A. OHA At-A-Glance B. Mission C. Statutory Responsibilities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PUBLIC NOTICE Federal Communications Commission News Media Information 202/418-0500 Fax-On-Demand 202/418-2830 445 12Th St., S.W
PUBLIC NOTICE Federal Communications Commission News media information 202/418-0500 Fax-On-Demand 202/418-2830 445 12th St., S.W. Internet: http://www.fcc.gov Washington, D.C. 20554 ftp.fcc.gov Report No. 480 Media Bureau Call Sign Actions 09/29/2004 During the period from 08/04/2004 to 09/27/2004 the Commission accepted applications to assign call signs to, or change the call signs of the following broadcast stations. Call Signs Reserved for Pending Sales Applicants Former Call Call Sign Service Requested By City State File-Number Sign KCUN- BALTTL- LP EBC KANSAS CITY, INC. KANSAS CITY MO K48FS LP 20040810ABI AUBURN-FEDERAL KDDS AM BUSTOS MEDIA OF WASHINGTON, LLC WA BAL-20040728AMX KNWX WAY KJJP FM KANZA SOCIETY, INC. AMARILLO TX BALH-20040513AAC KAEZ BALED- KKRD FM EDUCATIONAL MEDIA FOUNDATION ENID OK KBVV 20040714AAY KLRJ FM EDUCATIONAL MEDIA FOUNDATION ABERDEEN SD BALH-20040818ABQ KQAA KOGN AM AM RADIO 1490, INC. OGDEN UT 20040728AHH KYFO KROI FM RADIO ONE LICENSES, LLC SEABROOK TX BALH-20040526AHW KRTS KSAC AM DIAMOND BROADCASTING SACRAMENTO CA BAL-20040729ASU KSQR WDTK AM PENNSYLVANIA MEDIA ASSOCIATES, INC. DETROIT MI 20040326AKW WQBH MILLENNIUM ATLANTIC CITY II LICENSE HOLDCO, WSJO FM EGG HARBOR CITY NJ BALH-20040702AAN WOJZ LLC New or Modified Call Signs Row Effective Former Call Sign Service Assigned To City State File Number Number Date Call Sign 1 08/04/2004 KJJC-LP LP AMANDA ORRICK HELENA MT K34HL 2 08/04/2004 KMRE-LP FL AMERICAN MUSEUM OF RADIO, THE BELLINGHAM WA 20010612AGM New IGLESIA DEL CUERPO DE CRISTO OF 3 08/04/2004 KYLP-LP FL GREENVILLE TX 20010615AZH New GREENVILLE 4 08/04/2004 WGDQ FM UNITY BROADCASTERS HATTIESBURG MS 19930208MC New VAN ZANDT COMMUNITY HALL 5 08/05/2004 KAVZ-LP FL DEMING WA KNOO-LP ASSOCIATION 6 08/08/2004 WJRF FM REFUGE MEDIA GROUP DULUTH MN WNCB GOODLAND 7 08/09/2004 WHYT FM SUPERIOR COMMUNICATIONS MI WWKM TOWNSHIP 8 08/09/2004 WKEP-LP FL KEEPERS OF THE PLEDGE, INC. -

Revitalization of the AM Radio Service ) ) ) )
Before the FEDERAL COMMUNICATIONS COMMISSION Washington, DC In the matter of: ) ) Revitalization of the AM Radio Service ) MB Docket 13-249 ) ) COMMENTS OF REC NETWORKS One of the primary goals of REC Networks (“REC”)1 is to assure a citizen’s access to the airwaves. Over the years, we have supported various aspects of non-commercial micro- broadcast efforts including Low Power FM (LPFM), proposals for a Low Power AM radio service as well as other creative concepts to use spectrum for one way communications. REC feels that as many organizations as possible should be able to enjoy spreading their message to their local community. It is our desire to see a diverse selection of voices on the dial spanning race, culture, language, sexual orientation and gender identity. This includes a mix of faith-based and secular voices. While REC lacks the technical knowledge to form an opinion on various aspects of AM broadcast engineering such as the “ratchet rule”, daytime and nighttime coverage standards and antenna efficiency, we will comment on various issues which are in the realm of citizen’s access to the airwaves and in the interests of listeners to AM broadcast band stations. REC supports a limited offering of translators to certain AM stations REC feels that there is a segment of “stand-alone” AM broadcast owners. These owners normally fall under the category of minority, women or GLBT/T2. These owners are likely to own a single AM station or a small group of AM stations and are most likely to only own stations with inferior nighttime service, such as Class-D stations. -

