Immunology and Serology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mcb 407-Immunology and Immunochemistry-Lecture Note
MCB 407-IMMUNOLOGY AND IMMUNOCHEMISTRY-LECTURE NOTE DR. D. A. OJO BRIEF HISTORICAL REVIEW OF IMMUNOLOGY The mechanism by which antibody are formed has been debated for years. It was proposed that the specificity of an antibody molecule was determined both by its amino acid sequence but by the molding of the peptide chain around the antigenic determinant. This theory lost favour when it became apparent that antibody-forming cells were devoid of antigen and that antibody specificity was a function of amino acid sequence. At present, the CLONAL (proposed by Burnete) SELECTION THEORY is widely accepted. It holds that an immunologically responsive cell can respond to only one antigen or a closely related group of antigens and that this property is inherent in the cell before the antigen is encountered. According to the clonal selection theory, each individual is endowed with a very large pool of lymphocytes, each of which is capable of responding to a different antigen. When the antigen enters the body, it selects the lymphocyte which has the best “fit” by virtue of a surface receptor. The antigen binds to this antibody-like receptor, and the cell is stimulated to proliferate and form a clone of cells. Thus, selected cells quickly differentiate into plasma cells and secrete antibody which is specific for the antigen which served as the original selecting agent (or a closely related group of antigens). The History of Blood Transfusion Man’s centuries-long desire to perform blood transfusion as a therapeutic procedure forms the cornerstone of the modern science of immunohematology. At present time, the use of whole blood is a well-accepted and commonly employed measure without which many modern surgical procedures could not be carried out. -

"Epitope Mapping: B-Cell Epitopes". In: Encyclopedia of Life Sciences
Epitope Mapping: B-cell Advanced article Epitopes Article Contents . Introduction GE Morris, Wolfson Centre for Inherited Neuromuscular Disease RJAH Orthopaedic Hospital, . What Is a B-cell Epitope? . Epitope Mapping Methods Oswestry, UK and Keele University, Keele, Staffordshire, UK . Applications Immunoglobulin molecules are folded to present a surface structure complementary to doi: 10.1002/9780470015902.a0002624.pub2 a surface feature on the antigen – the epitope is this feature of the antigen. Epitope mapping is the process of locating the antibody-binding site on the antigen, although the term is also applied more broadly to receptor–ligand interactions unrelated to the immune system. Introduction formed of highly convoluted peptide chains, so that resi- dues that lie close together on the protein surface are often Immunoglobulin molecules are folded in a way that as- far apart in the amino acid sequence (Barlow et al., 1986). sembles sequences from the variable regions of both the Consequently, most epitopes on native, globular proteins heavy and light chains into a surface feature (comprised of are conformation-dependent and they disappear if the up to six complementarity-determining regions (CDRs)) protein is denatured or fragmented. Sometimes, by acci- that is complementary in shape to a surface structure on the dent or design, antibodies are produced against linear antigen. These two surface features, the ‘paratope’ on the (sequential) epitopes that survive denaturation, though antibody and the ‘epitope’ on the antigen, may have a cer- such antibodies usually fail to recognize the native protein. tain amount of flexibility to allow an ‘induced fit’ between The simplest way to find out whether an epitope is confor- them. -

