Keratoprosthesis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pediatric Keratoprosthesis
Pediatric Keratoprosthesis James V. Aquavella, MD,1,2 Matthew D. Gearinger, MD,1,2 Esen K. Akpek, MD,3 Gregory J. McCormick, MD2 Objective: To describe the authors’ experience using keratoprosthesis to treat pediatric corneal opacity. Design: Nonrandomized, consecutive, retrospective interventional series. Participants: Twenty-two eyes of 17 children with opaque corneas as a result of primary congenital disease and or previous failed keratoplasty. Methods: A retrospective review of pediatric patients with a history of corneal opacification treated with keratoprosthesis surgery. Main Outcome Measures: Intraocular pressure, inflammation, clarity of the visual axis, visual acuity, refraction, complications, and retention of the prosthesis. Results: Twenty-two eyes of 17 patients 1.5 to 136 months of age underwent 23 keratoprosthesis proce- dures. The follow-up period was 220 patient months (range, 1–37 months; mean, 9.7 months). In both cases implanted with the AlphaCor (Argus Biomedical Pty. Ltd., Perth, Australia), the keratoprosthesis was not retained. In one instance, the prosthesis sustained traumatic dislocation and was replaced with a cadaver cornea. In the second instance, the intralamellar implant began to extrude and was replaced with a Boston keratoprosthesis. In all 21 Boston cases, the prosthesis was retained without dislocation or extrusion. The visual axis remained clear in 100% of cases, although retroprosthetic membranes were removed in 5 eyes. Reoperation was necessitated for management of concurrent glaucoma (n ϭ 3) or retinopathy (n ϭ 2). There were no instances of surface infection or endophthalmitis. In 7 instances where patient age was 4 years or more, visual acuity ranged from counting fingers to 20/30. -

Glaucoma Management After Corneal Transplantation Surgeries
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Curr Opin Manuscript Author Ophthalmol. Manuscript Author manuscript; available in PMC 2017 September 05. Published in final edited form as: Curr Opin Ophthalmol. 2016 March ; 27(2): 132–139. doi:10.1097/ICU.0000000000000237. Glaucoma management after corneal transplantation surgeries Helen L. Kornmann and Steven J. Gedde Bascom Palmer Eye Institute, University of Miami, Miller School of Medicine, Miami, Florida, USA Abstract Purpose of review—Intraocular pressure (IOP) elevation and glaucoma progression following corneal transplantation, specifically, penetrating keratoplasty, Descemet’s stripping endothelial keratoplasty, and Boston keratoprosthesis, are well described causes of ocular morbidity. Depending on the procedure performed, the incidence of glaucoma is highly variable. Several etiologic factors have been identified, the most common being synechial angle closure and corticosteroid-induced IOP elevation. The purpose of this review is to describe the various treatment strategies for glaucoma following corneal transplantation. Recent findings—Medications and laser treatments are usually first-line therapies for postoperative IOP elevation. Surgical intervention, including filtering surgery and glaucoma drainage devices, may be necessary to control IOP and prevent progressive glaucomatous damage. Summary—Glaucoma is a common complication of corneal transplantation, and the degree of aggressiveness is often related to the indication for corneal surgery. -

Keratoprosthesis
Corporate Medical Policy Keratoprosthesis File Name: kera toprosthesis Origination: 11/1989 Last CAP Review: 6/2021 Next CAP Review: 6/2022 Last Review: 6/2021 Description of Procedure or Service A keratoprosthesis, consisting of a central optic held in a cylindrical frame, is a n a rtificial cornea that is intended to restore vision to patients with severe bilateral corneal disease (such as prior failed corneal transplants, chemical injuries, or certain immunological conditions) for whom a corneal transplant is not an option. The keratoprosthesis replaces the cornea that has been removed and is held in place by the surrounding tissue. Various biologic materials are being investigated to improve integration of the prosthetic into the eye. Background The cornea, a clear, dome-shaped membrane that covers the front of the eye, is a key refractive element of the eye. Layers of the cornea consist of the epithelium (outermost layer); Bowman’s layer; the stroma, which comprises approximately 90% of the cornea; Descemet’s membrane; and the endothelium. Treatment The established surgical treatment for corneal disease is penetrating keratoplasty (PK), which involves making a large central opening through the cornea and then filling the opening with full- thickness donor cornea. In certain conditions such as Stevens-Johnson syndrome, ocular cicatricial pemphigoid, chemical injury, or prior failed corneal transplant, survival of transplanted cornea is poor. The keratoprosthesis has been developed to restore vision in patients for whom a corneal transplant is not an option. Kera toprosthetic devices consist of a central optic held in a cylindrical fra me. The keratoprosthesis replaces the section of cornea that has been removed, and, along with being held in place by the surrounding tissue, may be covered by a membrane to further a nchor the prosthesis. -

