Psychology Internship Training Program 2021-2022 VA Eastern
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inventory of Physical Facilities and Space Utilization
INVENTORY OF PHYSICAL FACILITIES AND SPACE UTILIZATION FALL 2014 KANSAS BOARD OF REGENTS INVENTORY OF PHYSICAL FACILITIES AND SPACE UTILIZATION KANSAS BOARD OF REGENTS Kenny Wilk, Chair Shane Bangerter, Vice Chair Joe Bain Ann Brandau-Murguia Bill Feuerborn Fred Logan Robba Moran Zoe Newton Helen Van Etten Dr. Andy Tompkins, President and CEO January 2015 Table of Contents Page No. Table 1 - Area and Replacement Cost of Buildings 1.1 Table 2 - Gross Area of Buildings by Condition Value 1.2 Table 3 - Gross Area of Buildings by Age 1.3 Table 4 - Net Assignable Square Feet by Room Use 1.4 Table 5 - Classroom Utilization 1.5 Table 6 - Laboratory Utilization 1.5 Building Inventory by Institution 1.6-1.34 Appendix 1.35 1/13/2015 Table 1 Fall 2014 Area and Replacement Cost of Buildings Net Number of Total Gross Area Total Net Assignable Area Total Replacement Cost Institution Buildings Gross Area Auxiliary/Other Assignable Area Auxiliary/Other Replacement Cost Auxiliary/Other Acreage ESU 71 1,701,764 547,357 1,082,583 350,473 $433,511,565 $137,855,591 510.95 FHSU 53 2,135,190 148,315 1,341,359 78,243 $562,208,310 $42,976,275 3,964.00 KSU 261 9,209,011 3,447,817 5,733,957 2,022,245 $2,618,289,809 $768,209,415 15,189.92 KU 237 9,568,371 3,799,066 5,750,211 2,125,242 $2,435,423,362 $790,922,621 5,615.11 KU Edwards 4 237,235 19,155 138,630 16,665 $58,777,453 $5,669,880 24.98 KUMC 71 3,236,118 1,106,759 1,238,549 103,966 $808,809,020 $55,288,290 97.64 KUMC Wichita 2 151,822 82,597 $40,592,593 $0 6.94 PSU 83 2,100,937 580,750 1,337,426 348,973 $528,825,574 -

HOUSE RESOLUTION No. 6059 WHEREAS
HOUSE RESOLUTION No. 6059 ARESOLUTION congratulating the University of Kansas for 150 years of outstanding service to the State of Kansas, the United States and the world. WHEREAS, The University of Kansas was founded in 1865 as the State University for the State of Kansas, embodying the values and ideals of the people who fought and died to ensure Kansas would enter the Union as a free State, as symbolized by the university’s mascot, the Jayhawk; and WHEREAS, 150 years after its founding, the University of Kansas is home to 28,000 students and 2,800 faculty, and the university graduates more than 6,700 individuals each year who join the ranks of the 340,000 Jayhawk alumni living throughout Kansas, the United States and the world; and WHEREAS, The University of Kansas has been a member of the prestigious Association of American Universities since 1909; and WHEREAS, The University of Kansas has been open to all genders and races since its founding, and the university’s first valedictorian was Flora Richardson in 1873; and WHEREAS, The University of Kansas has 13 schools and offers more than 600 degree programs. Students come from all 50 States and 105 countries to study at the university; and WHEREAS, The University of Kansas recognizes that the understanding of world cultures is essential for American progress, and the university offers more than 40 separate language courses; and WHEREAS, One of the continuing education programs at the University of Kansas includes fire and law enforcement training centers that annually train over 16,000 -

Campus Parking
9TH ST 9TH ST MASSACHUSETTS ST MASSACHUSETTS ARKANSAS ST ST HAMPSHIRE NEW KENTUCKY ST KENTUCKY VERMONT ST VERMONT CONNECTICUT ST CONNECTICUT RHODE ISLAND ST ISLAND RHODE TENNESSEE ST TENNESSEE NEW YORK ST YORK NEW NEW JERSEY ST JERSEY NEW PENNSYLVANIA ST PENNSYLVANIA DELAWARE ST DELAWARE AVALON RD AVALON 10TH ST MAINE ST MAINE INDIANA ST INDIANA MISSOURI ST MISSOURI ALABAMA ST ALABAMA 10TH ST ILLINOIS ST MISSISSIPPI ST 1 YALE RD GSPH 111 ST OHIO BCST BAHR Sensory E HARVARD RD ZBT M 51 Garden HILLTOP DR HILLTOP E Grace Pearson Scholarship Hall GPH K4 R 111 NORTH & CENTRAL Y 128 Joseph R. Pearson Hall JRP I2 MAXK FAMBROUGH DR R SUNF 111 CORH BUILDING INDEX Joseph