WHO/EORTC Classification of Cutaneous Lymphomas 2005: Histological and Molecular Aspects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primary Spinal Intramedullary Lymphoma: a Case Report and Review of the Litera- Ture
Central JSM Neurosurgery and Spine Case Report *Corresponding author Feyza Karagoz Guzey, Topkapi Mahallesi, Kahalbagi Sokak 46/2 Fatih Istanbul, Turkey, 34093, Tel: Primary Spinal Intramedullary 905326334032; Email: Submitted: 28 November 2014 Lymphoma: A Case Report and Accepted: 05 January 2015 Published: 08 January 2015 Copyright Review of the Literature © 2015 Guzey et al. Feyza Karagoz Guzey1*, Yucel Hıtay1, Cihan Isler1, Abdurrahim OPEN ACCESS Tas1, Ozgur Aktas1, Azmi Tufan1, Mustafa Vatansever1 and Aslı Keywords 2 Kahraman Akkalp • Central nervous system lymphoma 1Department of Neurosurgery, Bagcilar Research and Training Hospital, Turkey • Lymphoma 2Department of Neurosurgery and Pathology, Bagcilar Research and Training Hospital, • Nonhodgkin lymphoma Turkey • Spinal intramedullary lymphoma • Spinal intramedullary tumor Abstract Background: Primary spinal intramedullary lymphoma is a very rare lesion. It has not specific laboratory or radiologic findings. Therefore false and late diagnosis is frequent. Case Report and Literature Review: A 55 year-old lady with multifocal primary spinal intramedullary B-cell non-Hodgkin’s lymphoma was reported. Review of literature yielded 45 cases with primary spinal intramedullary lymphoma and clinical and radiological characteristics of these 46 cases were evaluated. Results: Male/female ratio was 24/22. Median age of the patients was 51.5 years for all cases except a series consisting 14 cases to be reported in an article in which detailed data case by case was not given. Median age of those 14 cases was 62.5. Most of the cases were localized in the cervical and then thoracic segments. Multifocal spinal tumors were found in 12 patients. Most of the patients were admitted with rapidly progressing myelopathy symptoms and signs. -

Diffuse Large B-Cell Lymphoma of the Central Nervous System
Open Journal of Pathology, 2012, 2, 133-139 1 Published Online October 2012 (http://www.SciRP.org/journal/ojpathology) http://dx.doi.org/10.4236/ojpathology.2012.24024 Diffuse Large B-Cell Lymphoma of the Central Nervous System. Immunophenotype, Clinicopathological Features and Differential Diagnosis Mónica Belinda Romero-Guadarrama1*, María Esther Gutiérrez Díaz-Ceballos1, Fiacro Jiménez-Ponce2, Samantha Thingen-Velarde3 1Unit Pathology Hospital General de México, Medicine School, Autonomous University of Mexico, Mexico City, Mexico; 2Neurosur- gery Unit Hospital General de México, Mexico City, Mexico; 3Hemathology Service, Hospital General de México, Mexico City, Mexico. Email: *[email protected] Received June 14th, 2012; revised July 12th, 2012; accepted July 23rd, 2012 ABSTRACT Background: Diffuse large B-cell lymphomas of the central nervous system (DLBCL CNS) represent less than 1% of all lymphomas and between 2% and 3% of all cerebral tumors. They occur in adults of 60 years of age or more. The objective of this work is to describe the clinical-pathological characteristics, the immunophenotype and the differential diagnosis. Clinical Case: From the files of the surgical pathology unit we found four cases of primary diffuse large B cell lymphoma of the central nervous system in a 6-year period. Three corresponded to women over 47 years of age and the other to a 42-year-old man. The time of evolution was between 2 and 4 months. The symptoms were headache, blurred vision, hemiparesis, and seizures. Localization was in the pineal region, the frontal, parietal regions, and the right thalamus. Morphologically, large lymphoid cells with a diffuse growth pattern and necrosis were observed. -
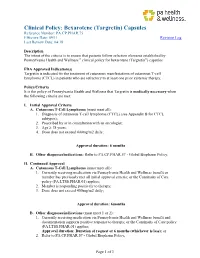
Bexarotene (Targretin) Capsules Reference Number: PA.CP.PHAR.75 Effective Date: 09/11 Revision Log Last Review Date: 04/18
Clinical Policy: Bexarotene (Targretin) Capsules Reference Number: PA.CP.PHAR.75 Effective Date: 09/11 Revision Log Last Review Date: 04/18 Description The intent of the criteria is to ensure that patients follow selection elements established by Pennsylvania Health and Wellness ® clinical policy for bexarotene (Targretin®) capsules FDA Approved Indication(s) Targretin is indicated for the treatment of cutaneous manifestations of cutaneous T-cell lymphoma (CTCL) in patients who are refractory to at least one prior systemic therapy. Policy/Criteria It is the policy of Pennsylvania Health and Wellness that Targretin is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Cutaneous T-Cell Lymphoma (must meet all): 1. Diagnosis of cutaneous T-cell lymphoma (CTCL) (see Appendix B for CTCL subtypes); 2. Prescribed by or in consultation with an oncologist; 3. Age ≥ 18 years; 4. Dose does not exceed 400mg/m2 daily; Approval duration: 6 months B. Other diagnoses/indications: Refer to PA.CP.PHAR.57 - Global Biopharm Policy. II. Continued Approval A. Cutaneous T-Cell Lymphoma (must meet all): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit or member has previously met all initial approval criteria; or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; 2. Member is responding positively to therapy; 3. Dose does not exceed 400mg/m2 daily; Approval duration: 6months B. Other diagnoses/indications (must meet 1 or 2): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit and documentation supports positive response to therapy; or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; Approval duration: Duration of request or 6 months (whichever is less); or 2. -

