Prevalence of Anaemia and Associated Risk Factors Among
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CARE for PEOPLE LIVING with DISABILITIES in the WEST NILE REGION of UGANDA:: 7(3) 180-198 UMU Press 2009
CARE FOR PEOPLE LIVING WITH DISABILITIES IN THE WEST NILE REGION OF UGANDA:: 7(3) 180-198 UMU Press 2009 CARE FOR PEOPLE LIVING WITH DISABILITIES IN THE WEST NILE REGION OF UGANDA: EX-POST EVALUATION OF A PROGRAMME IMPLEMENTED BY DOCTORS WITH AFRICA CUAMM Maria-Pia Waelkens#, Everd Maniple and Stella Regina Nakiwala, Faculty of Health Sciences, Uganda Martyrs University, P.O. Box 5498 Kampala, Uganda. #Corresponding author e-mail addresses: [email protected]; [email protected]; [email protected] Abstract Disability is a common occurrence in many countries and a subject of much discussion and lobby. People with disability (PWD) are frequently segregated in society and by-passed for many opportunities. Stigma hinders their potential contribution to society. Doctors with Africa CUAMM, an Italian NGO, started a project to improve the life of PWD in the West Nile region in north- western Uganda in 2003. An orthopaedic workshop, a physiotherapy unit and a community-based rehabilitation programme were set up as part of the project. This ex-post evaluation found that the project made an important contribution to the life of the PWD through its activities, which were handed over to the local referral hospital for continuation after three years. The services have been maintained and their utilisation has been expanded through a network of outreach clinics. Community-based rehabilitation (CBR) workers mobilise the community for disability assessment and supplement the output of qualified health workers in service delivery. However, the quality of care during clinics is still poor on account of large numbers. In the face of the departure of the international NGO, a new local NGO has been formed by stakeholders to take over some functions previously done by the international NGO, such as advocacy and resource mobilisation. -

Ministry of Health
UGANDA PROTECTORATE Annual Report of the MINISTRY OF HEALTH For the Year from 1st July, 1960 to 30th June, 1961 Published by Command of His Excellency the Governor CONTENTS Page I. ... ... General ... Review ... 1 Staff ... ... ... ... ... 3 ... ... Visitors ... ... ... 4 ... ... Finance ... ... ... 4 II. Vital ... ... Statistics ... ... 5 III. Public Health— A. General ... ... ... ... 7 B. Food and nutrition ... ... ... 7 C. Communicable diseases ... ... ... 8 (1) Arthropod-borne diseases ... ... 8 (2) Helminthic diseases ... ... ... 10 (3) Direct infections ... ... ... 11 D. Health education ... ... ... 16 E. ... Maternal and child welfare ... 17 F. School hygiene ... ... ... ... 18 G. Environmental hygiene ... ... ... 18 H. Health and welfare of employed persons ... 21 I. International and port hygiene ... ... 21 J. Health of prisoners ... ... ... 22 K. African local governments and municipalities 23 L. Relations with the Buganda Government ... 23 M. Statutory boards and committees ... ... 23 N. Registration of professional persons ... 24 IV. Curative Services— A. Hospitals ... ... ... ... 24 B. Rural medical and health services ... ... 31 C. Ambulances and transport ... ... 33 á UGANDA PROTECTORATE MINISTRY OF HEALTH Annual Report For the year from 1st July, 1960 to 30th June, 1961 I.—GENERAL REVIEW The last report for the Ministry of Health was for an 18-month period. This report, for the first time, coincides with the Government financial year. 2. From the financial point of view the year has again been one of considerable difficulty since, as a result of the Economy Commission Report, it was necessary to restrict the money available for recurrent expenditure to the same level as the previous year. Although an additional sum was available to cover normal increases in salaries, the general effect was that many economies had to in all be made grades of staff; some important vacancies could not be filled, and expansion was out of the question. -

