Peripheral Artery Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Evolution of Invasive Cerebral Vasospasm Treatment in Patients
Neurosurgical Review (2019) 42:463–469 https://doi.org/10.1007/s10143-018-0986-5 ORIGINAL ARTICLE The evolution of invasive cerebral vasospasm treatment in patients with spontaneous subarachnoid hemorrhage and delayed cerebral ischemia—continuous selective intracarotid nimodipine therapy in awake patients without sedation Andrej Paľa1 & Max Schneider1 & Christine Brand 1 & Maria Teresa Pedro1 & Yigit Özpeynirci2 & Bernd Schmitz2 & Christian Rainer Wirtz1 & Thomas Kapapa1 & Ralph König1 & Michael Braun2 Received: 16 February 2018 /Revised: 1 May 2018 /Accepted: 17 May 2018 /Published online: 26 May 2018 # Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Cerebral vasospasm (CV) and delayed cerebral ischemia (DCI) are major factors that limit good outcome in patients with spontaneous subarachnoid hemorrhage (SAH). Continuous therapy with intra-arterial calcium channel blockers has been intro- duced as a new step in the invasive treatment cascade of CV and DCI. Sedation is routinely necessary for this procedure. We report about the feasibility to apply this therapy in awake compliant patients without intubation and sedation. Out of 67 patients with invasive endovascular treatment of cerebral vasospasm due to spontaneous SAH, 5 patients underwent continuous superselective intracarotid nimodipine therapy without intubation and sedation. Complications, neurological improvement, and outcome at discharge were summarized. Very good outcome was achieved in all 5 patients. The Barthel scale was 100 and the modified Rankin scale 0–1 in all cases at discharge. We found no severe complications and excellent neurological monitoring was possible in all cases due to patients’ alert status. Symptoms of DCI resolved within 24 h in all 5 cases. We could demonstrate the feasibility and safety of selective intracarotid arterial nimodipine treatment in awake, compliant patients with spontaneous SAH and symptomatic CVand DCI. -

Control Study of Pregnancy Complications and Birth Outcomes
Hypertension Research (2011) 34, 55–61 & 2011 The Japanese Society of Hypertension All rights reserved 0916-9636/11 $32.00 www.nature.com/hr ORIGINAL ARTICLE Hypotension in pregnant women: a population-based case–control study of pregnancy complications and birth outcomes Ferenc Ba´nhidy1,Na´ndor A´ cs1, Erzse´bet H Puho´ 2 and Andrew E Czeizel2 Hypotension is frequent in pregnant women; nevertheless, its association with pregnancy complications and birth outcomes has not been investigated. Thus, the aim of this study was to analyze the possible association of hypotension in pregnant women with pregnancy complications and with the risk for preterm birth, low birthweight and different congenital abnormalities (CAs) in the children of these mothers in the population-based data set of the Hungarian Case–Control Surveillance of CAs, 1980–1996. Prospectively and medically recorded hypotension was evaluated in 537 pregnant women who later had offspring with CAs (case group) and 1268 pregnant women with hypotension who later delivered newborn infants without CAs (control group); controls were matched to sex and birth week of cases (in the year when cases were born), in addition to residence of mothers. Over half of the pregnant women who had chronic hypotension were treated with pholedrine or ephedrine. Maternal hypotension is protective against preeclampsia; however, hypotensive pregnant women were at higher risk for severe nausea or vomiting, threatened abortion (hemorrhage in early pregnancy) and for anemia. There was no clinically important difference in the rate of preterm births and low birthweight newborns in pregnant women with or without hypotension. The comparison of the rate of maternal hypotension in cases with 23 different CAs and their matched controls did not show a higher risk for CAs (adjusted OR with 95% confidence intervals: 0.66, 0.49–0.84). -

