Multiple Births
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Background on Multiple Births
National Maternity and Perinatal Audit NHS Maternity Care for Women with Multiple Births and Their Babies A study on feasibility of assessing care using data from births between 1 April 2015 and 31 March 2017 in England, Wales and Scotland The National Maternity and Perinatal Audit (NMPA) is led by the Royal College of Obstetricians and Gynaecologists (RCOG) in partnership with the Royal College of Midwives (RCM), the Royal College of Paediatrics and Child Health (RCPCH) and the London School of Hygiene and Tropical Medicine (LSHTM). The NMPA is commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of the National Clinical Audit and Patient Outcomes Programme (NCAPOP) on behalf of NHS England, the Welsh Government and the Health Department of the Scottish Government. HQIP is led by a consortium of the Academy of Medical Royal Colleges, the Royal College of Nursing, and National Voices. Its aim is to promote quality improvement in patient outcomes, and in particular, to increase the impact that clinical audit, outcome review programmes and registries have on healthcare quality. HQIP holds the contract to commission, manage and develop the NCAPOP, comprising around 40 projects covering care provided to people with a wide range of medical, surgical and mental health conditions. The programme is funded by NHS England, the Welsh Government and, with some individual projects, other devolved administrations and crown dependencies (www.hqip.org.uk/national-programmes). © 2020 Healthcare Quality Improvement Partnership (HQIP) -

Print) • Page 2 of 5
Page 1 of 5 Are twins always high risk? • aims.org.uk Are twins always high risk? AIMS Journal, 2011, Vol 23 No 4 Joanne Whistler asks whether they are really a variation on normal After a wonderful home birth with my firstborn, Oliver, in 2006 I felt confident in my body's ability to labour and give birth. Even when I discovered that I was pregnant with twins late last year I had the attitude that it was just a variation on normal. It was only when I started reading up about multiple pregnancy and birth that my belief that I would have another good experience began to falter. Everything I read said that multiple pregnancies were higher risk, that I should expect a more medicalised experience of pregnancy and birth than a mother of a singleton, and implied that for my babies' sake I should give up any thought of what I considered to be a normal birth. Of course I wanted my babies to be safe, but I also wanted their entry into the world to be gentle and unmedicated – I was very aware of the risks and side effects of pharmacological pain relief and interventions such as induction. In the end I had a fabulous home water birth attended by two independent midwives. My husband and a trusted friend were also there. My midwife monitored the babies intermittently and removed the caul from twin two's face but otherwise my labour and birth were completely intervention-free. In this article I will discuss the evidence base for management of multiple pregnancies and explore some aspects of planning the birth of twins or more. -

Multiple Perspective Discussion Paper
Multiple perspectives: What support do multiple birth families need to live happy and healthy lives? This discussion paper is a compilation of case studies and opinions collected from Twins Research Australia’s collaborators. It provides a wide-ranging overview of issues and challenges for families and health professionals during pregnancy, birth and the early life of twins and multiples. Its aim is to initiate further discussions and explorations, and it provides recommendations for research, education, policy and practice. Acknowledgements This paper is a collaboration of Twins Research Australia, the Twins and Multiple Births Association (TAMBA – UK), the Australian Multiple Birth Association (AMBA) and the International Council of Multiple Birth Organisations (ICOMBO). Authors We wish to thank the following authors of papers included in this publication: Ashlee Tenberge - Australian Multiple Birth Association Christie Bolch - Murdoch Children’s Research Institute, Melbourne Helen Turier - Twins and Multiple Births Association (UK) Janet Young - City of Kingston Council, Victoria Jeff Craig - Deakin University, Victoria Joanna Fitzsimons - Twins and Multiple Births Association (UK) Keith Reed - Twins and Multiple Births Association (UK) Kelly McDonald - Twins and Multiple Births Association (UK) Marie Claire Stear - Twins and Multiple Births Association (UK) Mark Umstad - Melbourne Royal Women’s Hospital Monica Rankin - International Council of Multiple Birth Organisations Natasha Fenwick - Twins and Multiple Births Association (UK) Nikki Roberts - Twins and Multiple Births Association (UK) We also wish to acknowledge the work of Lucas Calais Ferreira and Twins Research Australia’s team in coordinating the contributions and content. Further enquiries: Twins Research Australia School of Population and Global Health The University of Melbourne Level 3, 207 Bouverie Street, Carlton Victoria 3010 Australia Email enquiries [email protected] © First printed April 2019 For citation: Twins Research Australia (TRA). -