Report on Five Years of Operation of Leprosy Control Scheme in The
FIVE YEARS OPERATION OF A LEPROSY CONTROL SCHEME 2 J9 Report on Five Years of Operation of a Leprosy Control Scheme in the West Nile District of .Uganda DR. E. H. WILLIAMS Kuluva Hospital, Arua, Uganda In the latter half of J 958 the West Nile District Council introduced Bye-Laws to control leprosy. Basically these were very simple, consisting of rules to compel people thought to be suffering from leprosy to attend fo r examination and diagnosis, and to make it compulsory fo r persons diagnosed as having leprosy to attend fo r treatment. There were also provisions to try and segregate people with the more infective fo rms of leprosy, termed 'contagious cases'. These rules being in the fo rm of Bye Laws there was of necessity a punishment inserted, namely a fine of ten shillings only. This fine has been applied on relatively fe w occasions. These Bye-Laws were introduced to a background of one large lepro sarium with 400 places at Kuluva, one small leprosarium at Wandi, and 3 outpatient clinics. In order to implement the Bye-Laws a Committee of local Government Medical Officers and Mission Doctors met and agreed to increase the number cf outpatient clinics to all the Government Dis pensaries in the West Nile. In this way an immediate potential coverage of the population to nine-tenths was effected. A uniform system of regis tration, examination and treatment with Dapsone of all patients was worked out. From the result of two surveys carried out by the Leprologist of Uganda, DR. J. -
Usaid/Uganda Private Health Support Program (June 2013-June 2018)
USAID/UGANDA PRIVATE HEALTH SUPPORT PROGRAM (JUNE 2013-JUNE 2018) FINAL REPORT Contract No.: AID-617-C-13-00005 C Mothers and infants awaiting treatment at St Francis Health Care Services in Njeru (January 2018) September 2018 This report is made possible by the support of the American People through the United States Agency for International Development (USAID). The contents of this report are the sole responsibility of Cardno Emerging Markets USA, Ltd. and do not necessarily reflect the views of USAID or the United States Government. USAID/UGANDA PRIVATE HEALTH SUPPORT PROGRAM (JUNE 2013-JUNE 2018) FINAL REPORT Submitted by: Cardno Emerging Markets USA, Ltd. Submitted to: USAID/Uganda Contract No.: AID-617-C-13-00005 DISCLAIMER The author’s views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development or the United States Government. USAID/Uganda Private Health Support Program Table of Contents ACRONYMS ............................................................................................................................................................. III EXECUTIVE SUMMARY ........................................................................................................................................... 1 CONTEXTUAL OVERVIEW ..................................................................................................................................... 4 PROGRAM OBJECTIVES ........................................................................................................................................... -

List of Authorised Facilities As of 30/1/2019