Voice of the Broadcasting Industry Volume 23, Issue 10
October 2006 Voice of the Broadcasting Industry Volume 23, Issue 10 $8.00 USA $12.50 Canada-Foreign RADIO NEWS ® Will Nielsen enter New PPM to track non-encoding stations radio ratings derby? It looks like Cox Radio CEO Bob Neil will no longer be able to boycott the The Next-Generation Electronics Ratings Evalu- Houston test of Arbitron’s Portable People Meter (PPM) by refusing to let his ation Team, led by Clear Channel Radio, has stations encode. Arbitron announced that it is now field testing a PPM system been trying to pick between Arbitron’s PPM and which uses sound matching for non-encoding stations—a dual-function system the Smart Cell Phone-based system from The much like that of the competing system by The Media Audit/Ipsos. Media Audit/Ipsos for passive electronic radio While the main test panel in Houston is still using PPM devices that track only audience measurement. But now there is word encoding stations, Arbitron said it has successfully downloaded software upgrades to that the Next-Gen has also approached Nielsen current generations PPMs still held by 50 former panelists who are participating in the Media Research about making its own entry, dual-function test. The software upgrade was delivered via home phone lines. Arbitron now that it has rejected a PPM joint venture said it will now be testing to ensure that sound matching results are consistent with with Arbitron. But it is not clear that Nielsen is those already validated by encoded PPM data gathering. chomping at the bit to join the radio race. -

List of Radio Stations in Connecticut
Not logged in Talk Contributions Create account Log in Article Talk Read Edit View history Search Wikipedia List of radio stations in Connecticut From Wikipedia, the free encyclopedia Main page The following is a list of FCC-licensed radio stations in the U.S. state of Connecticut, which can be Contents sorted by their call signs, frequencies, cities of license, licensees, and programming formats. Featured content Current events Call City of license Frequency Licensee [1][2] Format [3][4] Random article sign [1][2] Donate to Wikipedia WACC- Asnuntuck Community Wikipedia store 107.7 FM Enfield Adult Alternative LP College Interaction WADS 690 AM Ansonia Radio Amor, Inc. Spanish Religious Help Torrington Community Radio About Wikipedia WAPJ 89.9 FM Torrington Community Community portal Foundation, Inc. Recent changes WATR 1320 AM Waterbury WATR, Inc. News/Talk/Oldies Contact page WAVZ 1300 AM New Haven CC Licenses, LLC Sports Tools The Berkshire Broadcasting WAXB 850 AM Ridgefield Classic Hits What links here Corp. Related changes Red Wolf Broadcasting Upload file WBMW 106.5 FM Pawcatuck Adult contemporary Special pages Corporation open in browser PRO version Are you a developer? Try out the HTML to PDF API pdfcrowd.com Permanent link WBVC 91.1 FM Pomfret Pomfret School Variety Page information Christian Wikidata item Educational Media WCCC 106.9 FM Hartford contemporary (K- Cite this page Foundation Love) Print/export WCFV- Calvary Fellowship of Create a book 101.7 FM Willimantic Religious Teaching LP Willimantic Download as PDF Printable version Connecticut College WCNI 90.9 FM New London Freeform Community Radio, Inc. -