Multiple Pregnancy – Care Pathway
Multiple Pregnancy – Care Pathway This care pathway covers the level of care you should be offered from the time of your first hospital scan, in addition to the routine care that is offered to all women during pregnancy. It aims to reduce risks and improve outcomes for you and your babies. Ideally you should be seen by a specialist team, who have more knowledge about multiple pregnancies, all the time. This would include a midwife, sonographer and doctor. This pathway is based on national best practice and hospitals receive extra funding to look after multiple pregnancies. If you are not receiving the care you would expect please raise it with the PALS team (patient liaison) at your hospital and let us know – [email protected] . We can then liaise with the hospital regarding the correct level of care that should be offered. Feel free to share this with your midwifery team and use it as a checklist for each appointment. Different Types of Multiple Pregnancy There are different types of multiple pregnancy so each care pathway is slightly different. Twins can be dichorionic (they have separate placentas) or monochorionic (they share a placenta). Triplets have a few possible combinations: Trichorionic – each baby has a separate placenta Dichorionic – two of the babies share a placenta and the third baby is separate Monochorionic – all three babies share a placenta It is possible for twins and triplets to share an amniotic sac as well as a placenta. Although rare, these pregnancies need extra care, closer monitoring by a specialist and an individual care pathway. -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

Twins & Multiples
Twins & Multiples Study Group Module Twins & Multiples National Midwifery Institute, Inc. Study Group Coursework Syllabus Description: This module explores twins and multiples in midwifery care. It includes recommended reading materials in print and online, and asks students to complete short answer questions for assessment, long answer questions for deeper reflection, and learning activities/projects to deepen your hands- on direct application of key concepts. Learning Objectives: ● Review embryology and fetal development as it pertains to twins and multiples ● Understand the unique needs of twins and multiples in pregnancy. ● Identify the role of ultrasound to confirm suspected twins or multiples. ● Identify the cultural phenomenon of increased multiple pregnancy. ● Identify support measures for bringing twin pregnancies to term. ● Review the concepts of informed consent. ● Understand twins to be a variation of normal birth. ● Identify the risks of twins birth.’ ● Identify specific guidelines for attending twin and multiples births. ● Identify local doctors who are willing to attend twin and multiples births. ● Identify the local doctors who are willing to consult with community midwives on twins and multiples. ● Identify the local community standard among midwives regarding twin and multiples births. ● Identify management of a surprise twin birth. Learning Activities: ● Research and read appropriate study sources, seeking out additional study sources where needed ● Complete short answer questions in attached module document for assessment -

