NMDAR Modulators As Rapid Antidepressants: Converging And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RAP-MD-05 GLYX13-C-203 Protocol Amendment 3 Final-R
NCT02192099 Study ID: GLYX13‐C‐203 Title: Open Label Extension for Subjects with Inadequate/Partial Response to Antidepressants during the Current Episode of Major Depressive Disorder Previously Treated with Rapastinel (GLYX‐13) (Extension of GLYX13‐C‐202, NCT01684163) Protocol Amendment 3 Date: 23 Nov 2016 Clinical Study Protocol Protocol Number: GLYX13-C-203 Study Drug: Rapastinel (GLYX-13) Injection (rapastinel Injection) FDA ID: 107,974 Clinicaltrials.gov: Title: Open Label Extension for Subjects with Inadequate/Partial Response to Antidepressants during the Current Episode of Major Depressive Disorder Previously Treated with Rapastinel (GLYX-13) (Extension of GLYX13-C-202, NCT01684163) Study Phase: 2 Sponsor: Naurex, Inc, an affiliate of Allergan, plc. Date: Amendment 3 dated 23 November 2016 Replaces Amendment 2 dated 20 January 2015 This document is a confidential communication from Naurex, Inc, an affiliate of Allergan, plc.. Acceptance of this document constitutes an agreement by the recipient(s) that no information contained herein will be published or disclosed without prior written approval from Allergan, plc., except that this document may be disclosed to appropriate Institutional Review Boards (IRBs) under the condition that they are also required to maintain confidentiality. Naurex, Inc, an affiliate of Allergan, plc. Protocol GLYX13-C-203 INVESTIGATOR SIGNATURE PAGE The signature of the investigator below constitutes his/her approval of this protocol and provides the necessary assurances that this study will be conducted according to all stipulations of the protocol as specified in both the clinical and administrative sections, including all statements regarding confidentiality. This trial will be conducted in compliance with the protocol and all applicable regulatory requirements, in accordance with Good Clinical Practices (GCPs), including International Conference on Harmonization (ICH) Guidelines, and in general conformity with the most recent version of the Declaration of Helsinki. -

Prevention Or Amelioration of Autism-Like Symptoms in Animal Models: Will It Bring Us Closer to Treating Human ASD?
International Journal of Molecular Sciences Review Prevention or Amelioration of Autism-Like Symptoms in Animal Models: Will it Bring Us Closer to Treating Human ASD? Asher Ornoy 1,* , Liza Weinstein-Fudim 1 and Zivanit Ergaz 1,2 1 Laboratory of Teratology, Department of Medical Neurobiology, Hebrew University Hadassah Medical School, Jerusalem 9112001, Israel; [email protected] 2 Neonatology Department, Hadassah Hebrew University Medical Center, Jerusalem 9112001, Israel; [email protected] * Correspondence: [email protected]; Tel.: +972-2-6758329 Received: 17 February 2019; Accepted: 23 February 2019; Published: 1 March 2019 Abstract: Since the first animal model of valproic acid (VPA) induced autistic-like behavior, many genetic and non-genetic experimental animal models for Autism Spectrum Disorder (ASD) have been described. The more common non-genetic animal models induce ASD in rats and mice by infection/inflammation or the prenatal or early postnatal administration of VPA. Through the establishment of these models, attempts have been made to ameliorate or even prevent ASD-like symptoms. Some of the genetic models have been successfully treated by genetic manipulations or the manipulation of neurotransmission. Different antioxidants have been used (i.e., astaxanthin, green tea, piperine) to reduce brain oxidative stress in VPA-induced ASD models. Agents affecting brain neurotransmitters (donepezil, agmatine, agomelatine, memantine, oxytocin) also successfully reduced ASD-like symptoms. However, complete prevention of the development of symptoms was achieved only rarely. In our recent study, we treated mouse offspring exposed on postnatal day four to VPA with S-adenosine methionine (SAM) for three days, and prevented ASD-like behavior, brain oxidative stress, and the changes in gene expression induced by VPA. -

