Genetic Heterogeneity and Prognostic Impact of Recurrent ANK2 and TP53 Mutations in Mantle Cell Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of Genes Associated with Sudden Cardiac Death (Scdgseta) Gene
List of genes associated with sudden cardiac death (SCDgseta) mRNA expression in normal human heart Entrez_I Gene symbol Gene name Uniprot ID Uniprot name fromb D GTEx BioGPS SAGE c d e ATP-binding cassette subfamily B ABCB1 P08183 MDR1_HUMAN 5243 √ √ member 1 ATP-binding cassette subfamily C ABCC9 O60706 ABCC9_HUMAN 10060 √ √ member 9 ACE Angiotensin I–converting enzyme P12821 ACE_HUMAN 1636 √ √ ACE2 Angiotensin I–converting enzyme 2 Q9BYF1 ACE2_HUMAN 59272 √ √ Acetylcholinesterase (Cartwright ACHE P22303 ACES_HUMAN 43 √ √ blood group) ACTC1 Actin, alpha, cardiac muscle 1 P68032 ACTC_HUMAN 70 √ √ ACTN2 Actinin alpha 2 P35609 ACTN2_HUMAN 88 √ √ √ ACTN4 Actinin alpha 4 O43707 ACTN4_HUMAN 81 √ √ √ ADRA2B Adrenoceptor alpha 2B P18089 ADA2B_HUMAN 151 √ √ AGT Angiotensinogen P01019 ANGT_HUMAN 183 √ √ √ AGTR1 Angiotensin II receptor type 1 P30556 AGTR1_HUMAN 185 √ √ AGTR2 Angiotensin II receptor type 2 P50052 AGTR2_HUMAN 186 √ √ AKAP9 A-kinase anchoring protein 9 Q99996 AKAP9_HUMAN 10142 √ √ √ ANK2/ANKB/ANKYRI Ankyrin 2 Q01484 ANK2_HUMAN 287 √ √ √ N B ANKRD1 Ankyrin repeat domain 1 Q15327 ANKR1_HUMAN 27063 √ √ √ ANKRD9 Ankyrin repeat domain 9 Q96BM1 ANKR9_HUMAN 122416 √ √ ARHGAP24 Rho GTPase–activating protein 24 Q8N264 RHG24_HUMAN 83478 √ √ ATPase Na+/K+–transporting ATP1B1 P05026 AT1B1_HUMAN 481 √ √ √ subunit beta 1 ATPase sarcoplasmic/endoplasmic ATP2A2 P16615 AT2A2_HUMAN 488 √ √ √ reticulum Ca2+ transporting 2 AZIN1 Antizyme inhibitor 1 O14977 AZIN1_HUMAN 51582 √ √ √ UDP-GlcNAc: betaGal B3GNT7 beta-1,3-N-acetylglucosaminyltransfe Q8NFL0 -

Heterotrimeric Go Protein Links Wnt-Frizzled Signaling with Ankyrins to Regulate the Neuronal Microtubule Cytoskeleton Anne-Marie Lüchtenborg1,2, Gonzalo P
© 2014. Published by The Company of Biologists Ltd | Development (2014) 141, 3399-3409 doi:10.1242/dev.106773 RESEARCH ARTICLE Heterotrimeric Go protein links Wnt-Frizzled signaling with ankyrins to regulate the neuronal microtubule cytoskeleton Anne-Marie Lüchtenborg1,2, Gonzalo P. Solis1, Diane Egger-Adam2, Alexey Koval1, Chen Lin1,2, Maxime G. Blanchard1, Stephan Kellenberger1 and Vladimir L. Katanaev1,2,* ABSTRACT The evolutionarily conserved Wg pathway is important for Drosophila neuromuscular junctions (NMJs) represent a powerful numerous developmental programs and cellular processes (Logan model system with which to study glutamatergic synapse formation and Nusse, 2004). In the nervous system of Drosophila,Wg and remodeling. Several proteins have been implicated in these signaling is involved in the formation of neuromuscular junctions processes, including components of canonical Wingless (Drosophila (NMJs) (Packard et al., 2002; Miech et al., 2008). Being a Wnt1) signaling and the giant isoforms of the membrane-cytoskeleton glutamatergic synapse, the Drosophila NMJ provides a useful linker Ankyrin 2, but possible interconnections and cooperation experimental model with which to study mammalian central between these proteins were unknown. Here, we demonstrate that nervous system synapses, their formation and remodeling (Collins the heterotrimeric G protein Go functions as a transducer of Wingless- and DiAntonio, 2007). The Drosophila NMJ is a beads-on-a-string- Frizzled 2 signaling in the synapse. We identify Ankyrin 2 as a target like structure that is formed at the axon terminus and is composed of – – of Go signaling required for NMJ formation. Moreover, the Go-ankyrin distinct circular structures the synaptic boutons which contain interaction is conserved in the mammalian neurite outgrowth pathway. -