530 CIAO BRAMPTON on ETHNIC AM 530 N43 35 20 W079 52 54 09-Feb
frequency callsign city format identification slogan latitude longitude last change in listing kHz d m s d m s (yy-mmm) 530 CIAO BRAMPTON ON ETHNIC AM 530 N43 35 20 W079 52 54 09-Feb 540 CBKO COAL HARBOUR BC VARIETY CBC RADIO ONE N50 36 4 W127 34 23 09-May 540 CBXQ # UCLUELET BC VARIETY CBC RADIO ONE N48 56 44 W125 33 7 16-Oct 540 CBYW WELLS BC VARIETY CBC RADIO ONE N53 6 25 W121 32 46 09-May 540 CBT GRAND FALLS NL VARIETY CBC RADIO ONE N48 57 3 W055 37 34 00-Jul 540 CBMM # SENNETERRE QC VARIETY CBC RADIO ONE N48 22 42 W077 13 28 18-Feb 540 CBK REGINA SK VARIETY CBC RADIO ONE N51 40 48 W105 26 49 00-Jul 540 WASG DAPHNE AL BLK GSPL/RELIGION N30 44 44 W088 5 40 17-Sep 540 KRXA CARMEL VALLEY CA SPANISH RELIGION EL SEMBRADOR RADIO N36 39 36 W121 32 29 14-Aug 540 KVIP REDDING CA RELIGION SRN VERY INSPIRING N40 37 25 W122 16 49 09-Dec 540 WFLF PINE HILLS FL TALK FOX NEWSRADIO 93.1 N28 22 52 W081 47 31 18-Oct 540 WDAK COLUMBUS GA NEWS/TALK FOX NEWSRADIO 540 N32 25 58 W084 57 2 13-Dec 540 KWMT FORT DODGE IA C&W FOX TRUE COUNTRY N42 29 45 W094 12 27 13-Dec 540 KMLB MONROE LA NEWS/TALK/SPORTS ABC NEWSTALK 105.7&540 N32 32 36 W092 10 45 19-Jan 540 WGOP POCOMOKE CITY MD EZL/OLDIES N38 3 11 W075 34 11 18-Oct 540 WXYG SAUK RAPIDS MN CLASSIC ROCK THE GOAT N45 36 18 W094 8 21 17-May 540 KNMX LAS VEGAS NM SPANISH VARIETY NBC K NEW MEXICO N35 34 25 W105 10 17 13-Nov 540 WBWD ISLIP NY SOUTH ASIAN BOLLY 540 N40 45 4 W073 12 52 18-Dec 540 WRGC SYLVA NC VARIETY NBC THE RIVER N35 23 35 W083 11 38 18-Jun 540 WETC # WENDELL-ZEBULON NC RELIGION EWTN DEVINE MERCY R. -

Exhibit 2181
Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 1 of 4 Electronically Filed Docket: 19-CRB-0005-WR (2021-2025) Filing Date: 08/24/2020 10:54:36 AM EDT NAB Trial Ex. 2181.1 Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 2 of 4 NAB Trial Ex. 2181.2 Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 3 of 4 NAB Trial Ex. 2181.3 Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 4 of 4 NAB Trial Ex. 2181.4 Exhibit 2181 Case 1:18-cv-04420-LLS Document 132 Filed 03/23/20 Page 1 of 1 NAB Trial Ex. 2181.5 Exhibit 2181 Case 1:18-cv-04420-LLS Document 133 Filed 04/15/20 Page 1 of 4 ATARA MILLER Partner 55 Hudson Yards | New York, NY 10001-2163 T: 212.530.5421 [email protected] | milbank.com April 15, 2020 VIA ECF Honorable Louis L. Stanton Daniel Patrick Moynihan United States Courthouse 500 Pearl St. New York, NY 10007-1312 Re: Radio Music License Comm., Inc. v. Broad. Music, Inc., 18 Civ. 4420 (LLS) Dear Judge Stanton: We write on behalf of Respondent Broadcast Music, Inc. (“BMI”) to update the Court on the status of BMI’s efforts to implement its agreement with the Radio Music License Committee, Inc. (“RMLC”) and to request that the Court unseal the Exhibits attached to the Order (see Dkt. -

CT FY15 Highway Safety Annual Report
