITALY), C. BARTRAM (UK), J.D. DELANCEY (USA), H.P. DIETZ (AUSTRALIA), V. K HULLAR (UK), P. Z IMMERN (USA) Consultant W. UMEK (AUSTRIA) 707 CONTENTS C. IMAGING IN FAECAL A. INTRODUCTION INCONTINENCE B. IMAGING IN URINARY D. PAD TESTING INCONTINENCE AND PELVIC FLOOR DYSFUNCTION E. OTHER INVESTIGATIONS B1. IMAGING OF THE UPPER URINARY TRACT F. CONCLUSIONS B2. LOWER URINARY TRACT (LUT) IMAGING B3. SPECIAL ISSUES 708 Imaging and other Investigations A. TUBARO W. ARTIBANI, C. BARTRAM, H.P. DIETZ, V. KHULLAR, J.D. DELANCEY,P. ZIMMERN W. UMEK modalities may provide evidence regarding the seve- A. INTRODUCTION rity of the disease, indications for treatment, pro- gnostic values as treatment outcome or patient pro- gnosis, but they can also be used to monitor patient conditions over time and in treatment follow-up. The committee evaluated the current evidence regar- Imaging can also be used to evaluate treatment out- ding imaging techniques and clinical indications in come as well as for research purposes. At the end of patients with urinary or faecal incontinence, pelvic each paragraph, recommendations for the clinical floor dysfunction and pelvic organ prolapse. Addi- use of a certain imaging modality are provided and tional related issues such as pad testing were also reviewed. The present chapter is based upon the out- the relative level of evidence is stated. Areas of inter- come of the 2nd International Consultation on Incon- est for further research are identified. tinence which was held in Paris in 2001 [1].