PERIPHERAL ARTERIAL DISEASES Postgrad Med J: First Published As 10.1136/Pgmj.22.243.22 on 1 January 1946
PERIPHERAL ARTERIAL DISEASES Postgrad Med J: first published as 10.1136/pgmj.22.243.22 on 1 January 1946. Downloaded from By SAUL S. SAMUELS, A.M., M.D. New York, N.Y. Arterial Diseases arteries that might be mentioned, but clinical Peripheral evidence of which is difficult to determine. They This new specialty has evolved within the past are encountered so infrequently that it hardly twenty years into a separate and distinct branch of seems important to devote much time to them. medicine and surgery. In its infancy it was rele- Among these may be mentioned syphilitic arteritis, gated to the internist who had some special interest tuberculosis of the peripheral arteries and certain in this work, just as in the early days of urology an non-specific forms of peripheral arteritis, which acquaintance with venereal diseases was sufficient have as yet been incompletely studied. for the designation of specialist in this field. In the field of functional disturbances of the peripheral arterial system, we consider two main General sub-groups. The first, and more important of Considerations these is Raynaud's Disease. This is a disturbance The peripheral arterial diseases may be separated of the control mechanism of the peripheral arteri- into two definite groups. The first and more oles which causes frequent attacks of vasospasm important is that of the changes in the arterial in the extremities and in the various acral parts of walls. These two groups may be again sub- the body, such as the tip of the nose, tongue and divided so that in the organic field we recognise ears. -

Vasculitis: Pearls for Early Diagnosis and Treatment of Giant Cell Arteritis
Vasculitis: Pearls for early diagnosis and treatment of Giant Cell Arteritis Mary Beth Humphrey, MD, PhD Professor of Medicine McEldowney Chair of Immunology [email protected] Office Phone: 405 271-8001 ext 35290 October 2019 Relevant Disclosure and Resolution Under Accreditation Council for Continuing Medical Education guidelines disclosure must be made regarding relevant financial relationships with commercial interests within the last 12 months. Mary Beth Humphrey I have no relevant financial relationships or affiliations with commercial interests to disclose. Experimental or Off-Label Drug/Therapy/Device Disclosure I will be discussing experimental or off-label drugs, therapies and/or devices that have not been approved by the FDA. Objectives • To recognize early signs of vasculitis. • To discuss Tocilizumab (IL-6 inhibitor) as a new treatment option for temporal arteritis. • To recognize complications of vasculitis and therapies. Professional Practice Gap Gap 1: Application of imaging recommendations in large vessel vasculitis Gap 2: Application of tocilizimab in treatment of giant cell vasculitis Cranial Symptoms Aortic Vision loss Aneurysm GCA Arm PMR Claudication FUO Which is not a risk factor or temporal arteritis? A. Smoking B. Female sex C. Diabetes D. Northern European ancestry E. Age Which is not a risk factor or temporal arteritis? A. Smoking B. Female sex C. Diabetes D. Northern European ancestry E. Age Giant Cell Arteritis • Most common form of systemic vasculitis in adults – Incidence: ~ 1/5,000 persons > 50 yrs/year – Lifetime risk: 1.0% (F) 0.5% (M) • Cause: unknown At risk: Women (80%) > men (20%) Northern European ancestry>>>AA>Hispanics Age: average age at onset ~73 years Smoking: 6x increased risk Kermani TA, et al Ann Rheum Dis. -
Jordan M. Garrison, Md Facs Fasmbs What Are We Talking About?
PERIPHERAL VASCULAR DISEASE JORDAN M. GARRISON, MD FACS FASMBS WHAT ARE WE TALKING ABOUT? Peripheral Arterial Disease (PAD) • Near or Complete obstruction of > 1 Peripheral Artery Peripheral Venous Reflux Disease • Varicose Veins • Chronic Venous Stasis Ulcer Disease • Phlegmasia Cerulia Dolans or Alba Dolans (Milk Leg) • Deep Vein Thrombosis and Pulmonary Embolus Disease Coronary Artery Disease ◦ Myocardial Infarct Aneurysmal Disease • Aortic • Popliteal Cerebral and Carotid Artery Disease • Stroke • TIA Renal Vascular Hypertensive Disease • High Blood Pressure • Kidney Failure Peripheral Arterial Disease PREVELANCE Males > Females 10% of People over 60 Race • AA double the rate of all other ethnicities High Income Countries Peripheral Arterial Disease RISK FACTORS Smoking is the #1 risk factor Diabetes Mellitus Diet Obesity ETOH Cholesterol Heredity Lifestyle Homocysteine, C Reactive Protein, Fibrinogen Arterial Anatomy Lower Extremity Anatomy Plaque Formation Plaque Peripheral Arterial Disease Claudication • Disabling • Intestinal Limb Threatening Ischemia(LTI) Critical Limb Ischemia(CLI) • Rest Pain • Tissue Loss • Gangrene Disabling Claudication Intestinal Ischemia Intestinal Claudication Peripheral Arterial Disease Claudication • Disabling • Intestinal Limb Threatening Ischemia(LTI) Critical Limb Ischemia(CLI) • Rest Pain • Tissue Loss • Gangrene Rest Pain/ Dependent Rubor Tissue Loss Gangrene Peripheral Artery Disease Diagnosis Segmental Pressures • Lower extremity Blood Pressures ABI • Nl >1.0, Diabetes will give elevated reading -

