Diagnostic Difficulties in Bacterial Spondylodiscitis Dificuldades Diagnósticas Na Espondilodiscite Bacteriana
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brucellar Spondylodiscitis with Rapidly Progressive Spinal Epidural Abscess Showing Cauda Equina Syndrome
Citation: Spinal Cord Series and Cases (2016) 2, 15030; doi:10.1038/scsandc.2015.30 © 2016 International Spinal Cord Society All rights reserved 2058-6124/16 www.nature.com/scsandc CASE REPORT Brucellar spondylodiscitis with rapidly progressive spinal epidural abscess showing cauda equina syndrome Tan Hu1,2,JiWu1,2, Chao Zheng1 and Di Wu1 Early diagnosis of Brucellosis is often difficult in the patient with only single non-specific symptom because of its rarity. We report a patient with Brucellar spondylodiscitis, in which the low back pain was the only symptom and the magnetic resonance imaging (MRI) showed not radiographic features about infection at initial stage. He was misdiagnosed as a lumbar disc herniation for inappropriate treatment in a long time. The delay in diagnosis and correct treatment led to rapid progression of the disease and severe complications. The patient was treated successfully with triple-antibiotic and surgical intervention in the end. Brucellar spondylodiscitis should always be suspended in the differential diagnosis specially when the patient comes from an endemic area or has consumed dairy products from animals in such an area and comprehensive examination should be done for the patent to rule out some important diseases like Brucellosis with sufficient reasons. Spinal Cord Series and Cases (2016) 2, 15030; doi:10.1038/scsandc.2015.30; published online 7 January 2016 Brucellosis is caused by small, non-motile, Gram-negative, aerobic post meridiem and intermittent left lower limb numbness for the and facultative intracellular coccobacilli of the genus Brucella recent weeks. One week before admission, the patient returned transmitted from infected animals to humans either by to the local clinic because his symptoms worsen. -

Master.Pmd 2
The Effects of Tumor Necrosis Factor Inhibitors in a Particular Association of Psoriatic Arthritis and Behcet Disease ANCA EMANUELA MUSETESCU1#, ALESANDRA FLORESCU2*, ANA-MARIA BUMBEA3#, LUCIAN MIHAI FLORESCU4, PAULINA LUCIA CIUREA1, ANDREI BONDARI4, DAN NICOLAE FLORESCU5, SIMONA BONDARI4 1 University of Medicine and Pharmacy of Craiova,Department of Rheumatology, 2-4 Petru Rares Str., 200349, Craiova, Romania 2University of Medicine and Pharmacy of Craiova, 2-4 Petru Rares Str., 200349, Craiova, Romania 3University of Medicine and Pharmacy of Craiova, Department of Medical Rehabilitation, 2-4 Petru Rares Str., 200349, Craiova, Romania 4 University of Medicine and Pharmacy of Craiova, Department of Radiology and Medical Imaging, 2-4 Petru Rares Str., 200349, Craiova, Romania 5 University of Medicine and Pharmacy of Craiova, Department of Gastroenterology, 2-4 Petru Rares Str., 200349, Craiova, Romania The current case report presents a patient diagnosed with Behcet disease in concurrence with psoriatic arthritis, leading to a complex treatment, difficult management and challenging approach of both rheumatic disorders. After treatment with synthetic disease-modifying drugs and three different TNF inhibitors, the patient developed pulmonary tuberculosis, followed by tuberculosis spondylodiscitis, even after proper anti- tuberculosis therapy. Keywords: Behcet disease, psoriatic arthritis, tuberculosis spondylodiscitis, TNF inhibitors Psoriatic arthritis (PsA) is a chronic inflammatory disease characterized by the presence of both peripheral of uveitis in patients with BD, except for etanercept with joint and axial spine involvement, in concurrence with conflicting results [5]. psoriatic lesions and in the absence of rheumatoid factor. The term PsA comprises one of the five clinical forms: Experimental part symmetrical polyarthritis, asymmetrical oligoarthritis, distal Case report interphalangeal joint involvement, spondylitis and arthritis We present the case of a 34-year old male admitted in mutilans [1]. -
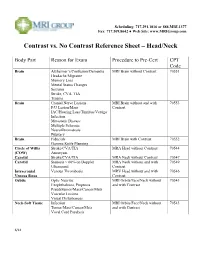
Contrast Vs. No Contrast Reference Sheet – Head/Neck
Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Head/Neck Body Part Reason for Exam Procedure to Pre-Cert CPT Code Brain Alzheimer’s/Confusion/Dementia MRI Brain without Contrast 70551 Headache/Migraine Memory Loss Mental Status Changes Seizures Stroke, CVA, TIA Trauma Brain Cranial Nerve Lesions MRI Brain without and with 70553 F/U Lesion/Mass Contrast IAC/Hearing Loss/Tinnitus/Vertigo Infection Metastatic Disease Multiple Sclerosis Neurofibromatosis Pituitary Brain Fiducials MRI Brain with Contrast 70552 Gamma Knife Planning Circle of Willis Stroke/CVA/TIA MRA Head without Contrast 70544 (COW) Aneurysm Carotid Stroke/CVA/TIA MRA Neck without Contrast 70547 Carotid Stenosis > 60% on Doppler MRA Neck without and with 70549 Ultrasound Contrast Intracranial Venous Thrombosis MRV Head without and with 70546 Venous Sinus Contrast Orbits Optic Neuritis MRI Orbits/Face/Neck without 70543 Exophthalmos, Proptosis and with Contrast Pseudotumor/Mass/Cancer/Mets Vascular Lesions Visual Disturbances Neck-Soft Tissue Infection MRI Orbits/Face/Neck without 70543 Tumor/Mass/Cancer/Mets and with Contrast Vocal Cord Paralysis 6/14 Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Spine Body Part Reason for Exam Procedure to Pre-Cert CPT Code Spine: Cervical Degenerative Disease MRI Cervical Spine without Contrast 72141 Disc Herniation Extremity Pain/Weakness Neck Pain Radiculopathy Trauma Spine: -