C3b Catalog Number: A114 Sizes Available
Name: C3b Catalog Number: A114 Sizes Available: 250 µg/vial Concentration: 1.0 mg/mL (see Certificate of Analysis for actual concentration) Form: Liquid Purity: >90% by SDS-PAGE Buffer: 10 mM sodium phosphate, 145 mM NaCl, pH 7.3 Extinction Coeff. A280 nm = 1.03 at 1.0 mg/mL Molecular Weight: 176,000 Da (2 chains) Preservative: None, 0.22 µm filtered Storage: -70oC or below. Avoid freeze/thaw. Source: Normal human serum (shown by certified tests to be negative for HBsAg and for antibodies to HCV, HIV-1 and HIV-II). Precautions: Use normal precautions for handling human blood products. Origin: Manufactured in the USA. General Description C3b is derived from native C3 upon cleavage and release of C3a. It is prepared by cleavage with the alternative pathway C3 convertase. This is important because only a single bond in C3 is cleaved by the native convertase, while cleavage by other proteases, such as trypsin, results in multiple cleavages at many other sites in the protein. Native human C3b is a glycosylated (~2.8%) polypeptide containing two disulfide-linked chains. C3b is central to the function of all three pathways of complement (Law, S.K.A. and Reid, K.B.M. (1995)). Initiation of each pathway generates proteolytic enzyme complexes (C3 convertases) which are bound to the target surface. These enzymes cleave a peptide bond in C3 releasing the anaphylatoxin C3a and activating C3b. For a brief time (~60 µs) this nascent C3b is capable of reacting with and covalently coupling to hydroxyl groups on the target surface. -
Syllabus for M
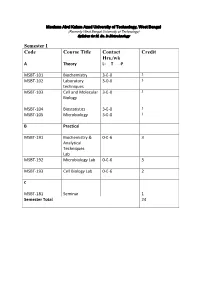
Maulana Abul Kalam Azad University of Technology, West Bengal (Formerly West Bengal University of Technology) Syllabus for M. Sc. In Biotechnology Semester I Code Course Title Contact Credit Hrs./wk A Theory L- T -P MSBT-101 Biochemistry 3-0-0 3 MSBT-102 Laboratory 3-0-0 3 techniques MSBT-103 Cell and Molecular 3-0-0 3 Biology MSBT-104 Biostatistics 3-0-0 3 MSBT-105 Microbiology 3-0-0 3 B Practical MSBT-191 Biochemistry & 0-0-6 3 Analytical Techniques Lab MSBT-192 Microbiology Lab 0-0-6 3 MSBT-193 Cell Biology Lab 0-0-6 2 C MSBT-181 Seminar 1 Semester Total 24 Maulana Abul Kalam Azad University of Technology, West Bengal (Formerly West Bengal University of Technology) Syllabus for M. Sc. In Biotechnology MSBT101: Biochemistry credits 3 Unit 1: Basic chemistry for biologists Formation of chemical bonds, molecular orbital (MO) theory and linear combination of atomic orbitals (LCAO),basics of mass spectrometry, molecules, Avogadro number, molarity, chemical reactions, reaction stoichiometry, rates of reaction, rate constants, order of reactions,kinetic versus thermodynamic controls of a reaction, reaction equilibrium (equilibrium constant); light and matter interactions (optical spectroscopy, fluorescence, bioluminescence, paramagnetism and diamagnetism, photoelectron spectroscopy; chemical bonds (ionic, covalent, Van derWalls forces); electronegativity, polarity; VSEPR theory and molecular geometry, dipole moment, orbital hybridizations; acids, bases and pH - Arrhenious theory, pH, ionic product of water, weak acids and bases, conjugate acid-base pairs, buffers and buffering action etc; chemical thermodynamics - internal energy, heat and temperature, enthalpy (bond enthalpy and reaction enthalpy), entropy, Gibbs free energy of ATP driven reactions, spontaneity versus driven reactions in biology;bond rotations and molecular conformations - Newman projections, conformational analysis of alkanes, alkenes and alkynes; functional groups, optically asymmetric carbon centers, amino acids, proteins, rotational freedoms in polypeptide backbone (Ramachandran plot). -