221 Keratoprosthesis
Medical Policy Keratoprosthesis Table of Contents • Policy: Commercial • Coding Information • Information Pertaining to All Policies • Policy: Medicare • Description • References • Authorization Information • Policy History Policy Number: 221 BCBSA Reference Number: 9.03.01 NCD/LCD: N/A Related Policies • Endothelial Keratoplasty, #180 • Implantation of Intrastromal Corneal Ring Segments, #235 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Medicare HMO BlueSM and Medicare PPO BlueSM Members The Boston (Dohlman-Doane) Keratoprosthesis (Boston KPro) may be considered MEDICALLY NECESSARY for the treatment of severe corneal opacification under the following conditions: • The cornea is severely opaque and vascularized AND • Best-corrected visual acuity is ≤ 20/400 or less in the affected eye and 20/40 or less in the contralateral eye AND • No end-stage glaucoma or retinal detachment is present AND • The patient has one of the following indications: o History of 1 or more corneal transplant graft failures o Stevens-Johnson syndrome o Ocular cicatricial pemphigoid o Autoimmune conditions with rare ocular involvement o Ocular chemical burns o An ocular condition unlikely to respond favorably to primary corneal transplant surgery (eg, limbal stem cell compromise or postherpetic anesthesia). Note: Patients should be expected to be able to be compliant with postoperative care. A permanent keratoprosthesis for all other conditions is considered INVESTIGATIONAL. All other types of permanent keratoprostheses are considered INVESTIGATIONAL. 1 Prior Authorization Information Inpatient • For services described in this policy, precertification/preauthorization IS REQUIRED for all products if the procedure is performed inpatient. Outpatient • For services described in this policy, see below for products where prior authorization might be required if the procedure is performed outpatient. -

Keratoprosthesis Protocol
Keratoprosthesis Protocol (90301) Medical Benefit Effective Date: 10/01/16 Next Review Date: 07/22 Preauthorization No Review Dates: 05/07, 07/08, 05/09, 01/10, 01/11, 01/12, 01/13, 09/13, 07/14, 07/15, 07/16, 07/17, 07/18, 07/19, 07/20, 07/21 Preauthorization is not required. The following protocol contains medical necessity criteria that apply for this service. The criteria are also applicable to services provided in the local Medicare Advantage operating area for those members, unless separate Medicare Advantage criteria are indicated. If the criteria are not met, reimbursement will be denied and the patient cannot be billed. Please note that payment for covered services is subject to eligibility and the limitations noted in the patient’s contract at the time the services are rendered. RELATED PROTOCOLS Endothelial Keratoplasty Implantation of Intrastromal Corneal Ring Segments Populations Interventions Comparators Outcomes Individuals: Interventions of interest Comparators of interest Relevant outcomes include: • With corneal blindness are: are: • Change in disease status who have failed or are not • Boston • Penetrating • Morbid events candidates for corneal Keratoprosthesis keratoplasty • Quality of life transplantation • Treatment-related morbidity Individuals: Interventions of interest Comparators of interest Relevant outcomes include: • With corneal blindness are: are: • Change in disease status who have failed or are not • Keratoprosthesis using • Penetrating • Morbid events candidates for corneal the AlphaCor device keratoplasty -