Intravascular Lymphoma
540 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2003.033662 on 16 March 2005. Downloaded from PAPER Intravascular lymphoma: magnetic resonance imaging correlates of disease dynamics within the central nervous system J M Baehring, C Henchcliffe, C J Ledezma, R Fulbright, F H Hochberg ............................................................................................................................... J Neurol Neurosurg Psychiatry 2005;76:540–544. doi: 10.1136/jnnp.2003.033662 Background: Intravascular lymphoma (IVL) is a rare non-Hodgkin’s lymphoma with relative predilection for the central nervous system. In the absence of extraneural manifestations, the disease is not recognised until autopsy in the majority of cases underlining the need for new clinical markers. Methods: This is a retrospective series of five patients with IVL seen at a single institution over three years. An advanced magnetic resonance imaging (MRI) protocol was performed at various time points prior to diagnosis and during treatment. See end of article for authors’ affiliations Results: MRI revealed multiple lesions scattered throughout the cerebral hemispheres; the brainstem, ....................... cerebellum, and spinal cord were less frequently involved. On initial presentation, hyperintense lesions were seen on diffusion weighted images suggestive of ischaemia in three of four patients in whom the Correspondence to: F H Hochberg, images were obtained at that time point. In four patients lesions were also identifiable as hyperintense Massachusetts General areas on fluid attenuated inversion recovery (FLAIR) sequences. Initial contrast enhancement was Hospital, Brain Tumor encountered in three cases. Diffusion weighted imaging lesions either vanished or followed the typical Center, Cox 315, Boston, MA 02114, USA; pattern of an ischaemic small vessel stroke with evolution of abnormal FLAIR signal followed by [email protected] enhancement with gadolinium in the subacute stage and tissue loss in the chronic stage. -

Message from the President
DermNewsletter of the American OsteopathicLine College of Dermatology Spring 2016 Vol. 32, No. 1 Message from the President Greetings from Houston, Texas - again! As President of the AOCD, I welcome you to another edition of DermLine. As I think about our recent past and the dramatic changes afoot, I recall Suzanne Sirota Rozenberg, DO, FAOCD, Past President of AOCD, commenting in the Spring 2014 edition of DermLine about the coming AOA/ACGME merger. As I stated previously, “Today, at this moment, we are living in yesterday’s future.” Our future has arrived. Because the AOA, along with the Accreditation Council for Graduate Medical Education and the American Association of Colleges of Osteopathic Medicine, have agreed to a single accreditation system for graduate medical education programs in the United States, our graduates of osteopathic institutions, along with graduates of allopathic medical schools will complete their residency and/or fellowship education in ACGME-accredited programs and demonstrate achievement of common milestones and competencies side-by-side. I hope you realize the power in the previous statement. Trained together, osteopathic and allopathic graduates will no longer be divided. Perhaps the most exciting news to share is the AAD vote that just passed last month. This has been a battle we have been fighting for generations. The vote suffered defeat in 2004 and 2010. On both occasions, a majority of the membership voted in favor, but the required two-thirds majority required to approve a change to the bylaws fell short. I was told I would never see this vote go through in my lifetime. -