R. Pearson Hall JRP I2 D Dennis E. Rieger Scholarship Hall RIEH L4 51 SUDX DISTRICTS Dennis E. Rieger Scholarship Hall RIEH L4 Adams Alumni Center AAC K3 Ritchie Hall Earth, Energy & Environment Center RIT H4 ΑΚΛ 11TH ST Adams Alumni Center AAC K3 Ritchie Hall Earth, Energy & Environment Center RIT H4 11TH ST 65 ПKA Allen Fieldhouse ALLN H6 Robinson Health & Physical Education Center ROB I6 LOUISIANA ST LOUISIANA H Allen Fieldhouse ALLN H6 LLS STAD Robinson Health & Physical Education Center ROB I6 I W H I Allen Fieldhouse Parking Garage G IL H L RR RD CAMPUS WEST Sabatini Multicultural Resource Center SMRC K3 CAMBRIDGE RD H 58 Allen Fieldhouse Parking Garage S W TE 11 Sabatini Multicultural Resource Center SMRC K3 P Parking & Transit AFPK H5 D Self Residence Hall K Kivisto SLFH E5 R 55 Parking & Transit AFPK H5 W Self Residence Hall SLFH E5 FOOT Field David A. -

“Jayhawk Generations,” Kansas Alumni Magazine’S Salute to True Blue Heritage
34 Contents Established in 1902 as The Graduate Magazine FEATURES Citizen Boog 28 His irreverent Costume Party campaign led to one of the most memorable student government elections—and administrations—in KU history. Now the former anarchist with the funny name is mayor of Lawrence. Ladies and gentlemen: Hizzoner, Boog Highberger. BY STEVEN HILL Perfect Form 34 The startling, expressive, fantastical sculptures of graduate student Munira Al-Meer. COVER BY CHRIS LAZZARINO Ice Sages 22 Their work on glacial melting made Prasad Gogineni and Dave Braaten leading experts on polar ice and the threat of sea-level rise. Now they have landed KU its largest grant ever: $19 million to start a National Science Foundation center for ice sheet monitoring. BY MICHAEL CAMPBELL Cover photograph by Earl Richardson 28 Volume 103, No. 3, 2005 America to raise money for football. We provided scholarships for three athletes. Lift the Chorus Unfortunately, World War II came along and we had to stop. In addition, I was drafted into the army. Keep up the good work! Little houses, big stories and music, later to become a noted Saul Kass, b’36 opera singer. To distract me from my Fairway Over the many stage fright, Joyce said, “John, I’m the years I have been only person I know who can sing a Cluck, cluck reading Kansas chord. Wanna hear it?” I admitted that I Alumni (since the did, and she emitted what was unmistak- For years we have been referred to early 1940s) ably a two-note chord, albeit, I think, a mockingly as “chickenhawks” or taunted there have been minor one. -
For Friends of the University of Kansas • Winter 2007
MARCHING JAYHAWKS • KU NATURE RESERVES • DANFORTH CHAPEL FOR FRIENDS OF THE UNIVERSITY OF KANSAS • WINTER 2007 • kuENDOWMENT.ORG BUILDING a greater university: KU Endowment’s VISIONS OF KU mission is to solicit, receive and administer gifts and bequests for the support and advancement of the University of Kansas. WINTER 2007 I VOLUME 1 I NUMBER 3 patterson dd JU David Clemmer directs KU’s athletic bands. Harris’s sparrows visit the KU nature reserves. DEPARTMENTS 12 Marching madness 3 LETTERS With precision and flair, KU’s Marching Jayhawks make spirits rise 4 PRESIDENT’S NOTE and hearts beat faster. Behind the scenes, becoming a great band means long hours, hard work and pure joy. By Charles Higginson 5 EVERY GIFT MATTERS Painting the state blue 6 ACROSS KU 18 A prairie runs through it 26 BE THE DIFFERENCE Donors help protect a native prairie and provide space for future public Lose the holiday shopping blues areas in KU’s Field Station and Ecological Reserves. By Lisa Scheller 27 AMONG FRIENDS 28 BIG PICTURE Grad students tackle the big questions 29 PAST AND PRESENT Danforth Chapel reborn PROFILES 8 WHY I GAVE 23 I AM KU Unconventional medicine EARL RICHARDSON 24 CHANCELLORS CLUB ON THE WEB Photo gallery: Danforth Chapel renovation Ice on the maples at Spooner Hall creates a winter postcard. New and familiar faces kuendowment.org/danforth/ COVER: A drum major leads the KU GIVING Band Day 2007 videos kuendowment.org/band/ Marching Jayhawks down the Memorial KU Giving is published three times a year, in spring, fall and winter, by KU Endowment, the private fundraising Stadium steps and out onto the field. -