Poster Session III, December 6, 2017
Neuropsychopharmacology (2017) 42, S476–S652 © 2017 American College of Neuropsychopharmacology. All rights reserved 0893-133X/17 www.neuropsychopharmacology.org Poster Session III a high-resolution research tomograph (HRRT), and struc- Palm Springs, California, December 3–7, 2017 tural (T1) MRI using a 3-Tesla scanner. PET data analyses were carried out using the validated 2-tissue compartment Sponsorship Statement: Publication of this supplement is model to determine the total volume of distribution (VT) of sponsored by the ACNP. [18F]FEPPA. Individual contributor disclosures may be found within the Results: Results show significant inverse associations (con- abstracts. Part 1: All Financial Involvement with a pharma- trolling for rs6971 genotype) between neuroinflammation ceutical or biotechnology company, a company providing (VTs) and cortical thickness in the right medial prefrontal clinical assessment, scientific, or medical products or compa- cortex [r = -.562, p = .029] and the left dorsolateral nies doing business with or proposing to do business with prefrontal cortex [r = -.629, p = .012](p values are not ACNP over past 2 years (Calendar Years 2014–Present); Part 2: corrected for multiple comparisons). No significant associa- Income Sources & Equity of $10,000 per year or greater tions were found with surface area. (Calendar Years 2014 - Present): List those financial relation- Conclusions: These results, while preliminary, suggest links ships which are listed in part one and have a value greater than between the microglial activation/neuroinflammation and $10,000 per year, OR financial holdings that are listed in part cortical thickness in the dorsolateral prefrontal cortex and one and have a value of $10,000 or greater as of the date of medial prefrontal cortex in AD patients. -
NMDA Receptors Containing the Glun2d Subunit Control Neuronal Function in the Subthalamic Nucleus
The Journal of Neuroscience, December 2, 2015 • 35(48):15971–15983 • 15971 Cellular/Molecular NMDA Receptors Containing the GluN2D Subunit Control Neuronal Function in the Subthalamic Nucleus X Sharon A. Swanger,1* Katie M. Vance,1* Jean-Franc¸ois Pare,3 Florence Sotty,4 Karina Fog,4 Yoland Smith,2,3 and X Stephen F. Traynelis1 1Department of Pharmacology and 2Department of Neurology, Emory University School of Medicine, Atlanta, Georgia 30322, 3Yerkes National Primate Research Center and Morris K. Udall Center of Excellence for Parkinson’s Disease Research, Emory University, Atlanta, Georgia 30329, and 4H. Lundbeck A/S, Division of Neurodegeneration and Biologics, Ottiliavej 9, DK-2500 Valby, Denmark The GluN2D subunit of the NMDA receptor is prominently expressed in the basal ganglia and associated brainstem nuclei, including the subthalamic nucleus (STN), globus pallidus, striatum, and substantia nigra. However, little is known about how GluN2D-containing NMDA receptors contribute to synaptic activity in these regions. Using Western blotting of STN tissue punches, we demonstrated that GluN2D is expressed in the rat STN throughout development [age postnatal day 7 (P7)–P60] and in the adult (age P120). Immunoelectron microscopy of the adult rat brain showed that GluN2D is predominantly expressed in dendrites, unmyelinated axons, and axon terminals within the STN. Using subunit-selective allosteric modulators of NMDA receptors (TCN-201, ifenprodil, CIQ, and DQP-1105), we provide evidence that receptors containing the GluN2B and GluN2D subunits mediate responses to exogenously applied NMDA and glycine, as well as synaptic NMDA receptor activation in the STN of rat brain slices. EPSCs in the STN were mediated primarily by AMPA and NMDA receptors and GluN2D-containing NMDA receptors controlled the slow deactivation time course of EPSCs in the STN. -
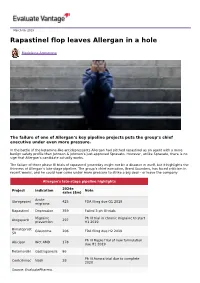
Rapastinel Flop Leaves Allergan in a Hole
March 06, 2019 Rapastinel flop leaves Allergan in a hole Madeleine Armstrong The failure of one of Allergan’s key pipeline projects puts the group’s chief executive under even more pressure. In the battle of the ketamine-like antidepressants Allergan had pitched rapastinel as an agent with a more benign safety profile than Johnson & Johnson’s just-approved Spravato. However, unlike Spravato, there is no sign that Allergan’s candidate actually works. The failure of three phase III trials of rapastinel yesterday might not be a disaster in itself, but it highlights the thinness of Allergan’s late-stage pipeline. The group’s chief executive, Brent Saunders, has faced criticism in recent weeks, and he could now come under more pressure to strike a big deal – or leave the company. Allergan's late-stage pipeline highlights 2024e Project Indication Note sales ($m) Acute Ubrogepant 425 FDA filing due Q1 2019 migraine Rapastinel Depression 359 Failed 3 ph III trials Migraine Ph III trial in chronic migraine to start Atogepant 297 prevention H1 2019 Bimatoprost Glaucoma 206 FDA filing due H2 2019 SR Ph III Maple trial of new formulation Abicipar Wet AMD 178 due H1 2019 Relamorelin Gastroparesis 86 Ph III Aurora trial due to complete Cenicriviroc Nash 28 2020 Source: EvaluatePharma. Activist shareholders have long been agitating for change at Allergan, and the latest failure will only provide more ammunition to those who want to split the roles of chairman and chief exec amid dissatisfaction with the group's acquisition strategy, and with its stock hovering around a five-year low. -