Definitions • Septic Shock
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Ann Rheum Dis Definitions • Septic shock: Persisting hypotension despite volume resuscitation, requiring vasopressors to maintain mean artery pressure (MAP) ≥65 mmHg and serum lactate level >2 mmol/L (1). • Renal failure: Doubling of basal Creatinine value or urine output <0.5 ml/kg/h for ≥12h (2) • Heart failure: Gradual or rapid change in heart failure signs and symptoms resulting in a need for urgent therapy (3). • Myocarditis: Myocarditis was diagnosed if serum levels of high-sensitivity cardiac troponin I were above the 99th percentile upper reference limit and compatible abnormalities were shown in electrocardiography and echocardiography. • Encephalopathy: Impaired consciousness as change of consciousness level (somnolence, stupor, and coma) or consciousness content (confusion and delirium) (4). • Thrombosis: Clinically or by imaging diagnosed acute pulmonary embolism (PE), deep-vein thrombosis, ischemic stroke, myocardial infarction or systemic arterial embolism (5). References 1. World Health Organization. Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance. 2020. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection- when-novel-coronavirus-(ncov)-infection-is-suspected. 2. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 2012;120:c179-84. 10.1159/000339789. 3. Gheorghiade M, Zannad F, Sopko G, et al. Acute heart failure syndromes: current state and framework for future research. Circulation. 2005;112(25):3958-3968. 4. Mao L, Jin H, Wang M, et al. -

Hypertension: Putting the Pressure on the Silent Killer
HYPERTENSION: PUTTING THE PRESSURE ON THE SILENT KILLER MAY 2016 TABLEHypertension: putting OF the CONTENTS pressure on the silent killer Table of contents UNDERSTANDING HYPERTENSION AND THE LINK TO CARDIOVASCULAR DISEASE 2 Understanding hypertension and the link to cardiovascular disease THEThe social SOCIAL and economic AND impact ECONOMIC of hypertension IMPACT OF HYPERTENSION 3 Diagnosing and treating hypertension – what is out there? DIAGNOSINGChallenges to tackling hypertension AND TREATING HYPERTENSION – WHAT IS OUT THERE? 6 Opportunities and focus areas for policymakers CHALLENGES TO TACKLING HYPERTENSION 9 OPPORTUNITIES AND FOCUS AREAS FOR POLICYMAKERS 15 HYPERTENSION: PUTTING THE PRESSURE ON THE SILENT KILLER UNDERSTANDING HYPERTENSION AND THE LINK TO CARDIOVASCULAR DISEASE Cardiovascular disease (CVD), or heart disease, is the number one cause of death in the world. 80% of deaths due to CVD occur in countries and poor communities where health systems are weak, and CVD accounts for nearly half of the estimated US$500 billion annual lost economic output associated with noncommunicable diseases (NCDs) in low-income and middle-income countries. In 2012, CVD killed 17.5 million people – the equivalent of every 3 in 10 deaths.1 Of these 17 million deaths a year, over half – 9.4 million - are caused by complications in hypertension, also commonly referred to as raised or high blood pressure2. Hypertension is a risk factor for coronary heart disease and the single most important risk factor for stroke - it is responsible for at least 45% of deaths due to heart disease, and at least 51% of deaths due to stroke. High blood pressure is defined as a systolic blood pressure at or above 140 mmHg and/or a diastolic blood pressure at or above 90 mmHg. -