Blocking Properdin Prevents Complement-Mediated Hemolytic Uremic Syndrome and Systemic Thrombophilia
BASIC RESEARCH www.jasn.org Blocking Properdin Prevents Complement-Mediated Hemolytic Uremic Syndrome and Systemic Thrombophilia Yoshiyasu Ueda,1 Takashi Miwa,1 Damodar Gullipalli,1 Sayaka Sato,1 Daisuke Ito,1 Hangsoo Kim,1 Matthew Palmer,2 and Wen-Chao Song1 Departments of 1Systems Pharmacology and Translational Therapeutics and 2Pathology and Laboratory Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania ABSTRACT Background Properdin (P) is a positive regulator of the alternative pathway of complement activation. Although P inhibition is expected and has been shown to ameliorate the alternative pathway of comple- ment-mediated tissue injury in several disease models, it unexpectedly exacerbated renal injury in a murine model of C3 glomerulopathy. The role of P in atypical hemolytic uremic syndrome (aHUS) is uncertain. Methods We blocked P function by genetic deletion or mAb-mediated inhibition in mice carrying a factor H (FH) point mutation, W1206R (FHR/R), that causes aHUS and systemic thrombophilia with high mortality. Results Pdeficiency completely rescued FHR/R mice from premature death and prevented thrombocyto- penia, hemolytic anemia, and renal disease. It also eliminated macrovessel thrombi that were prevalent in FHR/R mice. All mice that received a function-blocking anti-P mAb for 8 weeks survived the experimental period and appeared grossly healthy. Platelet counts and hemoglobin levels were significantly improved in FHR/R mice after 4 weeks of anti-P mAb treatment. One half of the FHR/R mice treated with an isotype control mAb but none of the anti-P mAb-treated mice developed stroke-related neurologic disease. Anti-P mAb-treated FHR/R mice showed largely normal renal histology, and residual liver thrombi were detected in only three of 15 treated mice. -

Ten Years of Lateral Flow Immunoassay Technique Applications: Trends, Challenges and Future Perspectives
sensors Review Ten Years of Lateral Flow Immunoassay Technique Applications: Trends, Challenges and Future Perspectives Fabio Di Nardo * , Matteo Chiarello , Simone Cavalera , Claudio Baggiani and Laura Anfossi Department of Chemistry, University of Torino, 10125 Torino, Italy; [email protected] (M.C.); [email protected] (S.C.); [email protected] (C.B.); [email protected] (L.A.) * Correspondence: [email protected] Abstract: The Lateral Flow Immunoassay (LFIA) is by far one of the most successful analytical platforms to perform the on-site detection of target substances. LFIA can be considered as a sort of lab-in-a-hand and, together with other point-of-need tests, has represented a paradigm shift from sample-to-lab to lab-to-sample aiming to improve decision making and turnaround time. The features of LFIAs made them a very attractive tool in clinical diagnostic where they can improve patient care by enabling more prompt diagnosis and treatment decisions. The rapidity, simplicity, relative cost-effectiveness, and the possibility to be used by nonskilled personnel contributed to the wide acceptance of LFIAs. As a consequence, from the detection of molecules, organisms, and (bio)markers for clinical purposes, the LFIA application has been rapidly extended to other fields, including food and feed safety, veterinary medicine, environmental control, and many others. This review aims to provide readers with a 10-years overview of applications, outlining the trends for the main application fields and the relative compounded annual growth rates. Moreover, future perspectives and challenges are discussed. Citation: Di Nardo, F.; Chiarello, M.; Cavalera, S.; Baggiani, C.; Anfossi, L. -

Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant
Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease 1 Produced by St. Jude Children’s Research Hospital Departments of Hematology, Patient Education, and Biomedical Communications. Funds were provided by St. Jude Children’s Research Hospital, ALSAC, and a grant from the Plough Foundation. This document is not intended to take the place of the care and attention of your personal physician. Our goal is to promote active participation in your care and treatment by providing information and education. Questions about individual health concerns or specifi c treatment options should be discussed with your physician. For more general information on sickle cell disease, please visit our Web site at www.stjude.org/sicklecell. Copyright © 2009 St. Jude Children’s Research Hospital How did bone marrow (stem cell) transplants begin for children with sickle cell disease? Bone marrow (stem cell) transplants have been used for the treatment and cure of a variety of cancers, immune system diseases, and blood diseases for many years. Doctors in the United States and other countries have developed studies to treat children who have severe sickle cell disease with bone marrow (stem cell) transplants. How does a bone marrow (stem cell) transplant work? 2 In a person with sickle cell disease, the bone marrow produces red blood cells that contain hemoglobin S. This leads to the complications of sickle cell disease. • To prepare for a bone marrow (stem cell) transplant, strong medicines, called chemotherapy, are used to weaken or destroy the patient’s own bone marrow, stem cells, and infection fi ghting system. -