The Osteo-Odonto-Keratoprosthesis (OOKP)
Seminars in Ophthalmology, 20:113–128, 2005 Copyright c Taylor & Francis Inc. ISSN: 0882-0538 DOI: 10.1080/08820530590931386 The Osteo-Odonto-Keratoprosthesis (OOKP) Christopher Liu Sussex Eye Hospital, Brighton, ABSTRACT The osteo-odonto-keratoprosthesis (OOKP), although described England, Aston University, Birmingham, England, and Kinki over 40 years ago, remains the keratoprosthesis of choice for end-stage corneal University, Osaka, Japan blindness not amenable to penetrating keratoplasty. It is particularly resilient Bobby Paul to a hostile environment such as the dry keratinized eye resulting from se- Sussex Eye Hospital, Brighton, England vere Stevens-Johnson syndrome, ocular cicatricial pemphigoid, trachoma, and Radhika Tandon chemical injury. Its rigid optical cylinder gives excellent image resolution and Sussex Eye Hospital, Brighton, England and All India Institute of Medical quality. The desirable properties of the theoretical ideal keratoprosthesis is de- Sciences, New Delhi, India scribed. The indications, contraindications, and patient assessment (eye, tooth, Edward Lee, Ken Fong, and buccal mucosa, psychology) for OOKP surgery are described. The surgical and Ioannis Mavrikakis anaesthetic techniques are described. Follow-up is life-long in order to detect Sussex Eye Hospital, Brighton, England and treat complications, which include oral, oculoplastic, glaucoma, vitreo- Jim Herold and Simon Thorp Royal Sussex County Hospital, retinal complications and extrusion of the device. Resorption of the osteo- Brighton, England odonto-lamina is responsible for extrusion, and this is more pronounced in Paul Brittain tooth allografts. Regular imaging with spiral-CT or electron beam tomography Sussex Eye Hospital, Brighton, England can help detect bone and dentine loss. The optical cylinder design is discussed. Ian Francis Preliminary work towards the development of a synthetic OOKP analogue Royal Sussex County Hospital, Brighton, England is described. -

BOSTON Kpro News Antimicrobial Prophylaxis for Life: FALL 2011 | NUMBER 8 As Important As Ever
BOSTON KPro news Antimicrobial prophylaxis for life: FALL 2011 | NUMBER 8 as important as ever However, it has become increasingly clear that very small amounts of antibiotics applied topically every day to the operated eye can be very effective in preventing bacterial infections. While this seems counterintuitive, our experience gained from thousands of KPro cases indicates that daily application of a light prophylaxis can be effective for many years without complications; it is also clear that, without any prophylactic antibiotics, the risk of infection is still very high. On the other hand, an excess of antibiotics can make the eye susceptible to fungal infections. Therefore, choosing the right antibiotic in the right concentration is very important for the long-term success of keratoprostheses. While many surgeons recommend ata drawn from thousands the most common culprit. Infections different regimens, the procedures of keratoprosthesis cases is rarely occur during the first few months we follow in Boston have been very showing that the judicious use postoperatively, but may surface D effective and are summarized here of daily antibiotics can successfully later, and are often related to obvious (Infectious Disease specialists Marlene lower postoperative infection rates. tissue melt and leak. Autoimmune Durand, MD and Irmgard Behlau, MD In the past, postoperative bacterial diseases (Stevens-Johnson syndrome, have been consulted): endophthalmitis frequently occurred ocular pemphigoid, graft vs. host after any type of keratoprosthesis, disease, atopy, etc.) have been the most 1. For the standard patient receiving a which contributed to the poor vulnerable to infection. The events have, Boston Keratoprosthesis Type I after reputation of the procedure. -

Osteo-Odonto- Patients with Corneal Blind -Keratoprosthesis (OOKP)
Osteo-Odonto-Keratoprosthesis (OOKP): A review ISSN: 2394-0026 (P) ISSN: 2394-0034 (O) Review Article Osteo-Odonto -Keratoprosthesis (OOKP) for patients with corneal blindness: A review Irfan Ashraf Baba 1, Chitroda Parita K 2, Kothari Shreyans P 3, Singh Ashutosh 4, Aasim Farooq Shah 5* 1Registrar, Dept. of Oral Medicine & Radiology , Govt. Dental College & Hospital, Srinagar , Jammu and Kashmir, India 2Reader, Dept of Oral Medicine & Radiology , Al-Badar Rural Dental College & Hospital , Gulbarga, Karnataka, India 3Assistant Professor, Dept. of Op hthalmology, KBN Medical College & Hospital, Gulbarga , Karnataka, India 4PG Student, Dept. of Oral Medicine & Radiology , Al-Badar Rural Dental College & Hospital , Gulbarga, Karnataka, India 5Department of Public Health Dentistry , Government Dental College and Hospital , Shrein Bagh, Srinagar, Jammu and Kashmir, India *Corresponding author email: [email protected] How to cite this article: Irfan Ashraf Baba, Chitroda Parita K, Kothari Shreyans P, Singh Ashutosh, Aasim Farooq Shah. Osteo-Odonto -Keratoprosthesis (OOKP) for patients with corneal blindness: A review. IAIM, 2015; 2(6): 240-248. Available online at www.iaimjournal.com Received on: 01-06-2015 Accepted on: 06-06-2015 Abstract Anatomically, the cornea is the outermost layer of the eye and is primarily responsible for light refraction which allows for central and peripheral vision. Corneal diseases are among the major causes of global blindness, secondary to cataracts. This paper intends to review Osteo -Odonto Keratoprosthesis (OOKP), which is a two stage procedure whereby dental and buccal tissue is auto - transplanted into eye to serve as a synthetic cornea. Our purpose is to inform readers about the relevant anatomy, two-stage pr ocedure, surgical inter-professionalism, indications, contraindications, complications, long -term functional and anatomical results and patient outcomes of OOKP. -