Small Cell Variant of Intravascular Large B-Cell Lymphoma: Highlighting a Potentially Fatal and Easily Missed Diagnosis
Small Cell Variant of Intravascular Large B-Cell Lymphoma: Highlighting a Potentially Fatal and Easily Missed Diagnosis The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Rahmani, Mahboubeh, Stephanie Halene, and Mina L. Xu. 2018. “Small Cell Variant of Intravascular Large B-Cell Lymphoma: Highlighting a Potentially Fatal and Easily Missed Diagnosis.” BioMed Research International 2018 (1): 9413015. doi:10.1155/2018/9413015. http://dx.doi.org/10.1155/2018/9413015. Published Version doi:10.1155/2018/9413015 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:37160263 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Hindawi BioMed Research International Volume 2018, Article ID 9413015, 6 pages https://doi.org/10.1155/2018/9413015 Research Article Small Cell Variant of Intravascular Large B-Cell Lymphoma: Highlighting a Potentially Fatal and Easily Missed Diagnosis Mahboubeh Rahmani ,1 Stephanie Halene,2 and Mina L. Xu3 1 Department of Pathology, Harvard Medical School, Boston, MA, USA 2Department of Internal Medicine, Hematology Division, Yale University School of Medicine, New Haven, CT, USA 3Department of Pathology and Laboratory Medicine, Yale University School of Medicine, New Haven, CT, USA Correspondence should be addressed to Mahboubeh Rahmani; [email protected] Received 26 November 2017; Revised 23 January 2018; Accepted 4 March 2018; Published 3 April 2018 Academic Editor: Francesco Di Raimondo Copyright © 2018 Mahboubeh Rahmani et al. -

Evaluation of Melanocyte Loss in Mycosis Fungoides Using SOX10 Immunohistochemistry
Article Evaluation of Melanocyte Loss in Mycosis Fungoides Using SOX10 Immunohistochemistry Cynthia Reyes Barron and Bruce R. Smoller * Department of Pathology and Laboratory Medicine, University of Rochester Medical Center, Rochester, NY 14642, USA; [email protected] * Correspondence: [email protected] Abstract: Mycosis fungoides (MF) is a subtype of primary cutaneous T-cell lymphoma (CTCL) with an indolent course that rarely progresses. Histologically, the lesions display a superficial lymphocytic infiltrate with epidermotropism of neoplastic T-cells. Hypopigmented MF is a rare variant that presents with hypopigmented lesions and is more likely to affect young patients. The etiology of the hypopigmentation is unclear. The aim of this study was to assess melanocyte loss in MF through immunohistochemistry (IHC) with SOX10. Twenty cases were evaluated, including seven of the hypopigmented subtype. The neoplastic epidermotropic infiltrate consisted predominantly of CD4+ T-cells in 65% of cases; CD8+ T-cells were present in moderate to abundant numbers in most cases. SOX10 IHC showed a decrease or focal complete loss of melanocytes in 50% of the cases. The predominant neoplastic cell type (CD4+/CD8+), age, race, gender, histologic features, and reported clinical pigmentation of the lesions were not predictive of melanocyte loss. A significant loss of melanocytes was observed in 43% of hypopigmented cases and 54% of conventional cases. Additional studies will increase our understanding of the relationship between observed pigmentation and the loss of melanocytes in MF. Citation: Barron, C.R.; Smoller, B.R. Evaluation of Melanocyte Loss in Keywords: mycosis fungoides; hypopigmented mycosis fungoides; SOX10; cutaneous T-cell lymphoma Mycosis Fungoides Using SOX10 Immunohistochemistry. -