Circular RNA Hsa Circ 0005114‑Mir‑142‑3P/Mir‑590‑5P‑ Adenomatous
ONCOLOGY LETTERS 21: 58, 2021 Circular RNA hsa_circ_0005114‑miR‑142‑3p/miR‑590‑5p‑ adenomatous polyposis coli protein axis as a potential target for treatment of glioma BO WEI1*, LE WANG2* and JINGWEI ZHAO1 1Department of Neurosurgery, China‑Japan Union Hospital of Jilin University, Changchun, Jilin 130033; 2Department of Ophthalmology, The First Hospital of Jilin University, Jilin University, Changchun, Jilin 130021, P.R. China Received September 12, 2019; Accepted October 22, 2020 DOI: 10.3892/ol.2020.12320 Abstract. Glioma is the most common type of brain tumor APC expression with a good overall survival rate. UALCAN and is associated with a high mortality rate. Despite recent analysis using TCGA data of glioblastoma multiforme and the advances in treatment options, the overall prognosis in patients GSE25632 and GSE103229 microarray datasets showed that with glioma remains poor. Studies have suggested that circular hsa‑miR‑142‑3p/hsa‑miR‑590‑5p was upregulated and APC (circ)RNAs serve important roles in the development and was downregulated. Thus, hsa‑miR‑142‑3p/hsa‑miR‑590‑5p‑ progression of glioma and may have potential as therapeutic APC‑related circ/ceRNA axes may be important in glioma, targets. However, the expression profiles of circRNAs and their and hsa_circ_0005114 interacted with both of these miRNAs. functions in glioma have rarely been studied. The present study Functional analysis showed that hsa_circ_0005114 was aimed to screen differentially expressed circRNAs (DECs) involved in insulin secretion, while APC was associated with between glioma and normal brain tissues using sequencing the Wnt signaling pathway. In conclusion, hsa_circ_0005114‑ data collected from the Gene Expression Omnibus database miR‑142‑3p/miR‑590‑5p‑APC ceRNA axes may be potential (GSE86202 and GSE92322 datasets) and explain their mecha‑ targets for the treatment of glioma. -

Cardiomyopathy
JACC: BASIC TO TRANSLATIONAL SCIENCE VOL.1,NO.5,2016 ª 2016 THE AUTHORS. PUBLISHED BY ELSEVIER ON BEHALF OF THE AMERICAN ISSN 2452-302X COLLEGE OF CARDIOLOGY FOUNDATION. THIS IS AN OPEN ACCESS ARTICLE UNDER http://dx.doi.org/10.1016/j.jacbts.2016.05.004 THE CC BY-NC-ND LICENSE (http://creativecommons.org/licenses/by-nc-nd/4.0/). PRE-CLINICAL RESEARCH FLNC Gene Splice Mutations Cause Dilated Cardiomyopathy a a b,c a d Rene L. Begay, BS, Charles A. Tharp, MD, August Martin, Sharon L. Graw, PHD, Gianfranco Sinagra, MD, e a a b,c,f b,c Daniela Miani, MD, Mary E. Sweet, BA, Dobromir B. Slavov, PHD, Neil Stafford, MD, Molly J. Zeller, b,c a d g g Rasha Alnefaie, Teisha J. Rowland, PHD, Francesca Brun, MD, Kenneth L. Jones, PHD, Katherine Gowan, a b,c a Luisa Mestroni, MD, Deborah M. Garrity, PHD, Matthew R.G. Taylor, MD, PHD VISUAL ABSTRACT HIGHLIGHTS Deoxyribonucleic acid obtained from 2 large DCM families was studied using whole-exome sequencing and cose- gregation analysis resulting in the iden- tification of a novel disease gene, FLNC. The2families,fromthesameItalian region, harbored the same FLNC splice- site mutation (FLNC c.7251D1G>A). A third U.S. family was then identified with a novel FLNC splice-site mutation (FLNC c.5669-1delG) that leads to haploinsufficiency as shown by the FLNC Western blot analysis of the heart muscle. The FLNC ortholog flncb morpholino was injected into zebrafish embryos, and when flncb was knocked down caused a cardiac dysfunction phenotype. -

Next Generation Sequencing for Molecular Confirmation of Hereditary