LIST OF AUTHORISED FACILITIES AS OF 30/1/2019 EXECUTIVE SUMMARY Atomic Energy Council is a body corporate established by the Atomic Energy Act (AEA), 2008, Act No.24, Cap.143 Laws of Uganda to regulate the peaceful applications of ionising radiation, to provide for the protection and safety of individuals, society and the environment from the dangers resulting from ionising radiation. Section 32 (1) of Atomic Energy Act No. 24 of 2008 requires facilities with practices involving ionizing radiation not to acquire, own, possess, operate, import, export, hire, loan, receive, use, install, commission, decommission, transport, store, sell, distribute, dispose of, transfer, modify, upgrade, process, manufacture or undertake any practice related to the application of atomic energy unless permitted by an authorization from Atomic Energy Council. # Facility Name Type of status District Licensed Machine/ License Number Date of Date of Facility radioactive sources Issue Expiry 1. Abii Clinic Medical Private Kampala Dental X-ray (OPG) AEC/PU/1409 11/04/2017 10/04/2019 Fixed X-ray AEC/PU/1090/02 25/01/2018 24/01/2020 Fixed Dental X-ray AEC/PU/1265/01 30/4/2018 29/4/2020 2. Abubaker Technical Services and Industrial Private Mukono 1 Nuclear gauge AEC/PU/1323/01 04/10/2018 03/10/2020 General Supplies Limited 3. Adjumani General Hospital Medical Government Adjumani Fixed X-ray AEC/PU/1515 17/11/2017 16/11/2019 4. AFYA Medical & Diagnostic Centre Medical Private Kasese AEC/PU/1024/03 18/12/2018 17/12/2020 5. Agakhan University Hospital-Acacia Medical Private Kampala Fixed Dental X-ray AEC/PU/1229/01 23/01/2018 22/01/2020 Medical Centre Fixed X-ray AEC/PU/1134/02 10/10/2018 09/10/2020 6. -

Hinari Participating Academic Institutions
Hinari Participating Academic Institutions Filter Summary Country City Institution Name Afghanistan Bamyan Bamyan University Chakcharan Ghor province regional hospital Charikar Parwan University Cheghcharan Ghor Institute of Higher Education Faizabad, Afghanistan Faizabad Provincial Hospital Ferozkoh Ghor university Gardez Paktia University Ghazni Ghazni University Ghor province Hazarajat community health project Herat Rizeuldin Research Institute And Medical Hospital HERAT UNIVERSITY 19-Dec-2017 3:13 PM Prepared by Payment, HINARI Page 1 of 367 Country City Institution Name Afghanistan Herat Herat Institute of Health Sciences Herat Regional Military Hospital Herat Regional Hospital Health Clinic of Herat University Ghalib University Jalalabad Nangarhar University Alfalah University Kabul Kabul asia hospital Ministry of Higher Education Afghanistan Research and Evaluation Unit (AREU) Afghanistan Public Health Institute, Ministry of Public Health Ministry of Public Health, Presidency of medical Jurisprudence Afghanistan National AIDS Control Program (A-NACP) Afghan Medical College Kabul JUNIPER MEDICAL AND DENTAL COLLEGE Government Medical College Kabul University. Faculty of Veterinary Science National Medical Library of Afghanistan Institute of Health Sciences Aga Khan University Programs in Afghanistan (AKU-PA) Health Services Support Project HMIS Health Management Information system 19-Dec-2017 3:13 PM Prepared by Payment, HINARI Page 2 of 367 Country City Institution Name Afghanistan Kabul National Tuberculosis Program, Darulaman Salamati Health Messenger al-yusuf research institute Health Protection and Research Organisation (HPRO) Social and Health Development Program (SHDP) Afghan Society Against Cancer (ASAC) Kabul Dental College, Kabul Rabia Balkhi Hospital Cure International Hospital Mental Health Institute Emergency NGO - Afghanistan Al haj Prof. Mussa Wardak's hospital Afghan-COMET (Centre Of Multi-professional Education And Training) Wazir Akbar Khan Hospital French Medical Institute for children, FMIC Afghanistan Mercy Hospital. -