Hypertension and Coronary Heart Disease
Journal of Human Hypertension (2002) 16 (Suppl 1), S61–S63 2002 Nature Publishing Group All rights reserved 0950-9240/02 $25.00 www.nature.com/jhh Hypertension and coronary heart disease E Escobar University of Chile, Santiago, Chile The association of hypertension and coronary heart atherosclerosis, damage of arterial territories other than disease is a frequent one. There are several patho- the coronary one, and of the extension and severity of physiologic mechanisms which link both diseases. coronary artery involvement. It is important to empha- Hypertension induces endothelial dysfunction, exacer- sise that complications and mortality of patients suffer- bates the atherosclerotic process and it contributes to ing a myocardial infarction are greater in hypertensive make the atherosclerotic plaque more unstable. Left patients. Treatment should be aimed to achieve optimal ventricular hypertrophy, which is the usual complication values of blood pressure, and all the strategies to treat of hypertension, promotes a decrease of ‘coronary coronary heart disease should be considered on an indi- reserve’ and increases myocardial oxygen demand, vidual basis. both mechanisms contributing to myocardial ischaemia. Journal of Human Hypertension (2002) 16 (Suppl 1), S61– From a clinical point of view hypertensive patients S63. DOI: 10.1038/sj/jhh/1001345 should have a complete evaluation of risk factors for Keywords: hypertension; hypertrophy; coronary heart disease There is a strong and frequent association between arterial hypertension.8 Hypertension is frequently arterial hypertension and coronary heart disease associated to metabolic disorders, such as insulin (CHD). In the PROCAM study, in men between 40 resistance with hyperinsulinaemia and dyslipidae- and 66 years of age, the prevalence of hypertension mia, which are additional risk factors of atheroscler- in patients who had a myocardial infarction was osis.9 14/1000 men in a follow-up of 4 years. -

Hypertension, Cholesterol, and Aspirin with Cost Info
Diabetes & Your Health High Blood Pressure & Diabetes Aspirin & Did you know as many as two out of three adults with Heart Health diabetes have high blood pressure? High blood pressure Studies have shown is a serious problem. It can raise your chances of stroke, that taking a low- heart attack, eye problems, and kidney disease. dose aspirin every Many people do not know they have high blood pressure day can lower the because they do not have any symptoms. That is why it risk for heart attack is often called “the silent killer.” and stroke. The only way to know if you have high blood pressure is Aspirin can help to have it checked. If you have diabetes, you should those who are at high have your blood pressure checked every time you see risk of heart attack, the doctor. People with diabetes should try to keep their such as people who blood pressure lower than 130 over 80. have diabetes or high blood pressure. Cholesterol & Diabetes Aspirin can also help Keeping your cholesterol and other blood fats, called lipids, under control can people with diabetes help you prevent diabetes problems. Cholesterol and blood lipids that are too who have already high can lead to heart attack and stroke. Many people with diabetes have had a heart attack or problems with their cholesterol and other lipid levels. a stroke, or who have heart disease. You will not know that your cholesterol and blood lipids are at dangerous levels unless you have a blood test to have them checked. Everyone with diabetes Taking an aspirin a should have cholesterol and other lipid levels checked at least once per year. -
Vela Proximal Endograft System Phoenix Atherectomy System
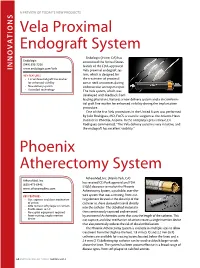
A PREVIEW OF today’s NEW PRODUCTS ONS I Vela Proximal Endograft System Endologix (Irvine, CA) has Endologix announced the United States (949) 595-7200 launch of the FDA-approved INNOVAT www.endologix.com/Vela Vela proximal endograft sys- KEY FEATURES tem, which is designed for • Circumferential graft line marker the treatment of proximal for enhanced visibility aortic neck anatomies during • New delivery system endovascular aneurysm repair. • ActiveSeal technology The Vela system, which was developed with feedback from leading physicians, features a new delivery system and a circumferen- tial graft line marker for enhanced visibility during the implantation procedure. One of the first Vela procedures in the United States was performed by Julio Rodriguez, MD, FACS, a vascular surgeon at the Arizona Heart Institute in Phoenix, Arizona. In the company’s press release, Dr. Rodriguez commented, “The Vela delivery system is very intuitive, and the endograft has excellent visibility.” Phoenix Atherectomy System AtheroMed, Inc. (Menlo Park, CA) AtheroMed, Inc. has received CE Mark approval and FDA (650) 473-6846 510(k) clearance to market the Phoenix www.atheromedinc.com Atherectomy System, a pushable, over-the- KEY FEATURES wire system that uses a rotating, front-cut- • Cut, capture, and clear mechanism ting element located at the distal tip of the of action catheter to shave diseased material directly • Able to treat soft plaque or calcium • Profile down to 5 F into the catheter. The debulked material is • No capital equipment required then continuously captured and removed • Front-cutting, single insertion by an internal Archimedes screw that runs the length of the catheter. -