Arch Cardiol Mex. 2015;85(1):68---72 www.elsevier.com.mx SPECIAL ARTICLE Next generation sequencing for molecular confirmation of hereditary sudden cardiac death syndromes a,∗ b b b Manlio F. Márquez , David Cruz-Robles , Selene Ines-Real , Gilberto Vargas-Alarcón , a Manuel Cárdenas a Departamento de Electrofisiología, Instituto Nacional de Cardiología Ignacio Chávez, México, D.F., Mexico b Departamento de Biología Molecular, Instituto Nacional de Cardiología Ignacio Chávez, México, D.F., Mexico Received 26 March 2014; accepted 8 December 2014 KEYWORDS Abstract Hereditary sudden cardiac death syndromes comprise a wide range of diseases result- Arrhythmias; ing from alteration in cardiac ion channels. Genes involved in these syndromes represent diverse Hereditary sudden mutations that cause the altered encoding of the diverse proteins constituting these channels, cardiac death thus affecting directly the currents of the corresponding ions. In the present article we will syndromes; briefly review how to arrive to a clinical diagnosis and we will present the results of molecular Right ventricle genetic studies made in Mexican subjects attending the SCD Syndromes Clinic of the National arrhythmogenic Institute of Cardiology of Mexico City. cardiomyopathy; © 2014 Instituto Nacional de Cardiología Ignacio Chávez. Published by Masson Doyma México Brugada syndrome S.A. All rights reserved. PALABRAS CLAVE Confirmación diagnóstica molecular mediante secuenciación masiva de nueva Arritmias; generación (‘‘next generation sequencing’’) en síndromes hereditarios de muerte Síndromes súbita cardíaca hereditarios de Resumen Los síndromes hereditarios de muerte súbita cardíaca comprenden una amplia gama muerte súbita; Displasia de enfermedades resultantes de la alteración en los canales iónicos cardíacos. Los genes implicados en estos síndromes presentan mutaciones que causan alteraciones de las diversas Arritmogénica del proteínas que constituyen estos canales y que, por lo tanto, afectan directamente a las difer- ventriculo derecho; entes corrientes iónicas. -
A Missense Mutation in the RSRSP Stretch of Rbm20 Causes Dilated
www.nature.com/scientificreports OPEN A missense mutation in the RSRSP stretch of Rbm20 causes dilated cardiomyopathy and atrial fbrillation in mice Kensuke Ihara1,2*, Tetsuo Sasano2, Yuichi Hiraoka3, Marina Togo‑Ohno4, Yurie Soejima5, Motoji Sawabe5, Megumi Tsuchiya6, Hidesato Ogawa6, Tetsushi Furukawa1 & Hidehito Kuroyanagi4* Dilated cardiomyopathy (DCM) is a fatal heart disease characterized by left ventricular dilatation and cardiac dysfunction. Recent genetic studies on DCM have identifed causative mutations in over 60 genes, including RBM20, which encodes a regulator of heart‑specifc splicing. DCM patients with RBM20 mutations have been reported to present with more severe cardiac phenotypes, including impaired cardiac function, atrial fbrillation (AF), and ventricular arrhythmias leading to sudden cardiac death, compared to those with mutations in the other genes. An RSRSP stretch of RBM20, a hotspot of missense mutations found in patients with idiopathic DCM, functions as a crucial part of its nuclear localization signals. However, the relationship between mutations in the RSRSP stretch and cardiac phenotypes has never been assessed in an animal model. Here, we show that Rbm20 mutant mice harboring a missense mutation S637A in the RSRSP stretch, mimicking that in a DCM patient, demonstrated severe cardiac dysfunction and spontaneous AF and ventricular arrhythmias mimicking the clinical state in patients. In contrast, Rbm20 mutant mice with frame‑shifting deletion demonstrated less severe phenotypes, although loss of RBM20‑dependent alternative splicing was indistinguishable. RBM20S637A protein cannot be localized to the nuclear speckles, but accumulated in cytoplasmic, perinuclear granule‑like structures in cardiomyocytes, which might contribute to the more severe cardiac phenotypes. Dilated cardiomyopathy (DCM) is a fatal cardiac disease characterized by enlargement of the cardiac chambers and impaired systolic function1. -

