GM2-Gangliosidosis, AB Variant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sphingolipid Metabolism Diseases ⁎ Thomas Kolter, Konrad Sandhoff
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biochimica et Biophysica Acta 1758 (2006) 2057–2079 www.elsevier.com/locate/bbamem Review Sphingolipid metabolism diseases ⁎ Thomas Kolter, Konrad Sandhoff Kekulé-Institut für Organische Chemie und Biochemie der Universität, Gerhard-Domagk-Str. 1, D-53121 Bonn, Germany Received 23 December 2005; received in revised form 26 April 2006; accepted 23 May 2006 Available online 14 June 2006 Abstract Human diseases caused by alterations in the metabolism of sphingolipids or glycosphingolipids are mainly disorders of the degradation of these compounds. The sphingolipidoses are a group of monogenic inherited diseases caused by defects in the system of lysosomal sphingolipid degradation, with subsequent accumulation of non-degradable storage material in one or more organs. Most sphingolipidoses are associated with high mortality. Both, the ratio of substrate influx into the lysosomes and the reduced degradative capacity can be addressed by therapeutic approaches. In addition to symptomatic treatments, the current strategies for restoration of the reduced substrate degradation within the lysosome are enzyme replacement therapy (ERT), cell-mediated therapy (CMT) including bone marrow transplantation (BMT) and cell-mediated “cross correction”, gene therapy, and enzyme-enhancement therapy with chemical chaperones. The reduction of substrate influx into the lysosomes can be achieved by substrate reduction therapy. Patients suffering from the attenuated form (type 1) of Gaucher disease and from Fabry disease have been successfully treated with ERT. © 2006 Elsevier B.V. All rights reserved. Keywords: Ceramide; Lysosomal storage disease; Saposin; Sphingolipidose Contents 1. Sphingolipid structure, function and biosynthesis ..........................................2058 1.1. -

Attenuation of Ganglioside GM1 Accumulation in the Brain of GM1 Gangliosidosis Mice by Neonatal Intravenous Gene Transfer
Gene Therapy (2003) 10, 1487–1493 & 2003 Nature Publishing Group All rights reserved 0969-7128/03 $25.00 www.nature.com/gt RESEARCH ARTICLE Attenuation of ganglioside GM1 accumulation in the brain of GM1 gangliosidosis mice by neonatal intravenous gene transfer N Takaura1, T Yagi2, M Maeda2, E Nanba3, A Oshima4, Y Suzuki5, T Yamano1 and A Tanaka1 1Department of Pediatrics, Osaka City University Graduate School of Medicine, Osaka, Japan; 2Department of Neurobiology and Anatomy, Osaka City University Graduate School of Medicine, Osaka, Japan; 3Gene Research Center, Tottori University, Yonago, Japan; 4Department of Pediatrics, Takagi Hospital, Saitama, Japan; and 5Pediatrics, Clinical Research Center, Nasu Institute for Developmental Disabilities, International University of Health and Welfare, Ohtawara, Japan A single intravenous injection with 4 Â 107 PFU of recombi- ganglioside GM1 was above the normal range in all treated nant adenovirus encoding mouse b-galactosidase cDNA to mice, which was speculated to be the result of reaccumula- newborn mice provided widespread increases of b-galacto- tion. However, the values were still definitely lower in most of sidase activity, and attenuated the development of the the treated mice than those in untreated mice. In the disease including the brain at least for 60 days. The b- histopathological study, X-gal-positive cells, which showed galactosidase activity showed 2–4 times as high a normal the expression of exogenous b-galactosidase gene, were activity in the liver and lung, and 50 times in the heart. In the observed in the brain. It is noteworthy that neonatal brain, while the activity was only 10–20% of normal, the administration via blood vessels provided access to the efficacy of the treatment was distinct. -