Tornado Season on the Way Power of the Citizen by Anne Weltmer Safety Tips [email protected] by Fred A
Baseball defeats Wichita State, 8-2 Delta Chi wins Intramurals title Sophomore outfielder John Allman went Lee Iversen had 21 points in Delta Chi’s 54-35 3-for-5 in the KU victory against Wichita State victory against Phi Psi OHB Wednesday night. Wednesday night. The Jayhawks outhit the Iversen led his team in scoring. PAGE 1B Shockers 15-8 in the victory. PAGE 1B THE STUDENT VOICE SINCE 1904 VOL. 116 ISSUE 121 THURSDAY, MARCH 30, 2006 WWW.KANSAN.COM t OREAD NEIGHBORHOOD t STUDENT SENATE SAAC members Space invaders back candidates BY NICOLE KELLEY ing, it would affect the turn out Bar hoppers [email protected] of the vote. Kansan staff writer During the town hall meeting, occupy spots, the Delta Force coalition also For the first time in Student proposed the idea of creating a Senate election history, the Stu- student athlete senate seat. Jones may face tow dent Athlete Advisory Com- said it was interesting that the mittee will officially pick presi- coalition did that without know- BY MIKE MOSTAFFA dential and vice-presidential ing that SAAC had already gen- [email protected] candidates to support. erated the legislation to do it. Kansan staff writer To help make the decision, “That was cool to see and the committee showed us that When Mikey Munden drives held a town hall ne of our goals they are on the home after a night on the town meeting Mon- exact same page on the weekend, he knows he is day night. The “Othis year in SAAC as us,” Jones in for a long walk. -
National Register Nomination
NPS Form 10-900 OMB No. 1024-0018 (Expires 5/31/2012) United States Department of the Interior National Park Service National Register of Historic Places Registration Form This form is for use in nominating or requesting determinations for individual properties and districts. See instructions in National Register Bulletin, How to Complete the National Register of Historic Places Registration Form. If any item does not apply to the property being documented, enter "N/A" for "not applicable." For functions, architectural classification, materials, and areas of significance, enter only categories and subcategories from the instructions. Place additional certification comments, entries, and narrative items on continuation sheets if needed (NPS Form 10-900a). 1. Name of Property historic name University of Kansas Historic District other names/site number N/A 2. Location Roughly bounded by West Campus Road, the south edge of the N/A street & number buildings on the south side of Jayhawk Boulevard, Sunnyside Avenue, not for publication th Lilac Lane, Oread Avenue, and the topographic line west of West 13 N/A Street city or town Lawrence vicinity state Kansas code KS county Douglas code 045 zip code 66045 3. State/Federal Agency Certification As the designated authority under the National Historic Preservation Act, as amended, I hereby certify that this nomination _ request for determination of eligibility meets the documentation standards for registering properties in the National Register of Historic Places and meets the procedural and professional requirements set forth in 36 CFR Part 60. In my opinion, the property _ meets _ does not meet the National Register Criteria. -
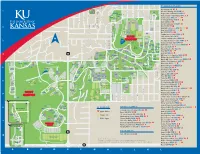
Main Campus West Campus
