Small-Bowel Capsule Endoscopy and Device-Assisted Enteroscopy For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Provocative Testing and Localization in Video Capsule Endoscopy
1 2 The Role of Provocative 3 4 Testing and Localization of 5 6 the Video Capsule Endoscope in 7 the Management of Small 8 9 Intestinal Bleeding Q4 10 11 a, b 12 Daniel L. Raines, MD *, Douglas G. Adler, MD Q5 Q6 Q7 13 Q1 Q2 14 15 KEYWORDS 16 Small intestinal bleeding Provocative angiography Provocative endoscopy 17 Video capsule endoscopy Device-assisted enteroscopy 18 19 20 KEY POINTS 21 Cases of small intestinal bleeding (SIB) are commonly encountered in clinical practice 22 despite advancements in medical technology that allow consistent visualization of the 23 entire gastrointestinal tract. 24 The use of antithrombotic agents to provoke bleeding has been found to be revealing in 25 cases of SIB when used in combination with angiography as well as endoscopy. 26 The performance of endoscopic procedures, including video capsule endoscopy (VCE) 27 and device-assisted enteroscopy (DAE) on active antiplatelet and/or anticoagulant ther- 28 apy is considered low risk and may improve diagnostic yield. 29 The use of VCE for gastrointestinal bleeding in the inpatient setting has been found to 30 improve diagnostic yield and decrease hospital stay. 31 Because DAE is required for therapeutic intervention in patients with small bowel 32 bleeding, access to this technology is essential for effective management in many cases. 33 34 35 Video content accompanies this article at http://www.giendo.theclinics.com/. 36 37 Q8 38 OBSCURE GASTROINTESTINAL BLEEDING Definitions 39 40 Small intestinal bleeding (SIB) has been described as bleeding that is undefined in 41 cause despite evaluation by standard upper endoscopy, colonoscopy, and small Q9 42 bowel follow-through (SBFT). -

ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding
nature publishing group PRACTICE GUIDELINES 1265 CME ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding L a u r e n B . G e r s o n , M D , M S c , F A C G1 , J e ff L. Fidler , MD 2 , D a v i d R . C a v e , M D , P h D , F A C G 3 a n d J o n a t h a n A . L e i g h t o n , M D , F A C G 4 Bleeding from the small intestine remains a relatively uncommon event, accounting for ~5–10% of all patients presenting with gastrointestinal (GI) bleeding. Given advances in small bowel imaging with video capsule endoscopy (VCE), deep enteroscopy, and radiographic imaging, the cause of bleeding in the small bowel can now be identifi ed in most patients. The term small bowel bleeding is therefore proposed as a replacement for the previous classifi cation of obscure GI bleeding (OGIB). We recommend that the term OGIB should be reserved for patients in whom a source of bleeding cannot be identifi ed anywhere in the GI tract. A source of small bowel bleeding should be considered in patients with GI bleeding after performance of a normal upper and lower endoscopic examination. Second-look examinations using upper endoscopy, push enteroscopy, and/or colonoscopy can be performed if indicated before small bowel evaluation. VCE should be considered a fi rst-line procedure for small bowel investigation. Any method of deep enteroscopy can be used when endoscopic evaluation and therapy are required. -

Obscure Gastrointestinal Bleeding in Cirrhosis: Work-Up and Management
Current Hepatology Reports (2019) 18:81–86 https://doi.org/10.1007/s11901-019-00452-6 MANAGEMENT OF CIRRHOTIC PATIENT (A CARDENAS AND P TANDON, SECTION EDITORS) Obscure Gastrointestinal Bleeding in Cirrhosis: Work-up and Management Sergio Zepeda-Gómez1 & Brendan Halloran1 Published online: 12 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Obscure gastrointestinal bleeding (OGIB) in patients with cirrhosis can be a diagnostic and therapeutic challenge. Recent advances in the approach and management of this group of patients can help to identify the source of bleeding. While the work-up of patients with cirrhosis and OGIB is the same as with patients without cirrhosis, clinicians must be aware that there are conditions exclusive for patients with portal hypertension that can potentially cause OGIB. Recent Findings New endoscopic and imaging techniques are capable to identify sources of OGIB. Balloon-assisted enteroscopy (BAE) allows direct examination of the small-bowel mucosa and deliver specific endoscopic therapy. Conditions such as ectopic varices and portal hypertensive enteropathy are better characterized with the improvement in visualization by these techniques. New algorithms in the approach and management of these patients have been proposed. Summary There are new strategies for the approach and management of patients with cirrhosis and OGIB due to new develop- ments in endoscopic techniques for direct visualization of the small bowel along with the capability of endoscopic treatment for different types of lesions. Patients with cirrhosis may present with OGIB secondary to conditions associated with portal hypertension. Keywords Obscure gastrointestinal bleeding . Cirrhosis . Portal hypertension . -