Healthy Moms, Healthy Kids: April 2011 a Series on Maternal and Child Health in Colorado
Healthy Moms, Healthy Kids: April 2011 A Series on Maternal and Child Health in Colorado Healthy Pregnancies “Healthy Pregnancies” is one in a series of six briefs published by the Colorado Children’s A woman’s behaviors during pregnancy can have a significant influence Campaign addressing maternal and child health on her baby’s healthy development. Women who smoke or drink topics titled Healthy Moms, Healthy Kids: A Series alcohol during pregnancy, go without prenatal care or suffer from on Maternal and Child Health in Colorado. Other poor nutrition are more likely to experience complications during topics in the series include domestic violence, pregnancy or childbirth, and their babies are at increased risk for maternal depression, family structure and teen developing a number of health problems. Regular prenatal care presents motherhood, social determinants of health and a key opportunity to inform expectant mothers about healthy behaviors nutrition. We wish to thank Kaiser Permanente during pregnancy and recognize risk factors associated with the leading for its generous support of this project. causes of infant mortality in the U.S. and Colorado. Low Birthweight The average weight for a newborn baby in the United States is about seven pounds.1 Approximately one in 12 U.S. babies, however, is born with low birthweight, classified as weighing less than five pounds, eight ounces at birth.2 The complications associated with low birthweight are numerous and can be severe. According to the Centers for Disease Control, complications related to low birthweight are a leading cause of infant mortality in the United States.3 Low birthweight also puts newborn babies at increased risk for a variety of acute health complications after birth, including respiratory distress syndrome and heart problems. -
Body Mass Index Assessment
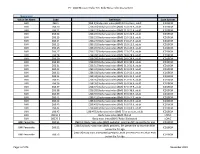
PT - 2020 Measure Value Set_Body Mass Index Assessment Numerator Value Set Name Code Definition Code System BMI Z68.1 [Z68.1] Body mass index (BMI) 19.9 or less, adult ICD10CM BMI Z68.20 [Z68.20] Body mass index (BMI) 20.0-20.9, adult ICD10CM BMI Z68.21 [Z68.21] Body mass index (BMI) 21.0-21.9, adult ICD10CM BMI Z68.22 [Z68.22] Body mass index (BMI) 22.0-22.9, adult ICD10CM BMI Z68.23 [Z68.23] Body mass index (BMI) 23.0-23.9, adult ICD10CM BMI Z68.24 [Z68.24] Body mass index (BMI) 24.0-24.9, adult ICD10CM BMI Z68.25 [Z68.25] Body mass index (BMI) 25.0-25.9, adult ICD10CM BMI Z68.26 [Z68.26] Body mass index (BMI) 26.0-26.9, adult ICD10CM BMI Z68.27 [Z68.27] Body mass index (BMI) 27.0-27.9, adult ICD10CM BMI Z68.28 [Z68.28] Body mass index (BMI) 28.0-28.9, adult ICD10CM BMI Z68.29 [Z68.29] Body mass index (BMI) 29.0-29.9, adult ICD10CM BMI Z68.30 [Z68.30] Body mass index (BMI) 30.0-30.9, adult ICD10CM BMI Z68.31 [Z68.31] Body mass index (BMI) 31.0-31.9, adult ICD10CM BMI Z68.32 [Z68.32] Body mass index (BMI) 32.0-32.9, adult ICD10CM BMI Z68.33 [Z68.33] Body mass index (BMI) 33.0-33.9, adult ICD10CM BMI Z68.34 [Z68.34] Body mass index (BMI) 34.0-34.9, adult ICD10CM BMI Z68.35 [Z68.35] Body mass index (BMI) 35.0-35.9, adult ICD10CM BMI Z68.36 [Z68.36] Body mass index (BMI) 36.0-36.9, adult ICD10CM BMI Z68.37 [Z68.37] Body mass index (BMI) 37.0-37.9, adult ICD10CM BMI Z68.38 [Z68.38] Body mass index (BMI) 38.0-38.9, adult ICD10CM BMI Z68.39 [Z68.39] Body mass index (BMI) 39.0-39.9, adult ICD10CM BMI Z68.41 [Z68.41] Body mass index (BMI) 40.0-44.9, -

Multiple Birth Statistics WHAT IS the LIKELIHOOD of HAVING TWINS OR MORE? in the UK About One in Every 65 Pregnancies Results in a Multiple Birth
Multiple birth statistics WHAT IS THE LIKELIHOOD OF HAVING TWINS OR MORE? In the UK about one in every 65 pregnancies results in a multiple birth. There has been an upward trend in the numbers over the last 20 years. The rise is attributed to fertility treatments, the survival rates of premature babies and women starting their families later. However, the multiple birth rate is now slowing in line with the singleton birth rate. Incidence of multiple births in the UK, 2019* England & Wales Scotland Northern Ireland UK Twins 9,656 717 384 10,757 Triplets and above 143 9 4 156 * source Office of National Statistics/General Registry Office, Scotland & Northern Ireland Statistics & Research Agency What are the chances of twins again are much higher. They may or may not share a placenta. having identical Women who have a family history (monozygotic) twins? of non-identical twins have a Characteristics such as size and The likelihood of having identical higher chance of producing non- personality depend on non- twins is about 1 in 250 (about identical twins themselves as genetic factors, so may be 0.5%). there is a genetically linked different. tendency to hyper-ovulate. Identical twins do not run in Triplets and more are formed in families. They occur when a There is no known genetic link for this way too, but may be in single embryo splits in two soon identical twinning. different combinations. after fertilisation. This is why Identical or non-identical? Non-identical twins are created identical twins have identical when a woman produces two Whether the babies are identical DNA. -