9th St 9th St Louisiana St Kentucky St Vermont St New Hampshire St Rhode Island St New York York St New Connecticut St New Jersey St Delaware St Pennsylvania St Arkansas St Massachusetts St BUILDING INDEX 10th St 10thAllen St Fieldhouse AL H5 Mississippi St Illinois St Maine St Alabama St Yale Rd Missouri St 1 K.K. AminiTennessee St Scholarship Hall KKAH L4 OLDF GSP Ohio St BH BAHR Sensory Garden Indiana St Margaret Amini Scholarship Hall MAH L3 Havard Rd Anderson Family Football Complex AFFC J2 Avalon Rd d SUNF R KADE 11th St y COR Anschutz Library ANSL I4 r Westdale Rd e SUDX m Art & Design Building A&D I4 E Sunset Dr 11th St Hilltop Dr 11th St Bailey Hall BA J4 H s W H ill MEMS i H g ill rr h s Cambridge Rd W e W Campus Rd Battenfeld Scholarship Hall BATT K4 P T D k w r Blake Hall BL K5 2 y Oxford Rd JRP Budig Hall Hoch Auditoria BUD I4 Oxford Rd Burge Union BURU G5 12th St AFFC Ave Oread Burt Hall BURT G4 Stratford Rd Practice IH Fields Computer Services Facility COMP J5 C-O MAIN Corbin Residence Hall COR L1 N University Dr MSG Crawford Community Center CRAW L4 Spencer Dr N CAMPUS S Potter t a AAC Dole Human Development Center DHDC J5 r 3 i o s Lake n m g i CAMP 13thDouthart St Scholarship Hall DOUT K4 t Iowa St Hillc SMRC r h es Ave t KREH r D D R r SMI WESL Dyche Hall Natural History Museum DYCH K4 r y d D SMA d it al Lawrence Ave R s ri er o Marvin U MAH Eaton Hall EATN H4 iv m RIEG rd n Me o U SRL Grove tf Ellsworth Residence Hall ELLS F6 a r SNOW GPH KKAH t Engel Rd S Jayhawk Blvd Fraser Hall FR K4 LIN MAR ST DYCH SP CRAW Crescent -

Calendar of Events from the University of Kansas
Calendar of Events from the University of Kansas From KU News Service, Office of Public Affairs | http://www.calendar.ku.edu Events for April 23-May 4, 2013 ----------------------------------------------- 23 Tuesday Governance. Faculty Senate Executive Committee. 3 p.m. P Strong Hall. Sponsored by University Governance. Call 785-864-5169. Workshop. Camtasia for Mac: Screen Recording. Workshop. 3 p.m. Budig Media Lab. Sponsored by KU Information Technology. Call 785-864-0410. Concert. KU School of Music Student Recital Series: Lan Jiang, cello, and Soojin Kim, piano. 5 p.m. Swarthout Recital Hall, Murphy Hall. Free. Sponsored by School of Music. Call 785-864-3436. Public Event. Snyder Book Collecting Contest Awards Reception. 5:30 p.m. 3 West, Watson Library. Free. Sponsored by KU Libraries. Call 785-864-8961. Baseball vs. Oral Roberts. 6 p.m. Hoglund Ballpark. Sponsored by Department of Athletics. Call 800-34-HAWKS. Concert. KU School of Music Wind Ensemble. 7:30 p.m. Lied Center. Cost $7 for general admission and $5 for students and seniors. Sponsored by School of Music. Call 785-864-3436. Concert. KU School of Music: Alex Eykamp, organ. 7:30 p.m. Bales Organ Recital Hall. Free. Sponsored by School of Music. Call 785-864-3536. Public Event. “The Environment & Energy: The Role of Free Enterprise & the Government.” Former Congressman Bob Inglis. 7:30 p.m. Dole Institute of Politics. Free. Sponsored by Dole Institute of Politics. Call 785-864-4900. Public Event. “Science on Tap: The Gut Talks, But Does the Liver Listen? The Role of the Gut Microbiome in Alcoholic Liver Disease.” 7:30 p.m. -

Art Goes to War Spencer Exhibition Explores World War I Graphic Arts
No. 2 ■ 2010 Art Goes to War Spencer exhibition explores World War I graphic arts Mini College Boulevard brewer 30 Contents Established in 1902 as The Graduate Magazine FEATURES Back to School 30 The College of Liberal Arts and Sciences’ Mini College draws alumni back to campus for lectures, tours and even another shot at dorm living. And this time there are no tests. BY CHRIS LAZZARINO The Brew Master 34 Boulevard brewery founder John McDonald has blended modern and old-school technologies and techniques to build one of Kansas City’s signature hometown brands. BY STEVEN HILL COVER Into the Void 22 An exhibition at the Spencer Museum of Art takes a new look at the carnage of World War I through the eyes of Europe’s graphic artists. BY CHRIS LAZZARINO Cover art: “Monoplan M.S. attaquant un LVG” (“Monoplane M.S. attacking an LVG”), 1920, by Maurice Busset, courtesy Spencer Museum of Art 34 Volume 108, No. 2, 2010 Lift the Chorus Two Jayhawks set example cow stall would equate with glamour? But for me and many other KU students, Having left the cozy confines of the Shirk’s barn was where the best of KU Medical Center for a new job in college memories were made. Lexington, Ky., just over a year ago, I Mr. Shirk was also a relentless KU cannot tell you how much receiving fan—attending every game for years. He, Kansas Alumni brightens my spirits. The like Avery, led by example. He always publication remains true blue to its had a smile on his face, a kind word to calling—to inspire and share and a loyalty to KU empower Jayhawks around that made you understand the globe. -