Medical Providers Panel Uganda
MEDICAL PROVIDERS PANEL UGANDA www.jubileeinsurance.com 1 JUBILEE INSURANCE UPDATED SERVICE PROVIDER LIST 2021 KAMPALA & SURROUNDING ALL SPECIALITIES: PEADIATRICS, OBS & GYN, ORTHOPAEDICS, RADIOLOGY, ENT, DERMATOLOGY, INTERNAL MEDICINE ETC OPERATING LOCATION PROVIDER ADRESS SERVICES CONTACT PERSON EMAIL TELEPHONE TIMES In & Out- 0414-34 6772 / Norvik Hospital & [email protected]/info Bombo Rd Plot 13, Bombo Rd Patient 24/7 Salama/Isaac 0705631550/07757977 Research Centre Ltd @[email protected] 86 In & Out- 0414 345 Savannah Sunrise Shoal House Bombo Rd. Patient 24/7 Paul/ Dr.Grace Kaisa [email protected] 325/0704709074/0772 Medical Center Bombo Rd. 465409 In & Out- 0414250362/03122507 Buganda Case Medical Plot 69/71 Dr. Sebbale A [email protected] Patient 24/7 00/0701 111 122/0701 Road Centre Buganda Road Kato/Osinde/Denis g 111 161 In & Out- 0414231534/04142581 Buganda Plot 83 Buganda Dr. Kajumba/Asia/ St Catherine's Clinic Patient 24/7 [email protected] 08/0704 986 858/0789 Road Road Marion 769 582 Buganda Platinum Medical Plot 113 Buganda In & Out- [email protected] 0392176915/07520168 24/7 Dr. Ssekabira Road Centre Road Patient om 72/0774446825 In & Out- 0772436228/ Bugolobi Medical 134 Spring Rd, Bugolobi Patient 24/7 Dr.Kawanguzi /Gilbert [email protected] 0703284309/04142223 Centre Bugolobi 54 Kampala Hospital Plot 6 Makindu In & Out- [email protected]/billi 0776433199/03125634 Kololo 24/7 Catherine/ Kawalya Ltd Close, Kololo Patient [email protected] 00/ 0414255006 -
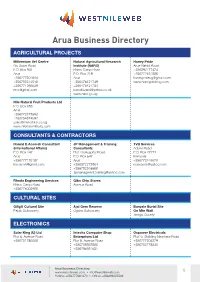
Arua Business Directory.Indd
Arua Business Directory AGRICULTURAL PROJECTS Millennium Vet Centre Natural Agricultural Research Honey Pride Go Down Road Institute (NARO) Arua-Nebbi Road P.O. Box 941 Rhino Camp Road +256392177474 Arua P.O. Box 219 +256772451586 +256777301694 Arua [email protected] +256785514518 +256476421749 www.honeyprideug.com +256771296029 +256476421734 [email protected] [email protected] www.naro.go.ug Nile Natural Fruit Products Ltd P.O. Box 685 Arua +256772373692 +256754374692 [email protected] www.nilenaturalfruits.com CONSULTANTS & CONTRACTORS Harold E.Acemah Consultant JP Management & Training TVB Services (International Affairs) Consultants Adumi Road P.O. Box 147 Plot 10,Hospital Road P.O. Box 27772 Arua P.O. Box 647 Kampala +256777175187 Arua +256772446676 [email protected] +256372273964 [email protected] +256782346688 [email protected] Rhoda Engineering Services Gibo Chip Stores Rhino Camp Road Avenue Road +256776002988 CULTURAL SITES Giligili Cultural Site Ajai Gem Reserve Banyale Burial Site Pajulu Subcounty Ogoko Subcounty On Mtn Wati Terego County ELECTRONICS Solar King (U) Ltd Intechs Computer Shop Ospower Electricals Plot 6, Avenue Road Enterprises Ltd Plot14, Building New lane Road +256751786008 Plot 8, Avenue Road +256777204279 +256758353856 +256752778540 +256786931631 Arua Business Directory www.westnileweb.com • [email protected] 1 Hotline: +256777681670 • Office: +256393225533 Metro Electronics Arua Phones Service Centre Aliza Electronic Ltd Plot 10, Duka Road Plot12, Avenue Road Avenue Road +256702144786 +256772822122 +256715089299 +256713144786 Holly Wood Electronics (U) Roman Electronics (U) Ltd Plot1- 3, Adumi Road Adumi Road +256713144786 +256778134910 FINANCIAL INSTITUTIONS Centenary Bank Stanbic Bank Bank of Africa Plot 3, Avenue Road Avenue Road Plot 19, Avenue Road P.O. -

List of Villages and Parishes for Residual Elections July 2019 For