Connecticut Highway Safety Federal Fiscal Year 2015 Prepared by Connecticut Department of Transportation Bureau of Policy and Planning Highway Safety Office P.O. Box 317546 2800 Berlin Turnpike Newington, Connecticut 06131-7546 1 Table of Contents INTRODUCTION ............................................................................................................................................. 1 CRASH DATA/TRENDS ................................................................................................................................... 4 CORE PERFORMANCE MEASURES/GOALS AND TRENDS .............................................................................. 7 FINANCIAL SUMMARY................................................................................................................................. 20 Project Listing ........................................................................................................................................ 222 PROGRAM AREAS ...................................................................................................................................... 278 Impaired Driving...................................................................................................................................... 29 Occupant Protection ............................................................................................................................... 44 Child Passenger Safety ........................................................................................................................... -

Bulkeley High School Student Handbook
BULKELEY HIGH SCHOOL STUDENT HANDBOOK 2019-2020 ADMINISTRATION Digna A. Marte, Principal Dianne Georgantas, Assistant Principal Justin B. Nolan, Assistant Principal Brooke Lafreniere, Assistant Principal Re-imagining learning and teaching, while building our legacy one child at a time based on strong relationships and high expectations for all!!! Every day is an opportunity to be better and do better than the day before!!! “Borrón y Cuenta Nueva” BULKELEY HIGH SCHOOL 300 Wethersfield Avenue Telephone: (860) 695-1000 Hartford, CT 06114 Fax #: (860) 247 - 3491 Bulkeley High School Statement of Core Values and Beliefs The Bulkeley High School community believes that all students can become responsible, independent individuals possessing the academic, social, and civic competencies for the 21st century. We value high academic standards, individualized learning experiences, and specialized programs of study that meet the needs of a diverse student population. Academic Learning Expectations: ● Read, write, and speak effectively in a variety of forms and contexts ● Effectively analyze and evaluate evidence, arguments, and theories ● Apply critical and emergent thinking skills in a global community Social Learning Expectations: ● Utilize time and manage workload efficiently ● Interact and collaborate with diverse populations Civic Learning Expectations: ● Obtain knowledge and skills to become an involved, responsible citizen ● Understand and apply civic and personal rights within a democratic society BULKELEY HIGH SCHOOL A BRIEF HISTORY MORGAN GARDNER BULKELEY (1837-1922) Morgan Gardner Bulkeley was a man whose interest spanned many fields. Besides working at his family business, the Aetna Life Insurance Company, and serving as its president for 44 years, he was a City Councilman, Mayor of Hartford, Governor of Connecticut and then a U.S. -

TV Channel 5-6 Radio Proposal
