The Controversies of Parabens – an Overview Nowadays
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary Paraben Concentrations and Ovarian Aging Among Women from a Fertility Center
Urinary Paraben Concentrations and Ovarian Aging among Women from a Fertility Center The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Smith, Kristen W., Irene Souter, Irene Dimitriadis, Shelley Ehrlich, Paige L. Williams, Antonia M. Calafat, and Russ Hauser. 2013. “Urinary Paraben Concentrations and Ovarian Aging among Women from a Fertility Center.” Environmental Health Perspectives 121 (11-12): 1299-1305. doi:10.1289/ehp.1205350. http://dx.doi.org/10.1289/ehp.1205350. Published Version doi:10.1289/ehp.1205350 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:11879222 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA All EHP content is accessible to individuals with disabilities. A fully accessible (Section 508–compliant) HTML version of this article is available at http://dx.doi.org/10.1289/ehp.1205350. Research Urinary Paraben Concentrations and Ovarian Aging among Women from a Fertility Center Kristen W. Smith,1 Irene Souter,2 Irene Dimitriadis,1,2 Shelley Ehrlich,1 Paige L. Williams,3 Antonia M. Calafat,4 and Russ Hauser1,2 1Department of Environmental Health, Harvard School of Public Health, Boston, Massachusetts, USA; 2Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology and Infertility, Harvard Medical School/Massachusetts General Hospital Fertility Center, Boston, Massachusetts, USA; 3Department of Biostatistics, Harvard School of Public Health, Boston, Massachusetts, USA; 4National Center for Environmental Health, Centers for Disease Control and Prevention, Atlanta, Georgia, USA In 2008, the Cosmetic Ingredient Review BACKGROUND: Parabens are preservatives commonly used in personal care products, pharmaceuticals, Panel concluded that parabens used in cos- and foods. -

Studies on the Effects of Paraben Mixtures on MCF-7 Breast Cancer
Studies on the Effects of Paraben Mixtures on MCF-7 Breast Cancer Cells in Culture A thesis submitted in partial fulfilment of the requirements for the Degree of Masters of Science in Biochemistry In the Department of Chemistry At the University of Canterbury New Zealand By Kristie Webber University of Canterbury 2013 Table of Contents Acknowledgements .............................................................................................................................. i Abstract ............................................................................................................................................... ii Abbreviations ..................................................................................................................................... iii List of figures and tables .................................................................................................................... iv 1 Introduction ......................................................................................................................................... 1 1.1 Hormones and the endocrine system ........................................................................................... 2 1.2 Estrogens ....................................................................................................................................... 5 1.2.1 What are estrogens? .............................................................................................................. 5 1.2.2 17β-Estradiol ......................................................................................................................... -

Science of the Total Environment 445–446 (2013) 299–305
Science of the Total Environment 445–446 (2013) 299–305 Contents lists available at SciVerse ScienceDirect Science of the Total Environment journal homepage: www.elsevier.com/locate/scitotenv Relationship between urinary triclosan and paraben concentrations and serum thyroid measures in NHANES 2007–2008 Erika S. Koeppe, Kelly K. Ferguson, Justin A. Colacino, John D. Meeker ⁎ Department of Environmental Health Sciences, University of Michigan School of Public Health, Ann Arbor, MI, United States HIGHLIGHTS ► Triclosan and parabens are widely used in the US and elsewhere. ► Biomarkers of exposure were examined in relation to serum thyroid hormone levels. ► In adults, we observed inverse associations between parabens and thyroid hormones. ► In adolescents, we observed positive associations between triclosan and total T3. ► Future research is necessary to confirm findings and explore clinical relevance. article info abstract Article history: Triclosan and parabens are broad spectrum antimicrobials used in a range of consumer products. In vitro and Received 28 September 2012 animal studies have suggested the potential for these compounds to disrupt thyroid function, though studies Received in revised form 17 December 2012 in humans have been limited. The objective of the study was to assess the relationship of urinary concentra- Accepted 17 December 2012 tions of triclosan and parabens with serum thyroid measures in a large, representative sample of the US pop- Available online 20 January 2013 ulation. We conducted an exploratory, cross-sectional analysis of data on urinary biomarkers of triclosan and paraben exposure and serum thyroid measures obtained from 1831 subjects (ages≥12 years) as part of the Keywords: – Biomarkers 2007 2008 National Health and Nutrition Examination Survey (NHANES). -