Multiple Birth Resources
Patient Education Maternity and Infant Center Multiple Birth Resources These resources are Newsletters/Magazines specially focused on the Milestones: A newsletter designed just for families who are concerns of families expecting multiples. Subscriptions are available and include seven issues, each one timed to arrive at the start of a new stage of expecting multiples. Be pregnancy, from the first trimester to postpartum. Include your sure to let us know if you babies’ due date when writing. Contact: Marvelous Multiples find a resource that is not Address: PO Box 467841, Atlanta, GA 31146 listed, so we may consider Telephone: (770) 242-2750 adding it to future The MOST Quarterly Magazine: Free with Mothers of Super Twins (MOST) membership. additions. (Please call Address: PO Box 951, Brentwood, NY 11717 Perinatal Education at Telephone: (516) 859-1110 Internet: www.mostonline.org (206) 598-4003.) Mothers of Twins Clubs Notebook: MOTC Notebook carries feature stories, columns, and research information about the lives of multiples and their families. Contact: National Organization of Mothers of Twins Clubs Address: PO Box 23188, Albuquerque, NM 87192-1188 Telephone: (800) 243-2276 Internet: www.nomotc.org The Triplet Quarterly: Published four times a year by The Triplet Connection. Address: PO Box 99571, Stockton, CA, 95209 Telephone: (209) 474-0885 Internet: www.tripletconnection.org Twins Magazine: Published six times a year, subscriptions available. New parent and expectant parent packets are available. Address: 5350 Roslyn Street, Englewood, CO, 80111 Telephone: (800)-328-3211 Internet: www.twinsmagazine.com Page 2 Maternity and Infant Center Multiple Birth Resources Books and Booklets Being a Twin, Having a Twin—Rosenberg, Maxine, 1985 Breastfeeding Twins—(booklet) La Leche League International, Books can be ordered from: (847)-519-7730 Child Safety Made Easy—Marques, Lori, Lisa Carter, and Mike 1. -
Twins, Triplets & More: Resource Guide for Multiple Pregnancy
Twins, Triplets & More! Resource Guide for Multiple Pregnancy & Parenthood March 2020: The Final (Last) Edition www.nursing.ubc.ca/pdfs/twinstripletsandmore.pdf One hour old http://allaboutcutybabies.blogspot.ca/2009/07/new-born-twins.html Linda G. Leonard, RN: Non-Practising, MSN Associate Professor, Emerita Multiple-Births Support Program University of British Columbia School of Nursing T201 2211 Wesbrook Mall Vancouver, BC V6T 2B5 CANADA e-mail: [email protected] http://community.babycenter.com/pcphoto/1873707 Dear Parents-to-be and Parents of Multiples Before and after a multiple birth, you likely will have many questions. You may ask: “How do I look after myself during a multiple pregnancy?” “How do I care for multiple infants?” “How will family life change for us?” “What kinds of help and support will we need? What is available? How do I find it?” “What equipment and supplies do we need?” “Are there any multiples-specific support groups, prenatal classes, web and social media sites, books, audiovisuals, and organizations?” This resource guide is designed for multiple-birth families living in Canada, particularly those in British Columbia and the BC Lower Mainland. Examples of products and businesses appear in the Guide for information purposes only and are not intended as an endorsement. The Guide contains web URL’s and e-mail addresses which you can click on. Please note: Resources and contact data change frequently. The information provided augments your medical and health care. It is not a substitute for professional health care advice, diagnosis or treatment. When you have questions or concerns about what action to take, please seek the advice of qualified health care providers. -

Complications of Multiple Pregnancies. Overwiew
Trakia Journal of Sciences, No 1, pp.108-111, 2016 Copyright © 2016 Trakia University Available online at: http://www.uni-sz.bg ISSN 1313-7050 (print) ISSN 1313-3551 (online) doi:10.15547/tjs.2016.01.016 Rewiew COMPLICATIONS OF MULTIPLE PREGNANCIES. OVERWIEW S. Lazarov, L. Lazarov, N. Lazarov Department of Obstetrics and Gynecology, Medical Faculty, Trakia University, Stara Zagora, Bulgaria ABSTRACT Multiple gestations are high risk pregnancies which may be complicated by prematurity,low birthweight, pre- eclampsia, anaemia, postpartum haemorrhage, intrauterine growth restriction, neonatal morbidity and high neonatal and infant mortality. Preterm labor and birth represent the greatest risk to a multiple pregnancy. Sixty percent of multiples are born prematurely (<37 weeks) compared to about 10% of singleton pregnancies. Placental function is more likely to be abnormal in a multiple pregnancy. Another placental problem is twin- twin transfusion, a life-threatening condition in identical twins. Preeclampsia, also known as toxemia, occurs 2 to 5 times more often in multiple pregnancies. Fifteen percent to 20% of women with twin pregnancies will experience preeclampsia, and an even higher percentage is preeclamptic in triplet or high-order pregnancies. Preterm labor and birth pose the greatest risk to a multiple pregnancy. Sixty percent of multiples are born prematurely (<37 weeks) compared to about 10% of singleton pregnancies. Fetal and Newborn complications such as preterm delivery, respiratory distress syndrome, brain damage are responsible for almost 10% of premature newborn deaths. Birth defects and stillbirths account for about 30% of the deaths in twins and multiple pregnancies. Low birth weight of less than 5.5 pounds (lb.) [2,500 grams] occurs in over half of twins.