Boston Keratoprosthesis Update
Boston Keratoprosthesis Update Newsletter VI: 2009 Editor: Rhonda Walcott-Harris http://www.meei.harvard.edu/shared/ophtho/cornea2.php Intraocular pressure sensors in KPro Samir Melki, MD, PhD, Miguel Lopez, MD and Claes Dohlman, MD, PhD Implantable sensor Telemetry pressure reader Postoperative glaucoma is still a considerable problem in KPro-implanted eyes, especially in those after chemical burns. Of patients accepted for KPro surgery in Boston, more than two- thirds had glaucoma diagnosed already preoperatively and some were aggravated by the subsequent surgery. What makes the problem more challenging is the difficulty of measuring the intraocular pressure accurately in an eye with a KPro. In the Boston KPro the stiff back plate prevents measurements based on indentation of the cornea, even in its periphery. Scleral tonometry or the use of any device acting through the lids has in our hands been highly unreliable due to often distorted or scarred tissue structures. For all its vagaries, finger palpation over the upper lid with the patient looking down has arguably been so far the best approach to gross estimation of the IOP. There is unquestionably a great need for more precise methodology to assess IOP in KPro eyes. An intraocular pressure transducer, that can be monitored from the outside has for a long time been a desirable goal for glaucoma researchers, and animal experiments since 1992 have showed some promise. Miniaturization and long-term stability have been problems, however. More recently a very small (0.5 mm diameter) pressure transducer was made available, allowing implantation in animals and pressures to be read optically through the KPro by laser interferometry (FISO, Inc., Ottawa, Canada). -
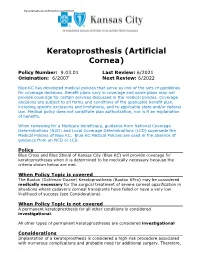
Keratoprosthesis (Artificial Cornea) 9.03.01
Keratoprosthesis (Artificial Cornea) 9.03.01 Keratoprosthesis (Artificial Cornea) Policy Number: 9.03.01 Last Review: 6/2021 Origination: 6/2007 Next Review: 6/2022 Blue KC has developed medical policies that serve as one of the sets of guidelines for coverage decisions. Benefit plans vary in coverage and some plans may not provide coverage for certain services discussed in the medical policies. Coverage decisions are subject to all terms and conditions of the applicable benefit plan, including specific exclusions and limitations, and to applicable state and/or federal law. Medical policy does not constitute plan authorization, nor is it an explanation of benefits. When reviewing for a Medicare beneficiary, guidance from National Coverage Determinations (NCD) and Local Coverage Determinations (LCD) supersede the Medical Policies of Blue KC. Blue KC Medical Policies are used in the absence of guidance from an NCD or LCD. Policy Blue Cross and Blue Shield of Kansas City (Blue KC) will provide coverage for keratoprostheses when it is determined to be medically necessary because the criteria shown below are met. When Policy Topic is covered The Boston (Dohlman-Doane) Keratoprosthesis (Boston KPro) may be considered medically necessary for the surgical treatment of severe corneal opacification in situations where cadaveric corneal transplants have failed or have a very low likelihood of success (see Considerations). When Policy Topic is not covered A permanent keratoprosthesis for all other conditions is considered investigational. All other types of permanent keratoprostheses are considered investigational Considerations Implantation of a keratoprosthesis is considered a high-risk procedure associated with numerous complications and probable need for additional surgery. -