Case Report Surgical Management of L5-S1 Spondylodiscitis on Previously Documented Isthmic Spondylolisthesis: Case Report and Review of the Literature
Hindawi Case Reports in Surgery Volume 2020, Article ID 1408701, 5 pages https://doi.org/10.1155/2020/1408701 Case Report Surgical Management of L5-S1 Spondylodiscitis on Previously Documented Isthmic Spondylolisthesis: Case Report and Review of the Literature Anthony Lubiato, Guillaume Baucher , Mikael Meyer, and Stéphane Fuentes Department of Adult Neurosurgery, La Timone University Hospital, APHM, Aix Marseille University, 264 Rue Saint Pierre, Marseille 13385, France Correspondence should be addressed to Guillaume Baucher; [email protected] Received 26 June 2019; Accepted 30 October 2019; Published 17 February 2020 Academic Editor: Mario Ganau Copyright © 2020 Anthony Lubiato et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Background. Although lumbar isthmic spondylolisthesis is frequent in the Caucasian population, its association with spondylodiscitis is extremely rare. Case Description. The authors reported the case of a 44-year-old patient affected by pyogenic spondylodiscitis on previously documented isthmic spondylolisthesis at the L5-S1 level. The patient was surgically treated by circumferential arthrodesis combining anterior lumbar interbody fusion (ALIF), followed by L4-S1 percutaneous osteosynthesis using the same anesthesia. Appropriate antibiotherapy to methicillin-susceptible Staphylococcus aureus, found on the intraoperative samplings, -

Surgical Treatment of Spondylodiscitis of the Thoracic and Lumbar Spine
Open Access Austin Neurosurgery: Open Access Research Article Surgical Treatment of Spondylodiscitis of the Thoracic and Lumbar Spine Aleksey Eroshkin1*, Nikolai Rainov2, Dmytro Romanukha1 Abstract 1 Department of Neurosurgery of Central Hospital of Background: The incidence of spondylodiscitis (SD) of different origin is Ministry of Internal Affairs of Ukraine (Central Police increasing in the last decades and its treatment may be difficult and prolonged. Hospital), Kyiv, Ukraine 2MVZ Wirbelsäulenzentrum Taufkirchen, Munich, Methods: All patients presented with SD of different origin and with different Germany degrees of pain and/or neurological deficits. All of them underwent standard posterior transpedicular fixation with debridement and decompression of neural *Corresponding author: Aleksey Eroshkin, Head structures in the spinal canal. In some cases with significant segmental instability, of Department of Neurosurgery of Central Hospital of intervertebral PLIF cages were used in addition to dorsal transpedicular fixation. Ministry of Internal Affairs of Ukraine (Central Police Clinical outcomes were assessed using functional outcome criteria (ASIA and Hospital), 1 Berdychivs’ka Street, Kyiv, 04116, Ukraine VAS scales). The sagittal alignment of the affected segments was evaluated Received: August 05, 2020; Accepted: September 04, preoperatively and postoperatively by measuring the Cobb angle. 2020; Published: September 11, 2020 Results: 47 patients with SD of different origin underwent posterior transpedicular fixation. PLIF cages were used in addition in 12 cases (26%). 31 (66%) of the patients were males and 16 (34%) females. The average age of the male population was 62.3 ± 4.8 years, and of the female population 58.2 ± 5.1 years. 42 of these patients completed follow-up at 12 months (89.4%). -