Before the Federal Communications Commission Washington, D.C. 20554 In the Matter of ) ) Promoting Diversification of Ownership ) MB Docket No 07-294 in the Broadcasting Services ) ) 2006 Quadrennial Regulatory Review – Review of ) MB Docket No. 06-121 the Commission’s Broadcast Ownership Rules and ) Other Rules Adopted Pursuant to Section 202 of ) the Telecommunications Act of 1996 ) ) 2002 Biennial Regulatory Review – Review of ) MB Docket No. 02-277 the Commission’s Broadcast Ownership Rules and ) Other Rules Adopted Pursuant to Section 202 of ) the Telecommunications Act of 1996 ) ) Cross-Ownership of Broadcast Stations and ) MM Docket No. 01-235 Newspapers ) ) Rules and Policies Concerning Multiple Ownership ) MM Docket No. 01-317 of Radio Broadcast Stations in Local Markets ) ) Definition of Radio Markets ) MM Docket No. 00-244 ) Ways to Further Section 257 Mandate and To Build ) MB Docket No. 04-228 on Earlier Studies ) To: Office of the Secretary Attention: The Commission BROADCAST MAXIMIZATION COMMITTEE John J. Mullaney Mark Lipp Paul H. Reynolds Bert Goldman Joseph Davis, P.E. Clarence Beverage Laura Mizrahi Lee Reynolds Alex Welsh SUMMARY The Broadcast Maximization Committee (“BMC”), composed of primarily of several consulting engineers and other representatives of the broadcast industry, offers a comprehensive proposal for the use of Channels 5 and 6 in response to the Commission’s solicitation of such plans. BMC proposes to (1) relocate the LPFM service to a portion of this spectrum space; (2) expand the NCE service into the adjacent portion of this band; and (3) provide for the conversion and migration of all AM stations into the remaining portion of the band over an extended period of time and with digital transmissions only. -
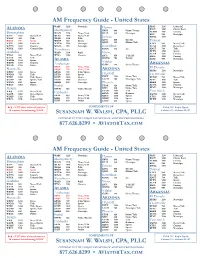
AM Radio Guide Version 1.4 For
AM Frequency Guide - United States LABAMA WABF 1220 Nostalgia Homer KISO 1230 Urban AC A KSLX 1440 Classic Rock Montgomery KBBI 890 News/Variety KCWW 1580 Country Birmingham WACV 1170 News/Talk KGTL 620 Nostalgia KOY 550 Nostalgia WAPI 1070 News/Talk WLWI 1440 News/Talk KMYL 1190 WERC 960 Talk WIQR 1410 Talk Juneau WJOX 690 Sports WMSP 740 Sports KINY 800 Hot AC Tucson WJLD 1400 Urban AC WTLM 1520 Nostalgia KJNO 630 Oldies/Talk KTKT 990 News/Talk WFHK 1430 Country WNZZ 950 Nostalgia Ketchikan KUAT 1550 News/Jazz WPYK 1010 Country Olds Tuscaloosa KTKN 930 AC KNST 790 Talk KFFN 1490 Sports Gadsden WAJO 1310 R&B Nome KCUB 1290 Country WNSI 810 News/Talk WVSA 1380 Country KICY 850 Talk/AC KHIL 1250 Country WAAX 570 Talk KNOM 780 Variety KSAZ 580 Nostalgia WHMA 1390 Sports ALASKA WZOB 1250 Country Valdez ARKANSAS WGAD 1350 Oldies Anchorage KCHU 770 News/Variety KENI 650 News/Talk El Dorado Huntsville KFQD 750 News/Talk ARIZONA KDMS 1290 Nostalgia WBHP 1230 News KBYR 700 Talk/Sports WVNN 770 Talk KTZN 550 Sports Flagstaff Fayetteville WTKI 1450 Talk/Sports KAXX 1020 Sports KYET 1180 News/Talk KURM 790 News/Talk WUMP 730 Sports/Talk KASH 1080 Classical KAZM 780 Nostalgia/Talk KFAY 1030 Talk WZNN 620 Sports KHAR 590 Nostalgia Phoenix KREB 1390 Sports WKAC 1080 Oldies Bethel KTAR 620 News/Talk KUOA 1290 Country KESE 1190 Nostalgia Mobile KYUK 640 News/Variety KFYI 910 News/Talk WKSJ 1270 News/Talk KXAM 1310 Talk Fort Smith WABB 1480 News/Sports Fairbanks KFNN 1510 Business KWHN 1320 News/Talk WHEP 1310 Talk KFAR 660 News/Talk KDUS 1060 Sports KTCS 1410 Country KIAK 970 News/Talk WBCA 1110 Country Olds KGME 1360 Sports KFPW 1230 Nostalgia KCBF 820 Oldies KMVP 860 Sports Red = FCC clear channel stations COMPLIMENTS OF AM & HF Radio Guide & stations broadcasting 50 KW SUSANNAH W. -