Paraben and Breast Cancer: a Stromal Link
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 5-2020 Paraben and Breast Cancer: A Stromal Link Emily Hager University of Tennessee, [email protected] Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Recommended Citation Hager, Emily, "Paraben and Breast Cancer: A Stromal Link. " PhD diss., University of Tennessee, 2020. https://trace.tennessee.edu/utk_graddiss/5915 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Emily Hager entitled "Paraben and Breast Cancer: A Stromal Link." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Nutritional Sciences. Ling Zhao, Major Professor We have read this dissertation and recommend its acceptance: Jay Whelan, Guoxen Chen, Hwa-Chain Wang Accepted for the Council: Dixie L. Thompson Vice Provost and Dean of the Graduate School (Original signatures are on file with official studentecor r ds.) Paraben and Breast Cancer: A Stromal Link A Dissertation Presented for the Doctor of Philosophy Degree The University of Tennessee, Knoxville Emily Nicole Hager May 2020 ACKNOWLEDGMENTS I am greatly honored and humbled to have pursued my Ph.D. -

206679Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 206679Orig1s000 PHARMACOLOGY REVIEW(S) DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH PHARMACOLOGY/TOXICOLOGY NDA/BLA REVIEW AND EVALUATION Application number: 206679 Supporting document/s: SDN10, SN0000 Applicant’s letter date: June 22, 2015 CDER stamp date: June 22, 2015 Product: Simvastatin oral suspension Indication: Treatment of primary and homozygous familial hypercholesterolemia in adults and for the treatment of heterozygous familial hypercholesterolemia in adult and pediatric patients (≥10 years) Applicant: Rosemont Pharmaceuticals (a wholly owned subsidiary of Perrigo Pharmaceuticals, U.S. agent) Review Division: Division of Metabolism and Endocrinology Products Reviewer/Team Leader: C. Lee Elmore, PhD Division Director: Jean-Marc Guettier, MD Project Manager: Richard Whitehead Disclaimer Except as specifically identified, all data and information discussed below and necessary for approval of NDA 206679 are owned by Rosemont Pharmaceuticals Ltd. or are data for which Rosemont Pharmaceuticals Ltd. has obtained a written right of reference. Any information or data necessary for approval of NDA 206679 that Rosemont Pharmaceuticals Ltd. does not own or have a written right to reference constitutes one of the following: (1) published literature, or (2) a prior FDA finding of safety or effectiveness for a listed drug, as reflected in the drug’s approved labeling. Any data or information described or referenced below from reviews or publicly available summaries of a previously approved application is for descriptive purposes only and is not relied upon for approval of NDA number 206679. 1 Reference ID: 3906236 NDA 206679 Reviewer/Team Leader: C. -
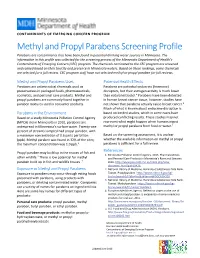
Methyl and Propyl Parabens Screening Profile Parabens Are Contaminants That Have Been Found in Potential Drinking Water Sources in Minnesota
CONTAMINANTS OF EMERGING CONCERN PROGRAM Methyl and Propyl Parabens Screening Profile Parabens are contaminants that have been found in potential drinking water sources in Minnesota. The information in this profile was collected for the screening process of the Minnesota Department of Health’s Contaminants of Emerging Concern (CEC) program. The chemicals nominated to the CEC program are screened and ranked based on their toxicity and presence in Minnesota waters. Based on these rankings, some chemicals are selected for a full review. CEC program staff have not selected methyl or propyl paraben for full reviews. Methyl and Propyl Parabens Uses Potential Health Effects Parabens are antimicrobial chemicals used as Parabens are potential endocrine (hormone) preservatives in packaged foods, pharmaceuticals, disruptors, but their estrogen activity is much lower cosmetics, and personal care products. Methyl and than natural estradiol.4 Parabens have been detected propyl parabens are commonly found together in in human breast cancer tissue; however, studies have paraben mixtures used in consumer products. not shown that parabens actually cause breast cancer.4 Much of what is known about endocrine disruption is Parabens in the Environment based on limited studies, which in some cases have Based on a study Minnesota Pollution Control Agency produced conflicting results. These studies may not (MPCA) did in Minnesota in 2010, parabens are represent what might happen when humans ingest widespread in Minnesota’s surface water. Twenty-one methyl or propyl parabens from food or water.4 percent of streams sampled had propyl paraben, with a maximum concentration of 0.6 parts per billion Based on the screening assessment, it is unclear (ppb). -

