Differentiating Lower Motor Neuron Syndromes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gluteal Muscle Contracture: Diagnosis and Management Options
SICOT J 2017, 3,1 Ó The Authors, published by EDP Sciences, 2017 DOI: 10.1051/sicotj/2016036 Available online at: www.sicot-j.org REVIEW ARTICLE OPEN ACCESS Gluteal muscle contracture: diagnosis and management options Saroj Rai1, Chunqing Meng1,*, Xiaohong Wang1, Nabin Chaudhary2, Shengyang Jin1, Shuhua Yang1, and Hong Wang1 1 Department of Orthopedics, Wuhan Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, #1277 Jiefang Avenue, 430022 Wuhan, P.R. China 2 Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, #1095 Jiefang Avenue, 430030 Wuhan, P.R. China Received 14 April 2016, Accepted 29 October 2016, Published online 6 January 2017 Abstract – Gluteal muscle contracture (GMC), a debilitating disease, exists all over the globe but it is much more prevalent in China. Patients typically present with abduction and external rotation of the hip and are unable to bring both the knees together while squatting. Multiple etiologies have been postulated, the commonest being repeated intramuscular injection into the buttocks. The disease is diagnosed primarily by clinical features but radiological features are necessary for the exclusion of other pathological conditions. Non-operative treatment with physiotherapy can be tried before surgery is considered but it usually fails. Different surgical techniques have been described and claimed to have a better outcome of one over another but controversy still exists. Based on published literatures, the clinical outcome is exceptionally good in all established methods of surgery. However, endoscopic surgery is superior to conventional open surgery in terms of cosmetic outcome with fewer complications. Nevertheless, its use has been limited by lack of adequate knowledge, instrumentations, and some inherent limitations. -

Cancer Cachexia Decreases Specific Force and Accelerates Fatigue in Limb Muscle
Biochemical and Biophysical Research Communications 435 (2013) 488–492 Contents lists available at SciVerse ScienceDirect Biochemical and Biophysical Research Communications journal homepage: www.elsevier.com/locate/ybbrc Cancer cachexia decreases specific force and accelerates fatigue in limb muscle ⇑ B.M. Roberts a, G.S. Frye b, B. Ahn b, L.F. Ferreira b,1, A.R. Judge a,1, a 1225 Center Drive, HPNP Building Room 1142, Department of Physical Therapy, University of Florida, Gainesville, FL 32610, USA b 1864 Stadium Road, Department of Applied Physiology & Kinesiology, University of Florida, Gainesville, FL 32610, USA article info abstract Article history: Cancer cachexia is a complex metabolic syndrome that is characterized by the loss of skeletal muscle Received 30 April 2013 mass and weakness, which compromises physical function, reduces quality of life, and ultimately can Available online 11 May 2013 lead to mortality. Experimental models of cancer cachexia have recapitulated this skeletal muscle atro- phy and consequent decline in muscle force generating capacity. However, more recently, we provided Keywords: evidence that during severe cancer cachexia muscle weakness in the diaphragm muscle cannot be Muscle weakness entirely accounted for by the muscle atrophy. This indicates that muscle weakness is not just a conse- Muscle atrophy quence of muscle atrophy but that there is also significant contractile dysfunction. The current study C-26 aimed to determine whether contractile dysfunction is also present in limb muscles during severe Contractile dysfunction Colon-26 (C26) carcinoma cachexia by studying the glycolytic extensor digitorum longus (EDL) muscle and the oxidative soleus muscle, which has an activity pattern that more closely resembles the dia- phragm. -