Cervical Neck Pain Or Cervical Radiculopathy
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Cervical Neck Pain or Cervical Radiculopathy Variant 1: New or increasing nontraumatic cervical or neck pain. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level Radiography cervical spine Usually Appropriate ☢☢ MRI cervical spine without IV contrast May Be Appropriate (Disagreement) O CT cervical spine without IV contrast May Be Appropriate ☢☢☢ CT cervical spine with IV contrast Usually Not Appropriate ☢☢☢ MRI cervical spine without and with IV Usually Not Appropriate contrast O CT cervical spine without and with IV Usually Not Appropriate contrast ☢☢☢ CT myelography cervical spine Usually Not Appropriate ☢☢☢☢ CTA neck with IV contrast Usually Not Appropriate ☢☢☢ Discography cervical spine Usually Not Appropriate ☢☢ Facet injection/medial branch block cervical Usually Not Appropriate spine ☢☢ MRA neck with IV contrast Usually Not Appropriate O MRA neck without IV contrast Usually Not Appropriate O MRI cervical spine with IV contrast Usually Not Appropriate O Bone scan whole body with SPECT or Usually Not Appropriate SPECT/CT neck ☢☢☢ X-ray myelography cervical spine Usually Not Appropriate ☢☢☢ ACR Appropriateness Criteria® 1 Cervical Neck Pain or Cervical Radiculopathy Variant 2: New or increasing nontraumatic cervical radiculopathy. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level MRI cervical spine without IV contrast Usually Appropriate O CT cervical spine without IV contrast -

Dutch Multidisciplinary Guideline for Invasive Treatment of Pain Syndromes of the Lumbosacral Spine
ORIGINAL ARTICLE Dutch Multidisciplinary Guideline for Invasive Treatment of Pain Syndromes of the Lumbosacral Spine Coen J. Itz, MD*,†; Paul C. Willems, MD, PhD‡; Dick J. Zeilstra, MD, PhD§; Frank J. Huygen, MD, PhD, FIPP¶ *Department of Anesthesiology, Erasmus Medical Center, Rotterdam; †Health Insurance Company VGZ Eindhoven, Eindhoven; ‡Department of Orthopedic Surgery, Maastricht University Medical Centre, Maastricht; §Neurosurgery, Nedspine Ede and Bergman Clinics Naarden, Ede and Naarden; ¶Department of Anesthesiology, Centre of Pain Medicine, Erasmus Medical Center, Rotterdam, the Netherlands & Abstract Evaluation system. For the evaluation of invasive treatment options, the guideline committee decided that the outcome Objectives: When conservative therapies such as pain med- measures of pain, function, and quality of life were most ication or exercise therapy fail, invasive treatment may be important. indicated for patients with lumbosacral spinal pain. The Results: The definition, epidemiology, pathophysiological Dutch Society of Anesthesiologists, in collaboration with the mechanism, diagnostics, and recommendations for invasive Dutch Orthopedic Association and the Dutch Neurosurgical therapy for each of the spinal back pain syndromes are Society, has taken the initiative to develop the guideline reported. “Spinal low back pain,” which describes the evidence Discussion: The guideline committee concluded that the regarding diagnostics and invasive treatment of the most categorization of low back pain into merely specific or common spinal low back pain syndromes, that is, facet joint nonspecific gives insufficient insight into the low back pain pain, sacroiliac joint pain, coccygodynia, pain originating problem and does not adequately reflect which therapy is from the intervertebral disk, and failed back surgery syn- effective for the underlying disorder of a pain syndrome. -