Comparison of Clinical Diagnoses and Autopsy Findings in 54 Cases with Lymphoid Neoplasms
Journal of Hematopathology (2019) 12:67–74 https://doi.org/10.1007/s12308-019-00357-9 ORIGINAL ARTICLE Comparison of clinical diagnoses and autopsy findings in 54 cases with lymphoid neoplasms Lara Abraham1 & Hans Kreipe1 & Kais Hussein1 Received: 23 August 2018 /Accepted: 3 May 2019 /Published online: 21 May 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract There are few systematic analyses on autopsy findings of patients with lymphoid neoplasms. Autopsy cases with (n = 54) and without (n = 50) lymphoid neoplasms were compared for this study. Neoplasms found were B cell lymphomas (n =30/54,56%), plasmacytomas (n = 15/54, 28%), T cell lymphomas (n = 7/54, 13%), Hodgkin lymphomas (n = 2/54, 3%) and solid tumours (n = 7/54, 13%). In the control group, 12/50 (24%) cases had solid tumours. Autopsy alone identified the previously unknown lymphoid neoplasm in 10/54 (18%) cases, whilst only 1/50 (2%) previously unknown carcinoma was found in the control group. Cardiac/respiratory failure was the most frequent cause of death in the lymphoid neoplasm group (n =35/54,65%)aswellasin the control group (n = 36/50, 72%). In 8/54 (15%) cases with lymphoid neoplasms and 5/50 (10%) control cases, class I discrepancies were found. This study shows the high rate of autopsy-verified lymphoid neoplasms and unrecognised co- morbidities. Keywords Autopsy . Post-mortem examination . Lymphoma . Plasmacytoma Introduction organ involvement or only post-transplant lymphoprolifera- tive diseases (PTLD) [7–9]. Most of these studies have no The diagnosis of lymphomas and plasmacytomas is a routine control group without haematological neoplasms. -

Intravascular Lymphoma of the Central Nervous System Presenting As Multiple Cerebral Infarctions
CASE REPORT Nagoya J. Med. Sci. 74. 353 ~ 358, 2012 INTRAVASCULAR LYMPHOMA OF THE CENTRAL NERVOUS SYSTEM PRESENTING AS MULTIPLE CEREBRAL INFARCTIONS HIROYUKI MOMOTA1,2, YOSHITAKA NARITA1, YASUJI MIYAKITA1 and SOICHIRO SHIBUI1 1Neurosurgery Division, National Cancer Center Hospital, Tokyo, Japan 2Department of Neurosurgery, Nagoya University Hospital, Nagoya, Japan ABSTRACT A 67-year-old woman presented with an acute onset of left-sided weakness. Magnetic resonance (MR) imaging revealed multiple cerebral infarctions and gadolinium-enhanced lesions in both cerebral hemispheres. Her symptoms once improved after starting steroid treatment; however, soon developed consciousness disturbance and hemiparesis on the left side. She was referred to our hospital where she underwent stereotactic needle biopsy, that revealed an intravascular large B-cell lymphoma in the cerebrum. She received high-dose methotrexate chemotherapy followed by whole-brain radiation therapy, and the MR findings improved. However, her medical condition gradually worsened, and she died 6 months after disease onset. Intravascular lymphoma (IVL) limited to the central nervous system (CNS) is very rare, and the optimal treatment for this medical condition has not been established yet. IVLs showing only neurologic manifestations might be overlooked or misdiagnosed as cerebral infarctions. Here, we present a case of CNS IVL, with its radiographic and pathologic features and treatment with high-dose methotrexate chemotherapy. Key Words: Intravascular lymphoma, Central nervous system, Cerebral infarction This is an Open Access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. To view the details of this license, please visit (http://creativecommons.org/licenses/by-nc-nd/4.0/). INTRODUCTION Intravascular lymphoma (IVL) is a rare variant of mature B-cell neoplasms restricted to the vascular lumina, and this condition preferentially affects the central nervous system (CNS) and skin. -

Intravascular Lymphoma Mimicking Acute Haemorrhagic
Case Report iMedPub Journals Journal of Neurology and Neuroscience 2021 www.imedpub.com ISSN 2171-6625 Vol.12 No.5:367 Intravascular Lymphoma Mimicking Acute Jonathan Naftali1*, Gilad Itchaki2, Haemorrhagic Leucoencephalitis Maor Mermelstein1 and Felix Benninger1 Abstract 1 Department of Neurology, Rabin Medical Center, Petach Tikva, Israel Intravascular lymphoma and Acute Haemorrhagic Leucoencephalitis are rapidly 2 Institute of Hematology, Rabin Medical progressive diseases with poor prognosis. Differentiated between CNS variant Center, Petach Tikva, Israel of IVL and AHLE can be challenging, as they both can be clinically identical. Our case is about 63-year-old female, who presented with rapid onset of cognitive impairment. During her hospitalization, another rapid deterioration has occurred, *Corresponding author: Naftali J and she became tetraplegic, with aphasia, and obtunded. Brain MRI showed many confluent lesions in the white matter, with. Most lesions appeared hemorrhagic. [email protected] After the MRI, a radiological and clinical differential diagnosis between intravascular lymphoma and Acute Haemorrhagic Leucoencephalitis was made. Rapid brain Department of Neurology, Rabin Medical biopsy has revealed the diagnosis of IVL. She had a good responsive to therapy, Center, Petach Tikva, Israel. and regained most of her cognitive and motor functions. Keywords: Intra-vascular lymphoma; Acute haemorrhagic leucoencephalitis Tel: +972-504807751 March 24, 2021; May 07, 2021; May 14, 2021 Received: Accepted: Published: Citation: Naftali J, Itchaki G, Mermelstein M, Benninger F (2021) Intravascular Lymphoma Mimicking Acute Introduction Haemorrhagic Leucoencephalitis. J Neurol Neurosci Vol.12 No.5:367 Intravascular Lymphoma (IVL) is a rare lymphoma, most commonly of B-cell origin. It is classified according to epidemiology and organ involvement: patients of Western variant present the patient was alert but disoriented and anomic, executes frequently with CNS and skin involvement, while in those of partial commands without any other focal neurological signs. -