The Medical Management of Fibrodysplasia Ossificans Progressiva: Current Treatment Considerations
THE MEDICAL MANAGEMENT OF FIBRODYSPLASIA OSSIFICANS PROGRESSIVA: CURRENT TREATMENT CONSIDERATIONS The International Clinical Consortium on Fibrodysplasia Ossificans Progressiva1 May 2011 From The Center for Research in FOP and Related Disorders, The University of Pennsylvania School of Medicine, Philadelphia, PA 19104 Corresponding Editor: Frederick S. Kaplan, M.D. Isaac and Rose Nassau Professor of Orthopaedic Molecular Medicine Director, Center for Research in FOP & Related Disorders The Perelman School of Medicine - The University of Pennsylvania Department of Orthopaedic Surgery 3737 Market Street – Sixth Floor Philadelphia, PA 19104, USA Tel: (office) 215-294-9145 Fax: 215-222-8854 Email: [email protected] Reprint Requests: [email protected] Associate Editors: Eileen M. Shore, Ph.D. Robert J. Pignolo, M.D., Ph.D. [Kaplan FS, Shore EM, Pignolo RJ (eds), name of individual consortium member, and The International Clinical Consortium on FOP. The medical management of fibrodysplasia ossificans progressiva: current treatment considerations. Clin Proc Intl Clin Consort FOP 4:1-100, 2011] 1See Section X (pages 84-100) for Complete Author Listing. ` 1 ABSTRACT…………………………………………………………………………………………… 5 I. THE CLINICAL AND BASIC SCIENCE BACKGROUND OF FOP……………..…………….. 6 A. Introduction………………………………………………………………..…..…..…………………. 6 B. Classic Clinical Features of FOP……………………………………………………..……………. 6 C. Other Skeletal Anomalies in FOP…………………………………………………………… 6 D. Radiographic Features of FOP……………………………………………………….…….... 7 E. Histopathology of FOP Lesions………………………………………………………………. 7 F. Laboratory Findings in FOP………………………………………………………………… 8 G. The Immune System & FOP…………………………………………………………………. 8 H. Misdiagnosis of FOP………………………………………………………………………………… 8 I. Epidemiologic, Genetic & Environmental Factors in FOP……………………..…………. 9 J. FOP & the BMP Signaling Pathway………………………………………………………… 9 K. The FOP Gene………………………………………………………………..………………. 9 L. Structural and Functional Consequences of the FOP Mutation…………………………… 10 M. -

Spinal and Bulbar Muscular Atrophy
Spinal and bulbar muscular atrophy Description Spinal and bulbar muscular atrophy, also known as Kennedy disease, is a disorder of specialized nerve cells that control muscle movement (motor neurons). These nerve cells originate in the spinal cord and the part of the brain that is connected to the spinal cord (the brainstem). Spinal and bulbar muscular atrophy mainly affects males and is characterized by muscle weakness and wasting (atrophy) that usually begins in adulthood and worsens slowly over time. Muscle wasting in the arms and legs results in cramping; leg muscle weakness can also lead to difficulty walking and a tendency to fall. Certain muscles in the face and throat (bulbar muscles) are also affected, which causes progressive problems with swallowing and speech. Additionally, muscle twitches (fasciculations) are common. Some males with the disorder experience unusual breast development ( gynecomastia) and may be unable to father a child (infertile). Frequency This condition affects fewer than 1 in 150,000 males and is very rare in females. Causes Spinal and bulbar muscular atrophy results from a particular type of mutation in the AR gene. This gene provides instructions for making a protein called an androgen receptor. This receptor attaches (binds) to a class of hormones called androgens, which are involved in male sexual development. Androgens and androgen receptors also have other important functions in both males and females, such as regulating hair growth and sex drive. The AR gene mutation that causes spinal and bulbar muscular atrophy is the abnormal expansion of a DNA segment called a CAG triplet repeat. Normally, this DNA segment is repeated up to about 36 times. -

Spinal Muscular Atrophy
FACT SHEET SPINAL MUSCULAR ATROPHY Spinal Muscular Atrophy (SMA) is a Motor Neuron Disease. It is caused by the mutation of the Survival of SYMPTOMS IN INFANTS • Muscle weakness. Motor Neuron (SMN) gene. It occurs due to the loss of • Muscle atrophy (wasting). motor neurons within the spinal cord and brain. It results • Poor muscle tone. in the progressive wasting away of muscles (atrophy) and • Areflexia (delayed reflexes). muscle weakness. SMA can affect people of all ages, races • Weak cry. or genders; however, the majority of cases occur in infancy • Difficulty sucking or swallowing. or childhood. There are four types of SMA. • Feeding difficulties. FORMS OF SMA • Weak cough. • Lack of developmental milestones (inability to lift head TYPE I (ACUTE INFANTILE) or sit up). • Also called Wernig-Hoffman Disease. • Limpness or a tendency to flop. • Most severe form of SMA. • Accumulations of secretions in the lungs or throat. • Usually diagnosed before six months of age. • Those affected cannot sit without support, lungs may SYMPTOMS IN ADULTS not fully develop, swallowing and breathing may be • Muscle weakness. difficult and there is weakness of the intercostal muscles • Muscle atrophy (wasting). (muscles between the ribs). • Weak tongue. • 95 per cent fatal by 18 • Stiffness. • Cramps. TYPE II (CHRONIC INFANTILE) • Fasciculation (twitching). • Usually diagnosed before the age of two, with the • Clumsiness. majority of cases diagnosed by 15 months. • Dyspnea (shortness of breath). • May be able to sit without assistance or even stand with support. DIAGNOSIS • Increased risk for complications from respiratory • A diagnosis can be made by an SMN gene test which infections. -