Drosophila Tau Negatively Regulates Translation and Olfactory Long-Term Memory, but Facilitates Footshock Habituation and Cytoskeletal Homeostasis
The Journal of Neuroscience, October 16, 2019 • 39(42):8315–8329 • 8315 Cellular/Molecular Drosophila Tau Negatively Regulates Translation and Olfactory Long-Term Memory, But Facilitates Footshock Habituation and Cytoskeletal Homeostasis X Katerina Papanikolopoulou,1* XIlianna G. Roussou,1* XJean Y. Gouzi,1* Martina Samiotaki,2 George Panayotou,2 X Luca Turin,1 and XEfthimios M.C. Skoulakis1 1Institute for Fundamental Biomedical Research, and 2Institute for Bioinnovation, Biomedical Sciences Research Centre “Alexander Fleming,” 16672 Vari, Greece Although the involvement of pathological tau in neurodegenerative dementias is indisputable, its physiological roles have remained elusive in part because its abrogation has been reported without overt phenotypes in mice and Drosophila. This was addressed using the recently described Drosophila tauKO and Mi{MIC} mutants and focused on molecular and behavioral analyses. Initially, we show that Drosophila tau (dTau) loss precipitates dynamic cytoskeletal changes in the adult Drosophila CNS and translation upregulation. Signif- icantly, we demonstrate for the first time distinct roles for dTau in adult mushroom body (MB)-dependent neuroplasticity as its down- regulation within ␣ЈЈneurons impairs habituation. In accord with its negative regulation of translation, dTau loss specifically enhances protein synthesis-dependent long-term memory (PSD-LTM), but not anesthesia-resistant memory. In contrast, elevation of the protein in the MBs yielded premature habituation and depressed PSD-LTM. Therefore, tau loss in Drosophila dynamically alters brain cytoskel- etal dynamics and profoundly affects neuronal proteostasis and plasticity. Key words: Drosophila; habituation; memory; proteome; tau Significance Statement We demonstrate that despite modest sequence divergence, the Drosophila tau (dTau) is a true vertebrate tau ortholog as it interacts with the neuronal microtubule and actin cytoskeleton. -
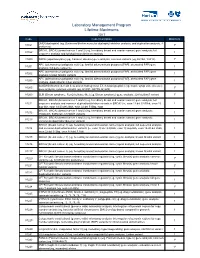
Laboratory Management Program Lifetime Maximums
Laboratory Management Program Lifetime Maximums 2017 Code Code Description Maximum DMD (dystrophin) (eg, Duchenne/Becker muscular dystrophy) deletion analysis, and duplication analysis, if 81161 1* performed BRCA1, BRCA2 (breast cancer 1 and 2) (eg, hereditary breast and ovarian cancer) gene analysis; full 81162 1 sequence analysis and full duplication/deletion analysis 81200 ASPA (aspartoacylase) (eg, Canavan disease) gene analysis, common variants (eg, E285A, Y231X) 1* APC (adenomatous polyposis coli) (eg, familial adenomatosis polyposis [FAP], attenuated FAP) gene 81201 1 analysis; full gene sequence APC (adenomatous polyposis coli) (eg, familial adenomatosis polyposis [FAP], attenuated FAP) gene 81202 1 analysis; known familial variants APC (adenomatous polyposis coli) (eg, familial adenomatosis polyposis [FAP], attenuated FAP) gene 81203 1 analysis; duplication/deletion variants BCKDHB (branched-chain keto acid dehydrogenase E1, beta polypeptide) (eg, maple syrup urine disease) 81205 1* gene analysis, common variants (eg, R183P, G278S, E422X) 81209 BLM (Bloom syndrome, RecQ helicase-like) (eg, Bloom syndrome) gene analysis, 2281del6ins7 variant 1* BRCA1, BRCA2 (breast cancer 1 and 2) (eg, hereditary breast and ovarian cancer) gene analysis; full 81211 sequence analysis and common duplication/deletion variants in BRCA1 (ie, exon 13 del 3.835kb, exon 13 1 dup 6kb, exon 14-20 del 26kb, exon 22 del 510bp, exon BRCA1, BRCA2 (breast cancer 1 and 2) (eg, hereditary breast and ovarian cancer) gene analysis; 81212 1 185delAG, 5385insC, 6174delT -