WO 2017/066590 Al 20 April 2017 (20.04.2017) P O P CT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2017/066590 Al 20 April 2017 (20.04.2017) P O P CT (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 38/06 (2006.01) A61K 31/519 (2006.01) kind of national protection available): AE, AG, AL, AM, A61 38/07 (2006.0V) A61K 31/551 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/13 (2006.01) A61K 31/5513 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, A61K 31/135 (2006.01) A61P 25/24 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, A61K 31/496 (2006.01) A61P 25/18 (2006.01) HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (21) International Application Number: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, PCT/US20 16/057071 OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (22) International Filing Date: SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, 14 October 2016 (14.10.201 6) TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, zw. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of regional protection available): ARIPO (BW, GH, (30) Priority Data: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, 62/242,633 16 October 2015 (16. -

Gottlieb's Shock Resignation Leaves Ripples in the Industry
15 March 2019 No. 3946 Scripscrip.pharmaintelligence.informa.com Pharma intelligence | informa time, which is difficult. He also used the office in a “forward-leaning way” not seen often. “He kind of drove the conversation through very good communication exter- nally,” Myers said. “He was able to use a lot of the ideas percolating in the agency, pack- age them and get them moved forward.” Gottlieb pushed FDA to the forefront of the drug pricing debate, a position the agency had not sought in the past. In his first speech to staff after confir- mation, he said that even though the agency cannot set drug prices, it can promote competition. Gottlieb was vocal in chastising the brand industry for blocking generic Credit: FDA Credit: competition, warning that Congress could make more drastic changes if it did not stop employing pay-for-delay and licensing tactics intended to pre- Gottlieb’s Shock Resignation vent patent challenges. (Also see “Got- tlieb: Real Risk Of Congressional Action If Leaves Ripples In The Industry Anti-Competitive Actions Continue” - Pink Sheet, 3 May, 2018.) DERRICK GINGERY [email protected] He also publicly released a list of com- panies thought to be using the Risk Evalu- S FDA Commissioner Scott Gott- being apart from my family for these past ation and Mitigation Strategy system to lieb, one of the most popular and two years and missing my wife and three prevent generic companies from purchas- Uvisible commissioners in decades, young children.” ing samples for testing, although it is not will end his tenure as head of FDA in about clear the move had much impact. -