Skeletal Muscle Damage in COVID-19: a Call for Action
medicina Review Skeletal Muscle Damage in COVID-19: A Call for Action Amira Mohammed Ali 1,2,* and Hiroshi Kunugi 3,4 1 Department of Psychiatric Nursing and Mental Health, Faculty of Nursing, Alexandria University, Alexandria 21527, Egypt 2 Department of Behavioral Medicine, National Institute of Mental Health, National Center of Neurology and Psychiatry, Tokyo 187-8553, Japan 3 Department of Psychiatry, School of Medicine, Teikyo University, Tokyo 173-8605, Japan; [email protected] 4 Department of Mental Disorder Research, National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo 187-8551, Japan * Correspondence: [email protected]; Tel.: +81-042-346-1986 Abstract: Both laboratory investigations and body composition quantification measures (e.g., com- puted tomography, CT) portray muscle loss in symptomatic Coronavirus disease 2019 (COVID-19) patients. Muscle loss is associated with a poor prognosis of the disease. The exact mechanism of muscle damage in COVID-19 patients, as well as the long-term consequences of muscle injury in disease survivors, are unclear. The current review briefly summarizes the literature for mechanisms, assessment measures, and interventions relevant to skeletal muscle insult in COVID-19 patients. Muscle injury is likely to be attributed to the cytokine storm, disease severity, malnutrition, prolonged physical inactivity during intensive care unit (ICU) stays, mechanical ventilation, and myotoxic drugs (e.g., dexamethasone). It has been assessed by imaging and non-imaging techniques (e.g., CT and electromyography), physical performance tests (e.g., six-minute walk test), anthropometric measures (e.g., calf circumference), and biomarkers of muscle dystrophy (e.g., creatine kinase). Interventions Citation: Ali, A.M.; Kunugi, H. -

Isolated Brachialis Muscle Atrophy
A Case Report & Literature Review Isolated Brachialis Muscle Atrophy John W. Karl, MD, MPH, Michael T. Krosin, MD, and Robert J. Strauch, MD or sensory complaints. His medical history was otherwise Abstract unremarkable. Physical examination revealed obvious wast- Isolated brachialis muscle atrophy, a rare entity with ing of the right brachialis muscle, most notable on the lateral few reported cases in the literature, is explained by a aspect of the distal arm (Figures 1, 2A, 2B). His biceps muscle variety of etiologies. We present a case of unilateral, was functioning with full strength and had a normal bulk. He isolated brachialis muscle atrophy that likely resulted had a normal range of active and passive motion, including from neuralgic amyotrophy. full extension and flexion of both elbows, as well as complete Figure 1. Frontal view of both arms: note the brachialis atrophy solated brachialis muscle atrophy has been rarely reported. (solid arrow) on the right side, although the biceps contracts well. Among the few cases in the literature, 1 was attributed I to a presumed compartment syndrome,1 1 to a displaced clavicle fracture,2 and 3 to neuralgic amyotrophy.3,4 We pres- ent a case of isolated brachialis muscle atrophy of unknown etiology, the presentation of which is consistent with neuralgic amyotrophy, also known as Parsonage-Turner syndrome or brachial plexitis. The patient provided written informed consent for print and electronic publication of this case report. AJO Case Report A 37-year-old right-handed highway worker presented for eval- uation of right-arm muscle atrophy. One year earlier, while lift- ing heavy bags at work, he felt a painful strain in his right arm, although there was no bruising or swelling. -

Whole Exome Sequencing Gene Package Intellectual Disability, Version 9.1, 31-1-2020
Whole Exome Sequencing Gene package Intellectual disability, version 9.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A2ML1 {Otitis media, susceptibility to}, 166760 610627 66 100 100 96 AARS1 Charcot-Marie-Tooth disease, axonal, type 2N, 613287 601065 63 100 97 90 Epileptic encephalopathy, early infantile, 29, 616339 AASS Hyperlysinemia, -
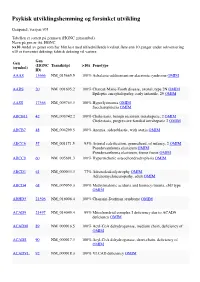
Psykisk Utviklingshemming Og Forsinket Utvikling
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD -

Myalgia As the Revealing Symptom of Multicore Disease and Fibre Type Disproportion Myopathy C Sobreira*, W Marques Jr, a a Barreira
1317 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.74.9.1317 on 21 August 2003. Downloaded from SHORT REPORT Myalgia as the revealing symptom of multicore disease and fibre type disproportion myopathy C Sobreira*, W Marques Jr, A A Barreira ............................................................................................................................. J Neurol Neurosurg Psychiatry 2003;74:1317–1319 toms of CFTDM are more uniform. However, some patients Background: Multicore disease and congenital fibre type exhibit unusual phenotypes such as rigid spine syndrome,10 11 disproportion myopathy are diseases assigned to the significant dysmorphic features,12 or very mild symptoms.13 heterogeneous group of congenital myopathies. Although Cramps are uncommon complaints in patients with multi- hypotonia and muscle weakness appearing in early life core disease or CFTDM and exercise related muscle pain has are the commonest manifestations of these diseases, not been associated with multicore disease. Aimed at contrib- distinct phenotypes and late onset cases have been uting to better delineating the phenotypic expression of these described. myopathies, we present the clinical cases of patients suffering Objective: To report the occurrence of myalgia as the late onset, generalised muscle pain, whose muscle biopsies revealing symptom of multicore disease and fibre type dis- revealed the distinguishing features of either multicore proportion myopathy. disease or CFTDM. Methods: The clinical cases of three patients with fibre type disproportion myopathy and one with multicore CASE REPORTS disease are described. Skeletal muscle biopsies were Patient 1 processed for routine histological and histochemical A 24 year old man was referred to a neurologist owing to studies. exercise related myalgia involving both the upper and lower Results: The clinical picture was unusual in that the symp- limbs. -

Steroid-Induced Myopathy and Its Significance to Respiratory Disease: a Known Disease Rediscovered
Eur Respir J REVIEW 1992, 5, 997-1003 Steroid-induced myopathy and its significance to respiratory disease: a known disease rediscovered P.N.R. Dekhuijzen, M. Decramer Steroid-induced myopathy and its significance to respiratory disease: a known dis Respiratory Muscle Research Unit, ease rediscovered. P.N.R. Dekhuijzen, M. Decramer. Laboratory for Pneumology and Respi ABSTRACT: Skeletal muscle myopathy is a well-known side-effect of systemi ratory Division, University Hospital, cally administered corticosteroids. In recent years renewed attention is being Katholieke Universiteit Leuven, B-3000 Leuvcn, Belgium. paid to the involvement of the respiratory muscles and its consequent signifi cance in pulmonary patients. Two different clinical patterns of steroid-induced Correspondence: M. Decramer, Respira muscular changes are known. In acute myopathy and atrophy after short term tory Division, University Hospital, treatment with high doses of steroids, generalized muscle atrophy and Weligerveld I, 3212 Pellenberg, Bel rhabdomyolysis occur, including the respiratory muscles. Chronic steroid my gium opathy, occurring after prolonged treatment with moderate doses, is character ized by the gradual onset of proximal limb muscle weakness and may be Keywords: Atrophy accompanied by reduced respiratory muscle force. corticosteroids Animal studies demonstrated diaphragmatic myopathy and atrophy similar myopathy respiratory muscles to the alterations in peripheral skeletal muscles. Fluorinated steroids induced selective type lib (fast-twitch -

Massive Indoor Cycling-Induced Rhabdomyolysis in a Patient With
CASE CoMMUNICATIONS IMAJ • VOL 14 • noveMber 2012 Massive Indoor Cycling-Induced Rhabdomyolysis in a Patient with Hereditary Neuropathy with Liability to Pressure Palsy Marganit Benish PhD1, Inna Zeitlin MD2, Dana Deshet MD2 and Yitzhak Beigel MD1,2 1Sackler Faculty of Medicine, Tel Aviv University, Ramat Aviv, Israel 2Department of Medicine D, Wolfson Medical Center, Holon, Israel profoundly decreased. Severe pain exercise-induced rhabdomyolysis, KEY WORDS: PATIENT DESCRIPTION and stiffness were observed when she hereditary neuropathy with liability A 21 year old female was hospitalized stretched both legs. She did not suffer to pressure palsy (HNPP), creatine kinase, indoor cycling, “spinning,” in December 2011 because of pain from any other medical condition and myoglobin and profound weakness in her thighs had no history of recent exposure to IMAJ 2012; 14: 712-714 rendering her unable to walk, and tea- medications, vaccines, alcohol drinking, colored urine. The muscular symptoms or any signs and symptoms of a viral had begun 5 days prior to her admis- infection. Laboratory results showed a sion, starting immediately after she had CK level of 132,170 U/L (range < 10–145 participated, for the first time in her U/L) and increased transaminase levels habdomyolysis is a condition charac- life, in an indoor-cycling class (“spin- (alanine transaminase 280 U/L (< 3–31 R terized by extended myolysis, marked ning”) lasting 45 minutes. The color U/L), aspartate transaminase 1256 U/L elevation of serum creatine kinase and of her urine changed and prompted (< 3–32 U/L) [Table], serum sodium myoglobinuria. Weakness, myalgia, and her to immediately seek medical care.