Cardionext®: Analyses of 92 Genes Associated with Inherited Cardiomyopathies and Arrhythmias
SAMPLE REPORT Ordered By Contact ID:1332810 Org ID:8141 Patient Name: 8911, Test08 Medical Rhodarmer, Jake, MA Accession #: 00-135397 Specimen #: Professional: AP2 Order #: 614269 Specimen: Blood EDTA (Purple Client: MOCKORG44 (10829) top) Birthdate: 09/08/9999 Gender: U MRN #: N/A Collected: N/A Indication: Internal Testing Received: 11/20/2018 CardioNext®: Analyses of 92 Genes Associated with Inherited Cardiomyopathies and Arrhythmias RESULTS SCN5A Variant, Unknown Significance: p.P877R SUMMARY Variant of Unknown Significance Detected INTERPRETATION No known clinically actionable alterations were detected. One variant of unknown significance was detected in the SCN5A gene. Risk Estimate: should be based on clinical and family history, as the clinical significance of this result is unknown. Genetic testing for variants of unknown significance (VUSs) in family members may be pursued to help clarify VUS significance, but cannot be used to identify at-risk individuals at this time. Genetic counseling is a recommended option for all individuals undergoing genetic testing. This individual is heterozygous for the p.P877R (c.2630C>G) variant of unknown significance in the SCN5A gene, which may or may not contribute to this individual's clinical history. Refer to the supplementary pages for additional information on this variant. No additional pathogenic mutations, variants of unknown significance, or gross deletions or duplications were detected. Genes Analyzed (92 total): ABCC9, ACTC1, ACTN2, AKAP9, ALMS1, ALPK3, ANK2, ANKRD1, BAG3, CACNA1C, -

Transcriptomic Causal Networks Identified Patterns of Differential Gene Regulation in Human Brain from Schizophrenia Cases Versus Controls
Transcriptomic Causal Networks identified patterns of differential gene regulation in human brain from Schizophrenia cases versus controls Akram Yazdani1, Raul Mendez-Giraldez2, Michael R Kosorok3, Panos Roussos1,4,5 1Department of Genetics and Genomic Science, Icahn School of Medicine at Mount Sinai, New York, NY, USA 2Lineberger Comprehensive Cancer Center, School of Medicine, University of North Carolina at Chapel Hill, NC, USA 3Department of Biostatistics, University of North Carolina at Chapel Hill, NC, USA 4Department of Psychiatry and Friedman Brain Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA 5Mental Illness Research Education and Clinical Center (MIRECC), James J. Peters VA Medical Center, Bronx, New York, 10468, USA Abstract Common and complex traits are the consequence of the interaction and regulation of multiple genes simultaneously, which work in a coordinated way. However, the vast majority of studies focus on the differential expression of one individual gene at a time. Here, we aim to provide insight into the underlying relationships of the genes expressed in the human brain in cases with schizophrenia (SCZ) and controls. We introduced a novel approach to identify differential gene regulatory patterns and identify a set of essential genes in the brain tissue. Our method integrates genetic, transcriptomic, and Hi-C data and generates a transcriptomic-causal network. Employing this approach for analysis of RNA-seq data from CommonMind Consortium, we identified differential regulatory patterns for SCZ cases and control groups to unveil the mechanisms that control the transcription of the genes in the human brain. Our analysis identified modules with a high number of SCZ-associated genes as well as assessing the relationship of the hubs with their down-stream genes in both, cases and controls. -