GLYX-13 Produces Rapid Antidepressant Responses with Key Synaptic and Behavioral Effects Distinct from Ketamine
Neuropsychopharmacology (2017) 42, 1231–1242 © 2017 American College of Neuropsychopharmacology. All rights reserved 0893-133X/17 www.neuropsychopharmacology.org GLYX-13 Produces Rapid Antidepressant Responses with Key Synaptic and Behavioral Effects Distinct from Ketamine 1,5 1,5 1,2 1 1 1 Rong-Jian Liu , Catharine Duman , Taro Kato , Brendan Hare , Dora Lopresto , Eunyoung Bang , 3 3,4 1 1 *,1 Jeffery Burgdorf , Joseph Moskal , Jane Taylor , George Aghajanian and Ronald S Duman 1Departments of Psychiatry and Neurosciences, Yale University School of Medicine, New Haven, CT, USA; 2Sumitomo Dainippon Pharma Co, Suita, 3 Osaka, Japan; Falk Center for Molecular Therapeutics, Department of Biomedical Engineering, Northwestern University, Evanston IL, USA; 4 Naurex, Inc., Evanston, IL, USA GLYX-13 is a putative NMDA receptor modulator with glycine-site partial agonist properties that produces rapid antidepressant effects, but without the psychotomimetic side effects of ketamine. Studies were conducted to examine the molecular, cellular, and behavioral actions of GLYX-13 to further characterize the mechanisms underlying the antidepressant actions of this agent. The results demonstrate that a single dose of GLYX-13 rapidly activates the mTORC1 pathway in the prefrontal cortex (PFC), and that infusion of the selective mTORC1 inhibitor rapamycin into the medial PFC (mPFC) blocks the antidepressant behavioral actions of GLYX-13, indicating a requirement for mTORC1 similar to ketamine. The results also demonstrate that GLYX-13 rapidly increases the number and function of spine synapses in the apical dendritic tuft of layer V pyramidal neurons in the mPFC. Notably, GLYX-13 significantly increased the synaptic responses to hypocretin, a measure of thalamocortical synapses, compared with its effects on 5-HT responses, a measure of cortical- cortical responses mediated by the 5-HT receptor. -

Sustained Antidepressant Action of the N‑Methyl‑D‑Aspartate Receptor Antagonist MK‑801 in a Chronic Unpredictable Mild Stress Model
5376 EXPERIMENTAL AND THERAPEUTIC MEDICINE 16: 5376-5383, 2018 Sustained antidepressant action of the N‑methyl‑D‑aspartate receptor antagonist MK‑801 in a chronic unpredictable mild stress model BANG-KUN YANG1, JUN QIN2, YING NIE3 and JIN-CAO CHEN1 1Department of Neurosurgery, Zhongnan Hospital of Wuhan University, Wuhan, Hubei 430071; Departments of 2Neurosurgery and 3Children's Medical Center, Taihe Hospital, Hubei University of Medicine, Shiyan, Hubei 442600, P.R. China Received December 29, 2016; Accepted November 29, 2017 DOI: 10.3892/etm.2018.6876 Abstract. (5S,10R)-5-methyl-10,11-dihydro-5H-dibenzo(A,D) mice. Therefore, the present study revealed the sustained cyclohepten-5,10-imine hydrogen maleate (MK-801) is antidepressant effects of MK-801 in the CUMS model. an N-methyl-D-aspartate non-competitive antagonist that Furthermore, synaptogenesis and neuronal regeneration in the possesses useful biological properties, including anticon- prelimbic regions of mPFC, DG and CA3 of the hippocampus vulsant and anesthetic activities. Studies have indicated the may be implicated as mechanisms that promote a sustained rapid antidepressant effects of MK-801 in animal models. antidepressant response. However, there are no reports concerning a sustained anti- depressant effect in the chronic unpredictable mild stress Introduction (CUMS) model. Furthermore, the antidepressant mechanism remains unclear. The aim of the present study was to examine In addition to being the most prevalent mental disorder, the effects of MK-801 (0.1 mg/kg) and rapastinel (10 mg/kg) depression is one of the leading causes of disability across on depression-like behavior in CUMS mice and measure the world (1). -

A Systematic Review of Performance-Enhancing Pharmacologicals and Biotechnologies in the Army
Bond University Research Repository A systematic review of performance-enhancing pharmacologicals and biotechnologies in the Army Ko, Henry ; Hunter, K E; Scott, A M; Ayson, Mark; Willson, M L Published in: Journal of the Royal Army Medical Corps DOI: 10.1136/jramc-2016-000752 Licence: CC BY-NC Link to output in Bond University research repository. Recommended citation(APA): Ko, H., Hunter, K. E., Scott, A. M., Ayson, M., & Willson, M. L. (2018). A systematic review of performance- enhancing pharmacologicals and biotechnologies in the Army. Journal of the Royal Army Medical Corps, 164(3). https://doi.org/10.1136/jramc-2016-000752 General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. For more information, or if you believe that this document breaches copyright, please contact the Bond University research repository coordinator. Download date: 06 Oct 2021 ABSTRACT Introduction: In 2015, the Australian Army commissioned a systematic review to assess the evidence on effectiveness and safety of pharmacological and biotechnological products for cognitive enhancement specifically in Army personnel. Methods: Searches for studies examining biotechnological and pharmacological products in Army populations were conducted in December 2015. Cochrane CENTRAL, MEDLINE, EMBASE, CINAHL and PsycINFO were searched; no date or language restrictions were applied. WHO’s International Clinical Trials Registry Platform and ClinicalTrials.gov were searched to identify ongoing trials. Studies meeting inclusion criteria were evaluated for risk of bias using the Cochrane Risk of Bias tool. -