LIST OF 149 VILLAGES & 13 PARISHES WHERE LC 1 & II RESIDUAL ELECTIONS ARE TO BE HELD, 2019 No District Subcounty Parish Village Reason for Failure 1 LIRA ADEKOKWOK BOROBORO EAST BOROBORO EAST NO NOMINATION 2 LIRA ADYEL TESO A MEDICAL QUARTERS NO NOMINATION 3 MITYANA CENTRAL DIVISION CENTRAL WARD HOSPITAL AREA NO NOMINATION 4 KYENJOJO KANYEGARAMIRE KITEGA KITEGA NO NOMINATION 5 BUNDIBUGYO BUTAMA-MITUNDA T/C BUNDINJONGYA WARD BUNDINJONGYA NO NOMINATION 6 BUNDIBUGYO BUTAMA-MITUNDA T/C KAHIMBI WARD BUNSERU NO NOMINATION 7 KYENJOJO BUFUNJO KANDAMA MUZIZI NO NOMINATION 8 LIRA ADYEL AKWOYO WARD LANGO COLLEGE NO NOMINATION 9 LIRA AMACH ABWOCOLIL WIODYEK A NO NOMINATION 10 KYEGEGWA KYEGEGWA TOWN COUNCIL KYEGEGWA WARD KIGANDO NO NOMINATION 11 BUKWO CHESOWER NYALIT KAPSIYWO NO NOMINATION 12 BUKWO CHESOWER NYALIT NYALIT NO NOMINATION 13 BUKWO CHESOWER KAPTEKA CHERINGANY NO NOMINATION 14 BUKWO CHESOWER KAPTEKA KWANWA NO NOMINATION 15 BUKWO CHESOWER KAPTEKA LOCH NO NOMINATION 16 BUKWO CHESOWER KAPTEKA TAKATET NO NOMINATION 17 BUKWO CHESOWER KAPTEKA RWANDET NO NOMINATION 18 KABAROLE BUKUUKU KIGUMA KALYANGO NO NOMINATION 19 KABAROLE HARUGONGO BUSAIGA WANKA NO NOMINATION 20 KABAROLE HARUGONGO KYAKAIGO KIKONGE B NO NOMINATION 21 KASESE MALIBA KATEBE KIHYO NO NOMINATION 22 BUKWO CHESOWER KAPTEKA BOYET NO NOMINATION 23 BUKWO CHESOWER KAPTEKA TUYOBEI NO NOMINATION 24 BUKWO CHEPKWASTA SUNGORA SUNGORA NO NOMINATION 25 BUKWO CHEPKWASTA SUNGORA KAPSOYEN NO NOMINATION 26 BUKWO CHEPKWASTA SUNGORA SURUMOYO NO NOMINATION 27 BUKWO CHEPKWASTA SUNGORA CHEMUGUN NO NOMINATION 28 BUKWO CHEPKWASTA SUNGORA MURYAMAT NO NOMINATION 29 BUKWO CHEPKWASTA SUNGORA CHEMURON NO NOMINATION 30 BUKWO KAMET KAMET TOMTO NO NOMINATION 31 KOBOKO DRANYA ALLA LEMEKORA NO NOMINATION 32 KOBOKO LUDARA CHAKULIA GIDOGIDONGA NO NOMINATION 33 NAKASEKE KINYOGOGA RUKONO SPECIAL AREA/BARRACKS NO NOMINATION 34 ALEBTONG AWEI ACEDE AKOKOWO A NO NOMINATION 35 ARUA ADUMI ANYARA ADUMI S.S. -
Hybrid Etlearning for Rural Secondary Schools In
SECONDARY SCHOOLS IN UGANDA SECONDARY HYBRID E.LEARNING FOR RURAL ABSTRACT For the last two decades, a number of policies ai- months in 2007 and they were independently exa- med at increasing participation of female students mined four times. The repeated measures data HYBRID E-LEARNING FOR RURAL in higher education have been implemented by that were collected were analysed using multilevel Uganda Government. However, the participation methods to establish the effects of the hybrid e- SECONDARY SCHOOLS IN UGANDA of female students in the engineering courses in learning intervention and school contexts on the Makerere University, Uganda’s biggest University, performance of the students in external exami- CO-EVOLUTION IN TRIPLE HELIX PROCESSES has remained between 17% to 20% only. Further- nations. more, over 90% of the female engineering stu- dents are from the ‘elite’ and advantaged urban Results of the analysis showed that, 41% of the schools located in the capital city, Kampala, and its students passed and were eligible for university surrounding Districts of Mukono and Wakiso. Ru- admission. Furthermore, it was found that within- ral secondary schools perform poorly in Physics student factors were chiefly responsible for the and Mathematics; the key technology and engine- performance of students in Physics, while for Mat- ering subjects. One rural District, which has failed hematics, the school contexts were more domi- Peter Okidi Lating to send female students to Makerere University nant. However, after extrapolation of the perfor- for engineering training, is Arua- a remote, poor mance of the students over twelve months, up to and insecure District in the West Nile Region of 72% of the students would have passed and be Uganda. -

The Ombaci Massacre: June 24, 1981