Endoscopic Technique for Diag- Nostic Investigations and Therapeutic Interventions of Small Bowel Pathology
ENDOSCOPY: OPENING NEW EYES, SERIES #3 Andrew K. Roorda, M.D., Series Editor The Evolution of Enteroscopy to Spiral Enteroscopy Disaya Chavalitdhamrong Rome Jutabha The diagnosis and treatment of small bowel diseases has historically proven difficult and challenging for gastroenterologists. Although sonde and push enteroscopy were developed first, the former is time-consuming and uncomfortable and the latter limits examination to the proximal jejunum. Intraoperative enteroscopy, which was once con- sidered the gold standard of enteroscopy, has largely been replaced by newer less inva- sive techniques. Capsule endoscopy provides a thorough examination of the small bowel but it does not allow for therapeutic interventions. Balloon-assisted enteroscopy was developed for complete examination of the small bowel and therapeutic interven- tions. Spiral enteroscopy has emerged as a viable alternative to balloon-assisted enteroscopy. It is a safe, effective, and relatively rapid endoscopic technique for diag- nostic investigations and therapeutic interventions of small bowel pathology. This arti- cle reviews the milestone technologies of enteroscopy highlighting the latest developed spiral enteroscopy. INTRODUCTION form endoscopic treatments. With the development of ndoscopic diagnosis and treatment of small bowel balloon-assisted enteroscopy and most recently, spiral conditions is a challenging area for gastroenterol- enteroscopy, endoscopic diagnosis and treatment of Eogists. Until recently, it was not possible to access the entire small intestine are now feasible without most of the small bowel using endoscopic techniques operative intervention. As indications expand and without concomitant surgery. Capsule endoscopy and caseloads grow, it is important for gastroenterologists balloon-assisted enteroscopy thus represent decisive to know how these procedures are done and to be breakthroughs in this field. -

Efficacy of Colonoscopy, Colon Capsule and Fecal Immunological Test For
Efficacy of colonoscopy, colon capsule and fecal immunological test for colorectal cancer screening, in first degree relatives of patients with colorectal neoplasia: a prospective randomized study - FAMCAP Study Version n°6 - Date: 2017-07-11 Sponsor: Hospices Civils de Lyon BP 2251 3 quai des Célestins 69229 LYON Cedex 02 - France Coordinator: Pr Jean-Christophe SAURIN Hepatogastroenterology - Pav. L Edouard Herriot Hospital - Hospices Civils de Lyon 5 Place d’Arsonval 69437 LYON Cedex 3 - FRANCE Phone: +33 (0)4 72 11 75 72; Fax: +33 (0)4 72 11 01 47 E-mail: [email protected] Methodologist: Pr Anne-Marie SCHOTT Pôle IMER - Hospices Civils de Lyon 162 avenue Lacassagne 69424 LYON Cedex 3 - FRANCE E-mail: [email protected] Sponsor code: 69HCL16_0091 ID-RCB number: 2016-A01097-44 Clinicaltrials.gov registration number: NCT02738359 Date of Ethics Committee (CPP Sud-Est III) approval: 2016-10-18 Abstract: Fecal immunological test (FIT) is the reference screening method in average risk patient. FIT is proposed every 2 years to all asymptomatic subjects with average risk aged from 50 to 74 years in France. Optical colonoscopy (OC) is the gold standard examination for patients at increased risk of colorectal cancer, like those with a first degree relative with colorectal cancer (relative risk between 2 and 4 times that of the general population). Colonoscopy should be performed in this high risk group before 50 years or 5 to 10 years before the earliest case of colorectal cancer. Optical colonoscopy has important limitations: complications (perforation, bleeding), need to use general anesthesia (in France 95% of colonoscopy are performed under general anesthesia), and low acceptability for screening even in high risk persons (40% in the best cases). -
Capsule Endoscopy
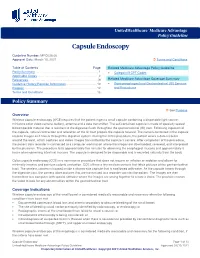
UnitedHealthcare® Medicare Advantage Policy Guideline Capsule Endoscopy Guideline Number: MPG036.06 Approval Date: March 10, 2021 Terms and Conditions Table of Contents Page Related Medicare Advantage Policy Guideline Policy Summary ............................................................................. 1 • Category III CPT Codes Applicable Codes .......................................................................... 3 References ..................................................................................... 9 Related Medicare Advantage Coverage Summary Guideline History/Revision Information ..................................... 10 • Gastroesophageal and Gastrointestinal (GI) Services Purpose ........................................................................................ 12 and Procedures Terms and Conditions ................................................................. 13 Policy Summary See Purpose Overview Wireless capsule endoscopy (WCE) requires that the patient ingest a small capsule containing a disposable light source, miniature color video camera, battery, antenna and a data transmitter. The self-contained capsule is made of specially sealed biocompatible material that is resistant to the digestive fluids throughout the gastrointestinal (GI) tract. Following ingestion of the capsule, natural contraction and relaxation of the GI tract propels the capsule forward. The camera contained in the capsule records images as it travels through the digestive system. During the entire procedure, the patient wears -