Northern Saskatchewan Prenatal Biomonitoring Study Technical
Northern Saskatchewan Prenatal Biomonitoring Study Technical Summary Report Ministry of Health, Government of Saskatchewan, 2019 Northern Saskatchewan Prenatal Biomonitoring Study Summary Report Ministry of Health, Government of Saskatchewan, 2019 For more information contact: Environmental Health Population Health Branch Miinistry of Health 3475 Albert Street, Regina, SK, Canada, S4S 6X6 Telephone: 306-787-8847 Website: https://publications.saskatchewan.ca:443/api/v1/products/101374/formats/112048/download TABLE OF CONTENTS Executive Summary ......................................................................................................................................................... 1 Introduction ..................................................................................................................................................................... 4 Study Rationale ......................................................................................................................................................... 4 Biomonitoring as the Tool of Choice ......................................................................................................................... 5 Stakeholder Analysis ................................................................................................................................................. 6 Alberta’s Biomonitoring Program ......................................................................................................................... 6 Engagement with Northern -

Comprehensive Effects of Parabens in Human Physiology
Comprehensive Effects of Parabens in Human Physiology Seeham Ali Qasim Alkafajy1*, and Rawaa Abdul-Ameer Abdul-Jabbar1 1. Dept of Biology, College of Science, Mutansiriyah University, Iraq *Corresponding author: [email protected] Abstract:- Parabens are industrial chemicals that have been widely applied as preservatives for many products, such as cosmetics, medicines and foodstuffs, due to their ability to extend the life of products and prevent pathogenic bacteria and mold from developing them. Paraben compounds include methylparaben, ethylparaben, propylparaben, butylparaben, heptylparaben and benzyl-paraben.P-hydroxybenzoic acid is the main receptor of parabens in the human body, recently, it has been observed these compounds are present in blood serum and urine in different concentrations after multiple and long-term exposure to parabens as it is absorbed through the skin due to the ability of parabens to dissolve in water. Also, the increased ability of parabens to penetrate the skin depends on their structures, length of ester side chains, and the type of volatile solvents such as acetone and ethanol. Academic studies have also proven the presence of these chemical compounds in the breast tissue of breast cancer patients, as the estrogenic properties of parabens may play a role in the development of breast cancer that has raised public concern about their use. Other studies have confirmed that parabens are classified among substances that cause endocrine function disruption, such as the thyroid and adrenal glands. On the other hand, researches indicated that women who have a high concentration of polyethylene paraben suffer from short menstrual periods and poor fertility, and current studies conducted on male rats have found that parabens negatively affect the function of the male reproductive system by reducing the concentration of sperm, reducing the level of testosterone secretion in their serum and comprehensively affects the quality of semen in males. -

United States Patent (19) 11 Patent Number: 6,096,733 Lubkin (45) Date of Patent: Aug
US006096733A United States Patent (19) 11 Patent Number: 6,096,733 Lubkin (45) Date of Patent: Aug. 1, 2000 54) DRUGS FOR TOPICAL APPLICATION OF Olige Estradio-Hemihydrat-Augentropfen 0.025 Prozent; SEX STEROIDS IN THE TREATMENT OF Fischer, H and Reimann H., Neues Rezeptur-Formularium DRY EYE SYNDROME, AND METHODS OF (NRF) Pharmazeutisches Laboratorium, Pharmazeutische PREPARATION AND APPLICATION Zeitung (Pharm. Ztg.) Jan. 14, 1999 144/2 (38-40). 75 Inventor: Virginia Lubkin, One Blackstone Pl., Benitez del Castillo, J.M.E., et al., “ffects of Estrogen Use on Bronx, N.Y. 10471 Lens Transmittance in Postmenopausal Women,” Ophthal 73 Assignee: Virginia Lubkin, Brnx, N.Y. mology 1997: 104:970–973. Sator, M.O., et al., “Treatment of menopausal keratocon 21 Appl. No.: 09/208,423 junctivitis sicca with topical oestradiol, Br. J. Obstet. Gyn. 1998; 105:100-102. 22 Filed: Dec. 10, 1998 (51) Int. Cl." ..................................................... A61K 31/56 52 U.S. Cl. .......................... 514/182; 514/169; 514/177; Primary Examiner Zohreh Fay 514/178; 514/912; 514/914 Attorney, Agent, or Firm Shanks & Herbert 58 Field of Search ..................................... 514/182, 169, 57 ABSTRACT 514/177, 178,912, 914 A topical drug application for the alleviation of kerato 56) References Cited conjunctivitis Sicca (dry eye syndrome) is comprised of a U.S. PATENT DOCUMENTS solution of 17-B-estradiol suspended or dissolved in a vehicle, and the method of preparation and application of the 4,642,305 2/1987 Johansson et al. Same. In the preferred embodiments, 17-B-estradiol is in a 4,774.236 9/1988 Cook et al. -