Freq Call State Location U D N C Distance Bearing
AM BAND RADIO STATIONS COMPILED FROM FCC CDBS DATABASE AS OF FEB 6, 2012 POWER FREQ CALL STATE LOCATION UDNCDISTANCE BEARING NOTES 540 WASG AL DAPHNE 2500 18 1107 103 540 KRXA CA CARMEL VALLEY 10000 500 848 278 540 KVIP CA REDDING 2500 14 923 295 540 WFLF FL PINE HILLS 50000 46000 1523 102 540 WDAK GA COLUMBUS 4000 37 1241 94 540 KWMT IA FORT DODGE 5000 170 790 51 540 KMLB LA MONROE 5000 1000 838 101 540 WGOP MD POCOMOKE CITY 500 243 1694 75 540 WXYG MN SAUK RAPIDS 250 250 922 39 540 WETC NC WENDELL-ZEBULON 4000 500 1554 81 540 KNMX NM LAS VEGAS 5000 19 67 109 540 WLIE NY ISLIP 2500 219 1812 69 540 WWCS PA CANONSBURG 5000 500 1446 70 540 WYNN SC FLORENCE 250 165 1497 86 540 WKFN TN CLARKSVILLE 4000 54 1056 81 540 KDFT TX FERRIS 1000 248 602 110 540 KYAH UT DELTA 1000 13 415 306 540 WGTH VA RICHLANDS 1000 97 1360 79 540 WAUK WI JACKSON 400 400 1090 56 550 KTZN AK ANCHORAGE 3099 5000 2565 326 550 KFYI AZ PHOENIX 5000 1000 366 243 550 KUZZ CA BAKERSFIELD 5000 5000 709 270 550 KLLV CO BREEN 1799 132 312 550 KRAI CO CRAIG 5000 500 327 348 550 WAYR FL ORANGE PARK 5000 64 1471 98 550 WDUN GA GAINESVILLE 10000 2500 1273 88 550 KMVI HI WAILUKU 5000 3181 265 550 KFRM KS SALINA 5000 109 531 60 550 KTRS MO ST. LOUIS 5000 5000 907 73 550 KBOW MT BUTTE 5000 1000 767 336 550 WIOZ NC PINEHURST 1000 259 1504 84 550 WAME NC STATESVILLE 500 52 1420 82 550 KFYR ND BISMARCK 5000 5000 812 19 550 WGR NY BUFFALO 5000 5000 1533 63 550 WKRC OH CINCINNATI 5000 1000 1214 73 550 KOAC OR CORVALLIS 5000 5000 1071 309 550 WPAB PR PONCE 5000 5000 2712 106 550 WBZS RI -

State of Connecticut Highway Safety Program Federal
State of Connecticut Highway Safety Program Federal Fiscal Year 2008 Connecticut Highway Safety Federal Fiscal Year 2008 Prepared by Connecticut Department of Transportation Bureau of Policy and Planning Transportation Safety Section P.O. Box 317546 2800 Berlin Turnpike Newington, Connecticut 06131-7546 INTRODUCTION........................................................................... 1 CRASH DATA/TRENDS ............................................................... 5 PERFORMANCE GOALS AND TRENDS .................................... 7 FINANCIAL SUMMARY .............................................................. 15 PROGRAM AREAS .................................................................... 17 Impaired Driving ....................................................................... 18 Police Traffic Services.............................................................. 21 Occupant Protection................................................................. 24 Child Passenger Safety............................................................ 27 Roadway Safety ....................................................................... 30 Motorcycle Safety..................................................................... 31 Traffic Records ......................................................................... 33 PAID MEDIA REPORT ............................................................... 35 NOTEWORTHY PRACTICES..................................................... 47 INTRODUCTION 1 INTRODUCTION The Connecticut Department