Primary Cutaneous Lymphoma: ESMO Clinical Recommendations for Diagnosis, Treatment and Follow-Up R
Annals of Oncology 19 (Supplement 2): ii72–ii76, 2008 clinical recommendations doi:10.1093/annonc/mdn095 Primary cutaneous lymphoma: ESMO Clinical Recommendations for diagnosis, treatment and follow-up R. Dummer1 & M. Dreyling2 On behalf of the ESMO Guidelines Working Group* 1Department of Dermatology, University Hospital, Zu¨rich, Switzerland; 2Department of Medicine III, University Hospital Grosshadern, Munich, Germany introduction the quality of life due to their impact on skin appearance and annoying symptoms such as pruritus. In some cases they can Cutaneous lymphomas (CL) are the second most common already be disfiguring in early disease stages. In advanced stages, extranodal non-Hodgkin’s lymphomas. Their incidence is local skin problems are accompanied by systemic immune estimated at 1/100 000 yearly. Primary CL develop by definition suppression which results in an increased risk of infections and in the skin and remain confined to the skin for a long period of secondary malignancies. Some of the late-stage problems in time, while secondary CL reflect cutaneous spread from MF/SS patients might have been aggravated by earlier disseminated primary nodal or extranodal lymphomas. Primary therapeutic interventions, e.g. radiotherapy or phototherapy CL include a wide spectrum of clinically and histologically may contribute to mutations that increase the proliferative heterogeneous lymphoproliferative neoplasms: 75% of CL are and invasive capacity of the tumor cell populations. Cytotoxic cutaneous T-cell lymphomas (CTCL); 25% cutaneous B-cell drugs favor infectious complications. Most patients with lymphomas (CBCL); and a few percent other uncommon advanced disease may die due to secondary problems such as forms. CL and nodal or extracutaneous lymphomas with the infections. -

Treatment of Pagetoid Reticulosis with Intensity Modulated Radiation Therapy Charles Mount Washington University School of Medicine in St
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2014 Treatment of pagetoid reticulosis with intensity modulated radiation therapy Charles Mount Washington University School of Medicine in St. Louis Daniel Ferraro Washington University School of Medicine in St. Louis Alejandro Gru Washington University School of Medicine in St. Louis Matthew rB adbury Washington University School of Medicine in St. Louis Lynn Cornelius Washington University School of Medicine in St. Louis See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Mount, Charles; Ferraro, Daniel; Gru, Alejandro; Bradbury, Matthew; Cornelius, Lynn; and Gay, Hiram, ,"Treatment of pagetoid reticulosis with intensity modulated radiation therapy." Dermatology Online Journal.20,10. (2014). https://digitalcommons.wustl.edu/open_access_pubs/5149 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Authors Charles Mount, Daniel Ferraro, Alejandro Gru, Matthew Bradbury, Lynn Cornelius, and Hiram Gay This open access publication is available at Digital Commons@Becker: https://digitalcommons.wustl.edu/open_access_pubs/5149 Dermatology Online Journal UC Davis Peer Reviewed Title: Treatment of pagetoid reticulosis with intensity modulated radiation therapy Journal Issue: Dermatology Online Journal, 20(10) Author: Mount, Charles, Washington University in St. Louis Ferraro, Daniel, Washington University in St. Louis Gru, Alejandro, Washington University in St. Louis; The Ohio State University Bradbury, Matthew, Washington University in St. Louis Cornelius, Lynn, Washington University in St.