Sccs/1514/13
SCCS/1514/13 Scientific Committee on Consumer Safety SCCS OPINION ON Parabens Updated request for a scientific opinion on propyl- and butylparaben COLIPA n° P82 The SCCS adopted this opinion by written procedure on 3 May 2013 1 SCCS/1514/13 Opinion on parabens, updated request on propyl- and butylparaben About the Scientific Committees Three independent non-food Scientific Committees provide the Commission with the scientific advice it needs when preparing policy and proposals relating to consumer safety, public health and the environment. The Committees also draw the Commission's attention to the new or emerging problems which may pose an actual or potential threat. They are: the Scientific Committee on Consumer Safety (SCCS), the Scientific Committee on Health and Environmental Risks (SCHER) and the Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR) and are made up of external experts. In addition, the Commission relies upon the work of the European Food Safety Authority (EFSA), the European Medicines Agency (EMA), the European Centre for Disease prevention and Control (ECDC) and the European Chemicals Agency (ECHA). SCCS The Committee shall provide opinions on questions concerning all types of health and safety risks (notably chemical, biological, mechanical and other physical risks) of non-food consumer products (for example: cosmetic products and their ingredients, toys, textiles, clothing, personal care and household products such as detergents, etc.) and services (for example: tattooing, artificial sun tanning, etc.). Scientific Committee members Ulrike Bernauer, Qasim Chaudhry, Gisela Degen, Elsa Nielsen, Thomas Platzek, Suresh Chandra Rastogi, Christophe Rousselle, Jan van Benthem, Pieter Coenraads, Maria Dusinska, David Gawkrodger, Werner Lilienblum, Andreas Luch, Manfred Metzler, Nancy Monteiro-Rivière. -

Opinion of the Scientific Committee on Consumer Safety on Parabens (P82)
SCCS/1348/10 Revision 22 March 2011 Scientific Committee on Consumer Safety SCCS OPINION ON Parabens COLIPA n° P82 The SCCS adopted this opinion at its 9th plenary on 14 December 2010 SCCS/1348/10 Opinion on parabens ___________________________________________________________________________________________ About the Scientific Committees Three independent non-food Scientific Committees provide the Commission with the scientific advice it needs when preparing policy and proposals relating to consumer safety, public health and the environment. The Committees also draw the Commission's attention to the new or emerging problems which may pose an actual or potential threat. They are: the Scientific Committee on Consumer Safety (SCCS), the Scientific Committee on Health and Environmental Risks (SCHER) and the Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR) and are made up of external experts. In addition, the Commission relies upon the work of the European Food Safety Authority (EFSA), the European Medicines Agency (EMA), the European Centre for Disease prevention and Control (ECDC) and the European Chemicals Agency (ECHA). SCCS The Committee shall provide opinions on questions concerning all types of health and safety risks (notably chemical, biological, mechanical and other physical risks) of non-food consumer products (for example: cosmetic products and their ingredients, toys, textiles, clothing, personal care and household products such as detergents, etc.) and services (for example: tattooing, artificial -

First Assessment of Triclosan, Triclocarban and Paraben Mass Loads at a Very Large Regional Scale: Case of Paris Conurbation (France)
First assessment of triclosan, triclocarban and paraben mass loads at a very large regional scale: case of Paris conurbation (France). Johnny Gasperi, Darine Geara, Catherine Lorgeoux, Adèle Bressy, Sifax Zedek, Vincent Rocher, Antoine El Samrani, Ghassan Chebbo, Régis Moilleron To cite this version: Johnny Gasperi, Darine Geara, Catherine Lorgeoux, Adèle Bressy, Sifax Zedek, et al.. First as- sessment of triclosan, triclocarban and paraben mass loads at a very large regional scale: case of Paris conurbation (France).. Science of the Total Environment, Elsevier, 2014, 493, pp.854-61. 10.1016/j.scitotenv.2014.06.079. hal-01063311 HAL Id: hal-01063311 https://hal-enpc.archives-ouvertes.fr/hal-01063311 Submitted on 23 May 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. FIRST ASSESSMENT OF TRICLOSAN, TRICLOCARBAN AND PARABEN MASS LOADS AT A VERY LARGE REGIONAL SCALE: CASE OF PARIS CONURBATION (FRANCE) Johnny Gasperi1*, Darine Geara1,2, Catherine Lorgeoux1,3, Adèle Bressy1, Sifax Zedek1, Vincent Rocher4, Antoine El Samrani5, Ghassan Chebbo1, Régis Moilleron1* 1. Université Paris-Est, LEESU, UMR MA 102 - AgroParisTech, 61 avenue du Général de Gaulle, 94010 Créteil Cedex, France. 2. Lebanese Atomic Energy Commission, Airport Highway BP 11 82 81, Riad El-Solh 1107 2260, Beirut (Lebanon).