Boston Keratoprosthesis Type I
Facultad de Medicina Departamento de Cirugía BOSTON KERATOPROSTHESIS TYPE I: INDICATIONS, LONG TERM RESULTS AND COMPLICATIONS Tesis por compendio de publicaciones para optar al grado de Doctor en Medicina y Cirugía por María Fideliz De la Paz Dalisay Directores: Dr. Ralph Michael Dr. Rafael I. Barraquer Compte Tutor: Prof. Dr. José García Arumí Barcelona 2015 2 For my husband Juan and my daughter Francesca, my inspiration to bring out the best in me. For my parents, Johnny and Flor, for teaching me to values of service, humility and faith. For Professor Joaquín Barraquer, to whom I owe my professional growth. For my patients, for their trust and friendship. 3 4 ACKNOWLEDGEMENTS 5 6 For my thesis director Dr. Ralph Michael, for all these years of working together harmoniously in analyzing our large database on keratoprostheses, and for personally leading me on this journey. For Dr. Rafael Barraquer and Prof. Dr. José García Arumí, my thesis directors, for their patience and guidance. For Dr. José Temprano, for fascinating me with his surgical skills and his legacy of the Tibial bone keratorprothesis; he is an inspiration for me to always give a ray of hope to those condemned to corneal blindness. For Valeria Rezende, Gerardo Muñoz, Orang Seyeddain, the manuscripts would not have been possible without their invaluable input and ideas. For Dr. Rafael Barraquer, Dr. Juan Alvarez de Toledo, from Barcelona, for Dr. Josef Stoiber and Prof. Günther Grabner, from Salzburg, for being pioneers in Boston KPro surgery, without your skills, the patients would not have benefitted from keratoprosthesis surgery. For my co-authors, here and abroad, our teamwork and constant communication are key to successfully publishing the keratoprosthesis manuscripts. -

Awarding the Honorary Degree of DOCTOR HONORIS CAUSA to Professor TRAIAN V
Politehnica University of Timisoara Awarding the Honorary Degree of DOCTOR HONORIS CAUSA to Prof. dr. ing. Traian V. CHIRILĂ Timișoara The 1st of October 2015 Universitatea Politehnica Timișoara Decernarea Titlului Academic de DOCTOR HONORIS CAUSA domnului Profesor dr. ing. TRAIAN V. CHIRILĂ Timișoara 1 Octombrie 2015 3 Professor Traian V. CHIRILĂ, PhD Cuprins Contents Laudatio adresat domnului Prof. dr. ing. Traian V. pag. 7 Laudatio addressed to Prof. Traian V. CHIRILĂ, PhD CHIRILĂ din partea Senatului Universității Politehnica by the Senate of Politehnica University of Timisoara Timișoara Experience in Education and Research of Experiența în Educație și Cercetare a domnului pag. 15 Professor Traian V. CHIRILA Profesor dr. ing. Traian V. CHIRILĂ Curriculum Vitae Curriculum Vitae pag. 19 Complete list of publications Lista completă a publicațiilor pag. 33 Supervised PhD Theses Teze de doctorat conduse pag. 71 Dissertation Disertație pag. 75 Members of DHC Commission Membrii Comisie de Specialitate pag. 99 Doctor Honoris Causa Diploma Diplomă Doctor Honoris Causa (copy) pag. 103 (copie) 5 Laudatio adresat domnului Prof. dr. ing. Traian V. CHIRILĂ din partea Senatului Universităţii Politehnica Timişoara addressed to Professor Traian V. CHIRILĂ, PhD by the Senate of Politehnica University Timisoara Laudatio Laudatio Distinşi oaspeţi şi colegi, Distinguished guests and colleagues, Onorată asistenţă, Honourable audience, Doamnelor şi domnilor, Ladies and Gentlemen, R O EN Senatul Universității Politehnica Timișoara s-a reunit astăzi în ședință festivă pentru a acorda titlul academic de The Senate of Politehnica University of Timisoara has gathered today in a ceremonial meeting to confer the academic title DOCTOR HONORIS CAUSA domnului Profesor Dr. Ing. TRAIAN V.