It Was Only the Gun Speaking, With a Pool of Blood Flowing The Ombaci Massacre: June 24, 1981 JRP Field Note 20, June 2014 Maps showing Ombaci Mission and St. Josephs College, Arua Figure 1: St. Joseph’s College and Ombaci Catholic Mission. Figure 2: St. Joseph’s College Figure 3: Ombaci Mission About the Justice and Reconciliation Project The Justice and Reconciliation Project (JRP) was established in 2005 in Gulu, Uganda to understand and explain the interests, needs, concerns and views of communities affected by conflict and to promote sustainable peace through the active involvement of war-affected communities in research and advocacy. Find out more about JRP at http://www.justiceandreconciliation.com or email [email protected] All pictures in this publication are courtesy of JRP. © The Justice and Reconciliation Project 2014. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without full attribution. Acknowledgments This Field Note was written by Evelyn Akullo Otwili and Victoria Esquivel- Korsiak. Acknowledgment goes to Lino Owor Ogora, Harriet Aloyo, and Jennifer Gigliotti for their role in the preparation of this report. Special thanks go to Stephen Acidri, Father Alex, Father Elio Zanei, Sister Paola, Veronica Eyotaru and all of the survivors and relatives of victims who took time to speak with JRP. Thanks also to the Royal Norwegian Embassy for their financial support. Designed by Oryem Nyeko. Cover photograph: The mass grave located at the Ombaci Mission. Back photographs: Survivors of the Ombaci massacre pose after the Ombaci Massacre Memorial Prayer, 24 June 2013. -

UNICEF Uganda End-Of-Year Humanitarian Situation Report
Uganda Country Office Humanitarian Situation Report No. 4 UNICEF/UNI325795/Abdul © Reporting Period: April 2020 Situation in Numbers Highlights 2.12 million • As of 30 April, Uganda reported 81 confirmed COVID-19 cases, 52 # of children in need of recoveries, and zero deaths. Of the reported cases, nine were in humanitarian assistance children. The majority of cases were imported by travelers and truck (UNICEF HAC 2020) drivers. The national lockdown, while effective in slowing the spread of the virus, is affecting access to essential social services. • During this reporting period, 40,000 children (20,080 girls, 19,920 3.48 million boys) were reached with home-based distance learning to ensure # of people in need continuity of learning after schools closed to prevent the spread of (UNICEF HAC 2020) the novel coronavirus. • 10,309 children (5,216 girls, 5,093 boys) were treated for severe acute malnutrition (SAM) in refugee-hosting districts and Karamoja 840,007 as of April 2020. # of refugees and asylum- • In April, 745,489 children and women (387,654 female, 357,835 seekers who are children male) continued to receive essential health care services, including immunization, prenatal, postnatal, HIV, and gender-based violence care in UNICEF-supported facilities. 1.42 million • 800,000 risk-communication materials were distributed to 120 # of total refugees and districts through partners in April 2020, strengthening COVID-19 asylum-seekers (OPM, Pro information, education and communication (IEC). Gres V4 30 April 2020) • 428,294 adolescents were reached with information on how to report allegations of sexual exploitation and abuse (SEA). UNICEF HAC Appeal 2020 UNICEF Response and Funding Status US$50.12 million Funding Status (in US$) US$ 0.73 M funds received US$ 12.6 M carried forward US$ 36.75 M funding gap 1 Funding Overview and Partnerships The 2020 UNICEF Humanitarian Action for Children (HAC) appeal for Uganda is seeking US$50.12 million to sustain the provision of life-saving services to vulnerable women and children.