Clinical Impact of Small Bowel Capsule Endoscopy in Obscure Gastrointestinal Bleeding
medicina Article Clinical Impact of Small Bowel Capsule Endoscopy in Obscure Gastrointestinal Bleeding Ana-Maria Singeap 1,2 , Camelia Cojocariu 1,2,*, Irina Girleanu 1,2, Laura Huiban 1,2, Catalin Sfarti 1,2, Tudor Cuciureanu 1,2, Stefan Chiriac 1,2 , Carol Stanciu 2 and Anca Trifan 1,2 1 Department of Gastroenterology, Faculty of Medicine, “Grigore T. Popa” University of Medicine and Pharmacy, 700115 Iasi, Romania; [email protected] (A.-M.S.); [email protected] (I.G.); [email protected] (L.H.); [email protected] (C.S.); [email protected] (T.C.); [email protected] (S.C.); [email protected] (A.T.) 2 Institute of Gastroenterology and Hepatology, “St. Spiridon” Emergency Hospital, 700111 Iasi, Romania; [email protected] * Correspondence: [email protected]; Tel.: +40-752223968 Received: 31 August 2020; Accepted: 16 October 2020; Published: 19 October 2020 Abstract: Background and objectives: The most frequent indications for small bowel capsule endoscopy (SBCE) are obscure gastrointestinal bleeding (OGIB) and iron deficiency anemia (IDA). The aim of this study was to evaluate the diagnostic yield (DY) of SBCE in overt and occult OGIB, as well as its impact on the clinical outcome. Materials and Methods: This study retrospectively included all cases of OGIB investigated by SBCE in a tertiary care referral center, between 1st January 2016 and 31st December 2018. OGIB was defined by overt or occult gastrointestinal bleeding, with negative upper and lower endoscopy. Occult gastrointestinal bleeding was either proved by a fecal test or presumptively incriminated as a cause for IDA. DY was defined as the detection rate for what were thought to be clinically significant findings. -

Capsule Endoscopy
CLINICAL MEDICAL POLICY Policy Name: Capsule Endoscopy Policy Number: MP-038-MD-PA Responsible Department(s): Medical Management Provider Notice Date: 02/17/2020 Issue Date: 02/17/2020 Effective Date: 03/16/2020 Annual Approval Date: 12/2020 Revision Date: 12/18/2019 Products: Gateway Health℠ Medicaid Application: All participating hospitals and providers Page Number(s): 1 of 12 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ provides coverage under the medical-surgical benefits of the Company’s Medicaid products for medically necessary capsule endoscopy procedures. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. (Current applicable Pennsylvania HealthChoices Agreement Section V. Program Requirements, B. Prior Authorization of Services, 1. General Prior Authorization Requirements.) Policy No. MP-038-MD-PA Page 1 of 12 DEFINITIONS Prior Authorization Review Panel (PARP) – A panel of representatives from within the Pennsylvania Department of Human Services who have been assigned organizational responsibility for the review, approval and denial of all PH-MCO Prior Authorization policies and procedures. Gastric Emptying Scintigraphy – A diagnostic test where the individual ingests a radionuclide-labeled standard meal, and then images are taken at 0, 1, 2, and 4 hours postprandial in order to measure how much of the meal has passed beyond the stomach. -

The Future of Small Bowel Transplantation
Archives ofDisease in Childhood 1995; 72: 447-451 447 CURRENT TOPIC Arch Dis Child: first published as 10.1136/adc.72.5.447 on 1 May 1995. Downloaded from The future of small bowel transplantation Deirdre A Kelly, John A C Buckels Although transplantation of solid organs such Indications for small bowel as kidney and liver have been established since transplantation the 1970s and 1980s, the future of small bowel Small bowel transplantation should be con- transplantation as treatment for intestinal fail- sidered for all children with irreversible ure is only just evolving. Early clinical experi- intestinal failure who are dependent on par- ence was almost universally unsuccessful but enteral nutrition for survival and in whom all recent developments in surgical technique, attempts to improve intestinal adaptation have immunosuppression, and postoperative man- been unsuccessful. Potential candidates may agement have improved outcome with a 50% require small bowel transplantation alone or survival in at least 100 operations.' combined with a liver transplant. Small intestinal transplantation was first The current indications for isolated small demonstrated to be technically feasible in bowel transplantation include: (1) loss of animals in 1902,24 and in humans in the vascular access with normal liver function and 1980s,5-7 but it was not until the Pittsburg histology and (2) intractable gastrointestinal group initiated a programme of small bowel fluid loss. The current indications for com- transplantation using the novel immuno- bined small -