Technical Methods
J Clin Pathol 1987;40:581-588 J Clin Pathol: first published as 10.1136/jcp.40.5.581 on 1 May 1987. Downloaded from 56°C for 30 minutes. Technical methods Complement fixation tests were performed accord- ing to established methods,10 1 except that microtitre plates were used instead of World Health Organisation trays. For maximum sensitivity an ini- Cytomegalovirus (CMV) tial serum dilution of 1/4 was used. The antigen prep- antibody screening in blood aration used was a CMV complement fixation test antigen supplied by either Flow Laboratories Ltd, donors: modification of new latex Irvine, Scotland, or the Central Public Health Labo- ratory, Colindale, England. Guinea pig complements agglutination test compared with were supplied by Wellcome Diagnostics, Dartford, two standard methods England, or Don Whitly Scientific Ltd, Shipley, England. Complement fixation tests were performed A PUCKETT J E DAVIS From the Regional Blood using the following CMV antigen and complement Transfusion Centre, John Radeliffe Hospital, combinations: (1) PHLS CMV antigen + Wellcome Headington, Oxford, England Diagnostics complement, (2) PHLS CMV antigen + Don Whitly complement, and (3) Flow Laboratories CMV antigen + Wellcome Diagnostics complement. Infection with cytomegalovirus (CMV) is common, Immunofluorescence tests were performed and between 50 and 100% of adults may show evi- according to a standard method12 13 using substrate dence of infection.1 The transmission of the virus by slides of CMV infected (Westwood strain) fibroblasts blood transfusion2 and, therefore, the need to screen the Oxford Public Health Laboratory. donations intended for at risk groups such as provided by immunocompromised patients34 and neonates5 -7 iS CMV Scan passive latex agglutination kits were now well established. -

Apheresis Donation This Quick Reference Guide Will Help You Identify the Best Donation for Your Unique Blood Type
Apheresis Donation This quick reference guide will help you identify the best donation for your unique blood type. Donors now have the opportunity to make an apheresis (ay-fur-ee-sis) donation and donate just platelets, red cells, or plasma at blood drives. These individual components are vital for local patients in need. Platelets Control Bleeding Red Cells Deliver Oxygen Plasma transports blood cells & controls bleeding Donation Type Blood Types Requirements Donation Time A+, B+, O+ Over 75% of population has one of these blood types. Platelet Donation: Be healthy, weigh at least 114 lbs 2 hours cancer & surgery patients no aspirin for 48 hours Platelets only last five days after donation so the need is constant. O-, O+, A-, B- Special height, weight, Double Red: O-Negative is the 1 hour and hematocrit requirements. surgery, trauma patients, universal red cell donor. +25 min Please call us or see a staff member accident, & burn victims Only 17% of population has one of these negative blood types Plasma: AB+, AB- Trauma patients, burn Universal Plasma Donors 1 hour Be healthy, weigh at least 114 lbs victims, & patients with +30 min serious illness or injuries Only 4% of population How Apheresis works: Blood is drawn from the donor’s arm and the components are separated. Only the components being donated are collected while the remaining components are safely returned to the donor How to Schedule an Appointment: Please call 800-398-7888 or visit schedule.bloodworksnw.org. Walk-ins are also welcome at some blood drives, so be sure to ask our staff when you stop in. -