Acute Calcific Discitis with Intravertebral Disc Herniation in the Dorsolumbar Spine
Published online: 2021-08-02 MUSCULOSKELETAL Case report: Acute calcific discitis with intravertebral disc herniation in the dorsolumbar spine Puneet Mittal, Kavita Saggar, Parambir Sandhu, Kamini Gupta Department of Radiodiagnosis, Dayanand Medical College & Hospital, Ludhiana, Punjab, India Correspondence: Dr. Puneet Mittal, Department of Radiodiagnosis, Dayanand Medical College & Hospital, Tagore Nagar, Civil Lines, Ludhiana, Punjab - 141 001, India. E-mail: [email protected] Abstract Acute calcific discitis is a rare but well-known condition of unknown etiology. In symptomatic cases, the most common site is the cervical spine. We describe the CT scan and MRI findings in a symptomatic patient, with a lesion in the dorsolumbar spine. Key words: Acute; calcific; discitis; dorsolumbar; MR Introduction Acute calcifc discitis is a rare condition. When symptomatic, it can be mistaken for infection.[1] Most of the symptomatic cases present in the cervical spine.[1-3] We present the CT scan and MRI findings in a patient who had involvement of the dorsolumbar spine, with associated intravertebral disc herniation. Case Report A 10-year-old boy presented with a 2-week history of pain in the lower back following a yoga session in school. The pain had gradually worsened over the last 5 days. The patient was afebrile. The total white blood cell (WBC) count was normal. The erythrocyte sedimentation rate (ESR) was raised (52 mm/h). The Mantoux test was negative. A radiograph obtained elsewhere and repeated a day after the MRI [Figure 1], showed calcification of the D12-L1 intervertebral disc. MRI showed hypointense signal in the D12-L1 intervertebral disc on T1W [Figure 2A] and T2W [Figure 2B and C] images. -

Cervical Spondylodiscitis in an Infant with Torticollis
Cervical Spondylodiscitis in IMAGES IN CLINICAL an Infant with Torticollis RADIOLOGY BRECHT VAN BERKEL KRISTIN SUETENS LUC BREYSEM *Author affiliations can be found in the back matter of this article ABSTRACT CORRESPONDING AUTHOR: Brecht Van Berkel Teaching point: Narrowing of the intervertebral space and destruction of the adjacent UZ Leuven, BE vertebral end plates on conventional radiography or CT should raise suspicion for brecht.vanberkel@student. spondylodiscitis in symptomatic infants. kuleuven.be KEYWORDS: Spondylodiscitis; MRI; pediatric; torticollis; cervical; CT TO CITE THIS ARTICLE: Van Berkel B, Suetens K, Breysem L. Cervical Spondylodiscitis in an Infant with Torticollis. Journal of the Belgian Society of Radiology. 2021; 105(1): 35, 1–4. DOI: https://doi.org/10.5334/ jbsr.2454 Van Berkel et al. Journal of the Belgian Society of Radiology DOI: 10.5334/jbsr.2454 2 CASE REPORT disc space and loss of height of vertebral bodies C3 and C4 and irregular alignment of the end plates. On An eight-month-old infant presented at the emergency the sagittal T1-weighted Short-tau inversion-recovery department with a history of torticollis for six weeks. (STIR) images, the hyperintense signal in the vertebral Blood results showed no elevated inflammatory bodies of C3 and C4, as well as in the surrounding tissues parameters. Vertical lateral X-ray of the cervical spine (arrowheads) were compatible with a widespread area demonstrated a kyphotic angulation at the level of C3– of bone and soft tissue oedema (Figure 2). There were C4, narrowing of the intervertebral disc space, irregular no diffusion-restricted areas and no accompanying fluid end plates, and loss of height of the vertebral body of collections. -

Characteristics, Management and Outcomes of Spondylodiscitis in Children: a Systematic Review
antibiotics Review Characteristics, Management and Outcomes of Spondylodiscitis in Children: A Systematic Review Irene Ferri 1, Gabriele Ristori 2, Catiuscia Lisi 1, Luisa Galli 1 and Elena Chiappini 1,* 1 Paediatric Infectious Disease Unit, Meyer Children’s University Hospital, Department of Health Sciences, University of Florence, 50139 Florence, Italy; [email protected]fi.it (I.F.); [email protected] (C.L.); luisa.galli@unifi.it (L.G.) 2 Paediatric Orthopaedic and Traumatology Department, Meyer Children’s University Hospital, Department of Health Sciences, University of Florence, 50139 Florence, Italy; [email protected] * Correspondence: elena.chiappini@unifi.it; Tel.: +39-0-555-662-480 Abstract: Spondylodiscitis (SD) is the concurrent infection of the intervertebral disc and the adjacent vertebral bodies. Currently, there is a substantial lack of structured reviews about this topic. The aim of this study was to systematically review the available literature in order to determine the main features of pediatric SD. A systematic search of MEDLINE database was performed, according to the PRISMA guideline recommendations. Clinical features, laboratory data, radiological signs, treatments strategies, and outcomes were summarized. Studies’ quality assessments were performed using the JBI Critical Appraisal Checklists. A total of 35 retrospective studies were analyzed and 340 children were identified. The most frequently affected age class was 0.5–4 years. The most affected site was the lumbar spine. The most commonly reported symptoms were back pain (37.97%) and refusal to walk/to stand/to sit (49.79%). The most frequently identified pathogen was Staphylococcus aureus (n = 33). The most used antibiotics were third generation cephalosporins. -