Download Danger Copyright Alert System to Battle Online Piracy; Those Caught Illegally Downloading Could Face Consequences
Volume 125 Issue 88 kansan.com Wednesday, March 13, 2013 THE UNIVERSITY DAILY KANSAN PAGE 2 Tyshawn stands up for Elijah Interactive art at Anschutz UDKthe student voice since 1904 PAGE 10 SHIVER ME TIMBERS DOWNLOAD DANGER Copyright Alert System to battle online piracy; those caught illegally downloading could face consequences EMILY DONOVAN er option for students who live regardless of the Copyright Alert [email protected] on campus, is not a part of the System.” Copyright Alert System. At home, Between 1999, the dawn of AT&T, Cablevision, Time however, Sandino’s family sub- peer-to-peer file-sharing, and Warner, Verizon and Comcast are scribes to Time Warner Cable. 2011, music sales in the U.S. have taking long awaited measures to If Sandino ignored six warn- dropped 53 percent, according to address entertainment copyright ings and were to continue ille- the Record Industry Association infringement. Online piracy now gally downloading, one of the pos- of America. faces a battle with the Copyright sible mitigation measures, band- “The music industry — the Alert System, developed by inter- width throttling, would reduce the people who produce and sell the net service providers and copy- Internet speed for Sandino’s entire music — has been decimated by right holders such as the Motion family. Theoretically, this would [illegal downloading],” said Kelly Picture Association of America, leave Sandino to download, his Corcoran, the owner of Love the Recording Industry Association sister to check Facebook, his mom Garden Sounds in Lawrence. “But of America and the National to reply to email and his dad to do they were overpriced for so many Cable and Telecommunications work all at a dial-up speed for one years that it led people to alternate Association. -

Jayhawk Roundup Dinner and Dancing, a Silent Auction Wooed Alumni Buyers, Who Cast Their Bids and Shared Cocktails with KU Friends
Jayhawk Society Membership is a Winning Hand The exceptional loyalty of Jayhawk Society members helps sustain the many programs that fulfill the Association’s mission to serve KU and its alumni. Jayhawk Society members also receive many special benefits: I Distinctive gold lapel pin, vehicle decal, brass key chain, membership card and a unique gift each time you renew.* I Recognition in Kansas Alumni magazine and at the Adams Alumni Center. I 15% discount at the Kansas Union Bookstore (excludes textbooks). I Discounts with select merchants in Lawrence, Kansas City and Topeka. A portion of Jayhawk Society dues is tax deductible and counts toward giving levels at the KU Endowment Association. *This year’s unique gift for renew- Annual Jayhawk Society payments are $100 for single members ing Jayhawk Society members is a and $150 for joint members. Call Bryan Greve at deck of playing cards featuring 785-864-4760 or 800-584-2957 today. the Jayhawks on Parade birds. 22 Contents Established in 1902 as The Graduate Magazine FEATURES Hard Bargain 22 Don Stull enjoys a good hamburger—or brain sandwich— as much as the next guy. He just thinks the social cost of America’s meat and poultry needn’t be so dear. BY STEVEN HILL Laugh Track 26 After stops at “The Late Show With David Letterman” and “Saturday Night Live,” Stewart Bailey found the perfect outlet for his comic sensibility on “The Daily Show With Jon Stewart.” Wanna polish his Emmy? BY SARA ECKEL COVER Stage Presence 18 Intense, funny and seriously talented: Meet Amir Khosrowpour, KU’s first national champion of the piano.