Eosinophil Cytolysis and Release of Cell-Free Granules
CORRESPONDENCE LINK TO ORIGINAL ARTICLE LINK TO INITIAL CORRESPONDENCE to determine what conditions in vivo favour piecemeal degranulation and what condi- Eosinophil cytolysis and release of tions promote cytolysis (with or without ‘net’ formation) and release of intact granules. cell-free granules There are several strong recent reviews cover- ing mechanisms of degranulation, including 10 Helene F. Rosenberg and Paul S. Foster those written by Neves and Weller , and Lacy and Moqbel11, for those seeking greater insight into this important and evolving field. We are grateful for an excellent oppor- The results of eosinophil cytolysis — Helene F. Rosenberg is in the Inflammation tunity to expand on our recent Review specifically, the release of intact granules — Immunobiology Section, National Institute of Allergy (Eosinophils: changing perspectives in are not new findings. There have been many and Infectious Diseases, National Institutes of Health, health and disease. Nature Rev. Immunol. reports of free granules in tissues found in Bethesda, Maryland 20892, USA. 13, 9–22 (2013))1 that has been provided by conjunction with eosinophil-associated dis- Paul S. Foster is at the Priority Research Center the correspondence from Carl Persson and eases, including allergic rhinitis, bronchial for Asthma and Respiratory Diseases, Hunter Medical Research Institute and School of Lena Uller (Primary lysis of eosinophils asthma, atopic dermatitis, urticaria and Biomedical Sciences and Pharmacy, Faculty of Health, 7 as a major mode of activation of eosino- eosinophilic esophagitis . However, it was University of Newcastle, Newcastle, New South Wales, phils in human diseased tissues. Nature not clear what role these granules had, if any, 2300, Australia. -
Adaptive Immune Systems
Immunology 101 (for the Non-Immunologist) Abhinav Deol, MD Assistant Professor of Oncology Wayne State University/ Karmanos Cancer Institute, Detroit MI Presentation originally prepared and presented by Stephen Shiao MD, PhD Department of Radiation Oncology Cedars-Sinai Medical Center Disclosures Bristol-Myers Squibb – Contracted Research What is the immune system? A network of proteins, cells, tissues and organs all coordinated for one purpose: to defend one organism from another It is an infinitely adaptable system to combat the complex and endless variety of pathogens it must address Outline Structure of the immune system Anatomy of an immune response Role of the immune system in disease: infection, cancer and autoimmunity Organs of the Immune System Major organs of the immune system 1. Bone marrow – production of immune cells 2. Thymus – education of immune cells 3. Lymph Nodes – where an immune response is produced 4. Spleen – dual role for immune responses (especially antibody production) and cell recycling Origins of the Immune System B-Cell B-Cell Self-Renewing Common Progenitor Natural Killer Lymphoid Cell Progenitor Thymic T-Cell Selection Hematopoetic T-Cell Stem Cell Progenitor Dendritic Cell Myeloid Progenitor Granulocyte/M Macrophage onocyte Progenitor The Immune Response: The Art of War “Know your enemy and know yourself and you can fight a hundred battles without disaster.” -Sun Tzu, The Art of War Immunity: Two Systems and Their Key Players Adaptive Immunity Innate Immunity Dendritic cells (DC) B cells Phagocytes (Macrophages, Neutrophils) Natural Killer (NK) Cells T cells Dendritic Cells: “Commanders-in-Chief” • Function: Serve as the gateway between the innate and adaptive immune systems. -

Serotyping of Bdellovibrios by Agglutination and Indirect Immunofluorescence
INTERNATIONAL JOURNAL OF SYSTEMATICBACT~RIOLOGY. Oct. 1983, p. 816-821 Vol. 33, No. 4 0020-7713/83/040816-06$02.00/0 Copyright 0 1983, Internationnl Union of Microbiologicdl Societie\ Serotyping of Bdellovibrios by Agglutination and Indirect Immunofluorescence M. E. SCHELLING’* AND S. F. CONTI’ Department Biology, Texus A &M Unitwsit?, College Station, Texus 77843‘ und University of Mussa ch us et t s , A rn ii erst, Muss N c h iiset t J 0 1 002’ A comparative serological study was undertaken to clarify the uncertain interrelationships among various bdellovibrios. A total of 17 predacious (host- dependent) strains and 12 nonpredacious strains were serotyped. Strains were grouped into serotypes on the basis of positive agglutination and strongly positive fluorescence cross-reactions. The results of division of the strains into serogroups by these two methods were identical. Bdellovihrio starrii strain A3.12 and Bdellovibrio stolpii strain UKi2 were found to be antigenically distinct from each other and from the group of strains comprising Bdellovihrio hacteriovorus; the latter was found to be an antigenically heterogeneous group consisting of at least nine serogroups. All nonpredacious strains were found to be related antigenically to their obligately predacious counterparts. An antigen(s) common to all of the Bdellovibrio strains examined was exhibited as weakly positive fluorescence. Selected strains of Bdellovihrio were studied by Ouchterlony immunodiffusion, which confirmed the serogrouping results and provided a technically simple method of serotyping. Further immunochemical characterization of the strains of Bdellovihrio in conjunction with increased knowledge of other differences among strains will likely result in the formation of additional species of Bdellovihrio.