Guideline-Management-Giant-Cell
Arthritis Care & Research Vol. 73, No. 8, August 2021, pp 1071–1087 DOI 10.1002/acr.24632 © 2021 American College of Rheumatology. This article has been contributed to by US Government employees and their work is in the public domain in the USA. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis Mehrdad Maz,1 Sharon A. Chung,2 Andy Abril,3 Carol A. Langford,4 Mark Gorelik,5 Gordon Guyatt,6 Amy M. Archer,7 Doyt L. Conn,8 Kathy A. Full,9 Peter C. Grayson,10 Maria F. Ibarra,11 Lisa F. Imundo,5 Susan Kim,2 Peter A. Merkel,12 Rennie L. Rhee,12 Philip Seo,13 John H. Stone,14 Sangeeta Sule,15 Robert P. Sundel,16 Omar I. Vitobaldi,17 Ann Warner,18 Kevin Byram,19 Anisha B. Dua,7 Nedaa Husainat,20 Karen E. James,21 Mohamad A. Kalot,22 Yih Chang Lin,23 Jason M. Springer,1 Marat Turgunbaev,24 Alexandra Villa-Forte, 4 Amy S. Turner,24 and Reem A. Mustafa25 Guidelines and recommendations developed and/or endorsed by the American College of Rheumatology (ACR) are intended to provide guidance for particular patterns of practice and not to dictate the care of a particu- lar patient. The ACR considers adherence to the recommendations within this guideline to be voluntary, with the ultimate determination regarding their application to be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are intended to promote beneficial or desirable outcomes but cannot guarantee any specific outcome. -

A 69-Year-Old Woman with Intermittent Claudication and Elevated ESR
756 Self-assessment corner Postgrad Med J: first published as 10.1136/pgmj.74.878.756 on 1 December 1998. Downloaded from A 69-year-old woman with intermittent claudication and elevated ESR M L Amoedo, M P Marco, M D Boquet, S Muray, J M Piulats, M J Panades, J Ramos, E Fernandez A 69-year-old woman was referred to our out-patient clinic because of long-term hypertension and stable chronic renal failure (creatinine 132 ,umol/l), which had been attributed to nephroan- giosclerosis. She presented with a one-year history of anorexia, asthenia and loss of 6 kg ofweight. In addition, she complained of intermittent claudication of the left arm and both legs lasting 2 months. This provoked important functional limitation of the three limbs, and impaired ambula- tion. She did not complain of headache or symptoms suggestive of polymyalgia rheumatica. Her blood pressure was 160/95 mmHg on the right arm and undetectable on the left arm and lower limbs. Both temporal arteries were palpable and not painful. Auscultation of both carotid arteries was normal, without murmurs. Cardiac and pulmonary auscultation were normal. Mur- murs were audible on both subclavian arteries. Neither the humeral nor the radial pulse were detectable on the left upper limb. Murmurs were also audible on both femoral arteries, and nei- ther popliteal nor distal pulses were palpable. Her feet were cold although they had no ischaemic lesions. Funduscopic examination was essentially normal. The most relevant laboratory data were: erythrocyte sedimentation rate (ESR) 120 mm/h, C-reactive protein 4.4 mg/dl (normal range <1.5); antinuclear and antineutrophil cytoplasmic antibodies were negative.