Spondt (Spondylodiscitis Diagnosis and Treatment): Spondylodiscitis Scoring System Lars Homagk1,4* , Daniel Marmelstein2, Nadine Homagk2 and Gunther O
Homagk et al. Journal of Orthopaedic Surgery and Research (2019) 14:100 https://doi.org/10.1186/s13018-019-1134-9 RESEARCH ARTICLE Open Access SponDT (Spondylodiscitis Diagnosis and Treatment): spondylodiscitis scoring system Lars Homagk1,4* , Daniel Marmelstein2, Nadine Homagk2 and Gunther O. Hofmann3 Abstract Background: Spondylodiscitis is a chameleon among infectious diseases due to the lack of specific symptoms with which it is associated. It is nevertheless a serious infection, with 7% mortality of hospitalized patients, in large part because of delayed diagnosis. The aim of this study was to develop a diagnosis and course-of-disease index to optimize its treatment. Material and methods: Through analysis of 296 patients between January 1998 and December 2013, we developed a scoring system for spondylodiscitis, which we term SponDT (Spondylodiscitis Diagnosis and Treatment) based on three traits: (1) the inflammatory marker C-reactive protein (CRP) (mg/dl), (2) pain according to a numeric rating scale (NRS) and (3) magnetic resonance imaging (MRI), to monitor its progression following treatment. Results: The number of patients receiving treatment increased over the past 15 years of our study. We also found an increasing age of patients at the point of diagnosis across the study, with an average age of 67.7 years. In 34% of patients, spondylodiscitis developed spontaneously. Almost 70% of them did not receive treatment until the first diagnosis using SponDT. Following treatment against spondylodiscitis, pain intensity decreased from 6.0 to 3.1 NRS. The inflammatory markers also decreased (CRP from 119.2 to 46.7 mg/dl). Similarly, MRI revealed a regression in inflammation following treatment. -
Spondyloarthropathies and Reactive Arthritis
RHEUMATOLOGY SPONDYLOARTHRITIS ROBERT L. DIGIOVANNI, DO, FACOI PROGRAM DIRECTOR LMC RHEUMATOLOGY FELLOWSHIP [email protected] DISCLOSURES •NONE SERONEGATIVE SPONDYLOARTHROPATHIES SLIDES PREPARED BY GENE JALBERT, DO SENIOR RHEUMATOLOGY FELLOW THE SPONDYLOARTHROPATHIES: • Ankylosing Spondylitis (A.S.) • Non-radiographic Axial spondyloarthropathies (nr-axSpA) • Psoriatic Arthritis (PsA) • Inflammatory Bowel Disease Associated (Enteropathic) • Crohn and Ulcerative Colitis • +/- Microscopic colitis • Reactive Arthritis (ReA) • Juvenile-Onset SpA • Others: Bechet’s dz, Celiac, Whipples, pouchitis. THE FAMOUS VENN DIAGRAM: SPONDYLOARTHROPATHY: • First case of Axial SpA was reported in 1691 however some believe Ramses II has A.S. • 2.4 million adults in the United States have Seronegative SpA • Compare with RA, which affects about 1.3 million Americans • Prevalence variation for A.S.: Europe (0.12-1%), Asia (0.17%), Latin America (0.1%), Africa (0.07%), USA (0.34%). • Pathophysiology in general: • Responsible Interleukins: IL-12, IL17, IL-22, and IL23. SPONDYLOARTHROPATHY: • Axial SpA: • Radiographic (Sacroiliitis seen on X- ray) • No Radiographic features non- radiographic SpA (nr-SpA) • Nr-SpA was formally known as undifferentiated SpA • Peripheral SpA: • Enthesitis, dactylitis and arthritis • Eventually evolves into a specific diagnosis A.S., PsA, etc. • Can be a/w IBD, HLA-B27 positivity, uveitis SHARED CLINICAL FEATURES: • Axial joint disease (especially SI joints) • Asymmetrical Oligoarthritis (2-4 joints). • Dactylitis (Sausage