Cardiovascular Diseases Genetic Testing Program Information
Cardiovascular Diseases Genetic Testing Program Description: Congenital Heart Disease Panels We offer comprehensive gene panels designed to • Congenital Heart Disease Panel (187 genes) diagnose the most common genetic causes of hereditary • Heterotaxy Panel (114 genes) cardiovascular diseases. Testing is available for congenital • RASopathy/Noonan Spectrum Disorders Panel heart malformation, cardiomyopathy, arrythmia, thoracic (31 genes) aortic aneurysm, pulmonary arterial hypertension, Marfan Other Panels syndrome, and RASopathy/Noonan spectrum disorders. • Pulmonary Arterial Hypertension (PAH) Panel Hereditary cardiovascular disease is caused by variants in (20 genes) many different genes, and may be inherited in an autosomal dominant, autosomal recessive, or X-linked manner. Other Indications: than condition-specific panels, we also offer single gene Panels: sequencing for any gene on the panels, targeted variant • Confirmation of genetic diagnosis in a patient with analysis, and targeted deletion/duplication analysis. a clinical diagnosis of cardiovascular disease Tests Offered: • Carrier or pre-symptomatic diagnosis identification Arrythmia Panels in individuals with a family history of cardiovascular • Comprehensive Arrhythmia Panel (81 genes) disease of unknown genetic basis • Atrial Fibrillation (A Fib) Panel (28 genes) Gene Specific Sequencing: • Atrioventricular Block (AV Block) Panel (7 genes) • Confirmation of genetic diagnosis in a patient with • Brugada Syndrome Panel (21 genes) cardiovascular disease and in whom a specific -

Genetic Testing for Inherited Cardiomyopathies and Channelopathies AHS – M2025
Corporate Medical Policy Genetic Testing for Inherited Cardiomyopathies and Channelopathies AHS – M2025 File Name: genetic_testing_for_inherited_cardiomyopathies_and_channelopathies Origination: 01/2019 Last CAP Review: 04/2021 Next CAP Review: 04/2022 Last Review: 04/2021 Description of Procedure or Service Cardiomyopathies are diseases of the heart muscle. These conditions are frequently genetic and do not include muscle abnormalities caused by coronary artery disease, hypertension, valvular disease, and congenital heart disease. Symptoms include arrhythmia, cardiac dysfunction, and heart failure (Cooper, 2019). Channelopathies, also known as primary electrical disease, are a group of cardiac diseases caused by genetic defects in ion channels of the heart leading to arrhythmias, syncope, and the risk of sudden cardiac death (SCD) (Campuzano, Sarquella-Brugada, Brugada, & Brugada, 2015). Rela ted Policies Cardiovascular Disease Risk Assessment AHS – G2050 ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for genetic testing for cardiomyopathies and channelopathies when it is determined the medical criteria or reimbursement guidelines below are met. Benefits Application This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy. When Genetic Testing for Cardiac Ion Channelopathies is covered 1. Reimbursement for genetic counseling for genetic testing for inherited cardiomyopathies and channelopathies is allowed. Genetic counseling is required for individuals prior to and after undergoing genetic testing for inherited cardiomyopathies and channelopathies for diagnostic, carrier, and/or risk assessment purposes.