Capsule Endoscopy Lets Your Doctor Examine the Lining of the Middle
by colonoscopy. The most common reason for abdomen with adhesive sleeves (similar to What is capsule endoscopy? doing capsule endoscopy is to search for a tape).These are attached to a data recorder cause of bleeding from the small intestine. It worn on a strap over your shoulder. The pill-sized Capsule Endoscopy lets your doctor examine may also be useful for detecting polyps, capsule endoscope is swallowed and passes the lining of the middle part of your inflammatory bowel disease (Crohn’s disease), naturally through your digestive tract while gastrointestinal tract, which includes the three ulcers, and tumours of the small intestine. transmitting video images to the data recorder. portions of the small intestine (duodenum, jejunum, and ileum). Your doctor will give you a You will be able to drink clear liquids after two pill sized video camera for you to swallow. This How Should I Prepare for the Procedure? hours and eat a light meal after four hours camera has its own light source and takes It is important that the small bowel is empty of following the capsule ingestion, unless your pictures of your small intestine as it passes food for the test. Your last solid food should be doctor instructs you otherwise. You will have to through. These pictures are transmitted by a taken at lunchtime the day before your avoid vigorous physical activity such as running weak radio signal to a small recording device appointment. You may continue to take clear or jumping during the study you have to wear on your body. fluids up to 12 hours before the test. -

Endoscopic Techniques in Bariatric Patients: Obesity Basics and Normal Postbariatric Surgery Anatomy Dan E
Techniques in Gastrointestinal Endoscopy (2010) 12, 124-129 Techniques in GASTROINTESTINAL ENDOSCOPY www.techgiendoscopy.com Endoscopic techniques in bariatric patients: Obesity basics and normal postbariatric surgery anatomy Dan E. Azagury, MD, David B. Lautz, MD Brigham and Women’s Hospital and Harvard Medical School, Department of Surgery, Boston, Massachusetts. KEYWORDS With the sharp rise in the number of bariatric surgical procedures over the past 15 y, the number and Gastric bypass; array of complications have also risen. Many of these complications are now either diagnosed or Vertical banded managed endoscopically. However, the rising diversity of surgical options requires endoscopists to gastroplasty; have a good working knowledge of normal postoperative anatomy for each procedure. This article Laparoscopic gastric reviews basic obesity epidemiology and describes postsurgical anatomy of the upper gastrointestinal banding; tract, separating the procedures into those with normal small bowel anatomy (restrictive procedures) Biliopancreatic diversion; and procedures resulting in small bowel modifications (procedures with a “malabsorptive” component). Laparoscopic sleeve © 2010 Elsevier Inc. All rights reserved. gastrectomy Many classifications have been used to measure and million potential candidates qualifying for a bariatric surgi- define obesity, of which body mass index (BMI) is the most cal procedure. The often dramatic results of this surgery widely used. BMI is calculated by dividing weight in kilo- have lead to a sharp rise in the interest and number of grams by the square of height in meters. Normal weight bariatric surgical procedures performed over the past 15 y. ranges from 18.5 to 24.9 kg/m2. A BMI between 25 and The number of bariatric procedures performed in the United 29.9 kg/m2 is defined as overweight and an individual is States and Canada was 14,000 in 1998,6 compared with an obese when his or her BMI is Ն30 kg/m2. -

Overview of Deep Small Bowel Enteroscopy 10/7/14, 4:23 PM
Overview of deep small bowel enteroscopy 10/7/14, 4:23 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Overview of deep small bowel enteroscopy Author Section Editor Deputy Editor Hiroto Kita, MD, PhD Douglas A Howell, MD, FASGE, FACG Anne C Travis, MD, MSc, FACG, AGAF All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Sep 2014. | This topic last updated: Oct 23, 2013. INTRODUCTION — Evaluation of the small bowel is difficult due to its length, intraperitoneal location, and contractility. Methods used to evaluate the small bowel include push enteroscopy, video capsule endoscopy, and intraoperative enteroscopy. These techniques all have advantages and limitations: ● Push enteroscopy has both diagnostic and therapeutic capabilities, but typically only examines that part of the small bowel that is 50 to 150 cm distal to the ligament of Treitz ● Video capsule endoscopy is capable of examining the entire small bowel, but lacks therapeutic capacity ● Intraoperative enteroscopy permits examination of the entire small bowel and therapeutic interventions, but is much more invasive Alternative endoscopic approaches have been developed to overcome these limitations. Deep small bowel enteroscopy permits visualization and interventional therapy throughout the small bowel by using insertion techniques that pleat the small bowel onto an overtube. The techniques used for deep small bowel enteroscopy limit stretching of the small bowel (as occurs with