Exploring Hallucinogen Pharmacology and Psychedelic Medicine with Zebrafish Models
ZEBRAFISH Volume 13, Number 5, 2016 Review Articles ª Mary Ann Liebert, Inc. DOI: 10.1089/zeb.2016.1251 Exploring Hallucinogen Pharmacology and Psychedelic Medicine with Zebrafish Models Evan J. Kyzar1 and Allan V. Kalueff2–6 Abstract After decades of sociopolitical obstacles, the field of psychiatry is experiencing a revived interest in the use of hallucinogenic agents to treat brain disorders. Along with the use of ketamine for depression, recent pilot studies have highlighted the efficacy of classic serotonergic hallucinogens, such as lysergic acid diethylamide and psilocybin, in treating addiction, post-traumatic stress disorder, and anxiety. However, many basic phar- macological and toxicological questions remain unanswered with regard to these compounds. In this study, we discuss psychedelic medicine as well as the behavioral and toxicological effects of hallucinogenic drugs in zebrafish. We emphasize this aquatic organism as a model ideally suited to assess both the potential toxic and therapeutic effects of major known classes of hallucinogenic compounds. In addition, novel drugs with hal- lucinogenic properties can be efficiently screened using zebrafish models. Well-designed preclinical studies utilizing zebrafish can contribute to the reemerging treatment paradigm of psychedelic medicine, leading to new avenues of clinical exploration for psychiatric disorders. Introduction requiring the use of both traditional (rodent) and novel model species.6 In this study, we briefly review the history of psy- allucinogenic drugs have been used by humans for chedelic medicine and the pharmacology of these drugs and centuries, exerting potent effects on thought, cognition, H discuss the effects of hallucinogenic drugs on larval and adult and behavior with little propensity for habit formation and zebrafish (Danio rerio). -

Ketamine and Beyond: Investigations Into the Potential of Glutamatergic Agents to Treat Depression
Drugs DOI 10.1007/s40265-017-0702-8 REVIEW ARTICLE Ketamine and Beyond: Investigations into the Potential of Glutamatergic Agents to Treat Depression 1 1 1 Marc S. Lener • Bashkim Kadriu • Carlos A. Zarate Jr Ó Springer International Publishing Switzerland (outside the USA) 2017 Abstract Clinical and preclinical studies suggest that dysfunction of the glutamatergic system is implicated in Key Points mood disorders such as major depressive disorder and bipolar depression. In clinical studies of individuals with This review highlights evidence supporting the major depressive disorder and bipolar depression, rapid antidepressant effects of subanesthetic-dose reductions in depressive symptoms have been observed in ketamine as a prototypical glutamatergic-modulating response to subanesthetic-dose ketamine, an agent whose agent from which other glutamatergic agents have mechanism of action involves the modulation of gluta- been investigated. matergic signaling. The findings from these studies have prompted the repurposing and/or development of other Evidence suggests that ketamine may have broad glutamatergic modulators for antidepressant efficacy, both biological effects on the glutamatergic system and as monotherapy or as an adjunct to conventional may exert its clinical efficacy by altering other monoaminergic antidepressants. This review highlights symptom domains related to depression, such as the evidence supporting the antidepressant effects of anxiety and suicidality. subanesthetic-dose ketamine as well as other glutamatergic This review also highlights important safety modulators, such as D-cycloserine, riluzole, CP-101,606, concerns regarding ketamine and selected CERC-301 (previously known as MK-0657), basimglurant, glutamatergic agents to promote the continued JNJ-40411813, dextromethorphan, nitrous oxide, GLYX- development of novel, effective, and safe 13, and esketamine.