GM2 Gangliosidoses: Clinical Features, Pathophysiological Aspects, and Current Therapies
International Journal of Molecular Sciences Review GM2 Gangliosidoses: Clinical Features, Pathophysiological Aspects, and Current Therapies Andrés Felipe Leal 1 , Eliana Benincore-Flórez 1, Daniela Solano-Galarza 1, Rafael Guillermo Garzón Jaramillo 1 , Olga Yaneth Echeverri-Peña 1, Diego A. Suarez 1,2, Carlos Javier Alméciga-Díaz 1,* and Angela Johana Espejo-Mojica 1,* 1 Institute for the Study of Inborn Errors of Metabolism, Faculty of Science, Pontificia Universidad Javeriana, Bogotá 110231, Colombia; [email protected] (A.F.L.); [email protected] (E.B.-F.); [email protected] (D.S.-G.); [email protected] (R.G.G.J.); [email protected] (O.Y.E.-P.); [email protected] (D.A.S.) 2 Faculty of Medicine, Universidad Nacional de Colombia, Bogotá 110231, Colombia * Correspondence: [email protected] (C.J.A.-D.); [email protected] (A.J.E.-M.); Tel.: +57-1-3208320 (ext. 4140) (C.J.A.-D.); +57-1-3208320 (ext. 4099) (A.J.E.-M.) Received: 6 July 2020; Accepted: 7 August 2020; Published: 27 August 2020 Abstract: GM2 gangliosidoses are a group of pathologies characterized by GM2 ganglioside accumulation into the lysosome due to mutations on the genes encoding for the β-hexosaminidases subunits or the GM2 activator protein. Three GM2 gangliosidoses have been described: Tay–Sachs disease, Sandhoff disease, and the AB variant. Central nervous system dysfunction is the main characteristic of GM2 gangliosidoses patients that include neurodevelopment alterations, neuroinflammation, and neuronal apoptosis. Currently, there is not approved therapy for GM2 gangliosidoses, but different therapeutic strategies have been studied including hematopoietic stem cell transplantation, enzyme replacement therapy, substrate reduction therapy, pharmacological chaperones, and gene therapy. -

Hyperglycopeptiduria in Genetic Mucolipidoses
Tohoku J. exp. Med., 1974, 112, 373-380 Hyperglycopeptiduria in Genetic Mucolipidoses TADAO ORII, TAKAMICHI CHIBA, RYOJI MINAMI, KAZUKO S UKEGAWA and TooRu NAKAO Department of Pediatrics, Sapporo Medical College, Sapporo ORII, T., CHmA, T., MINAMI, R., SUKEUAWA,K. and NAKAO, T. Hyper glycopeptiduria in Genetic Mucolipidoses. Tohoku J. exp. Med., 1974, 112 (4), 373-380 -Urinary cetylpyridinium chloride (CPC)-precipitates and non-CPC- precipitates in normal male children and seven patients with a new type of mucolipidosis, GM1-gangliosidosis type 1, I-cell disease, Hurler syndrome, Morquio syndrome, Gaucher's disease adult type and Tay-Sachs disease were studied using several methods including Sephadex G-25 gel filtration, ECTEOLA-cellulose column chromatography and enzymatic digestion with chondroitinase ABC. 1) Considerable amounts of glycopeptide fractions were detected in the urine of the patients with a new type of mucolipidosis, Gm1-gangliosidosis type 1, I-cell disease and also Gaucher's disease adult type compared with that of normal male children and other patients. 2) The total acid mucopolysaccharides excreted into the urine from two patients with Hurler syndrome and Morquio syndrome were much higher than those excreted in normal male children and other patients. 3) Large amounts of the chondroitinase ABC-resistant acid mucopolysaccharides were found in the urine of patients with Hurler syndrome, Morquio syndrome and Gm,-gangliosidosis type 1. mucolipidoses; glycopeptiduria; Gaucher's disease A group of storage disease which exhibits signs and symptoms of both mucopolysaccharidoses and sphingolipidoses has tentatively been classified as the mucolipidoses by Spranger and Wiedemann (1970). With the exception of the Austin type of sulfatidosis, it has been reported by several workers that the patients with mucolipidosis generally show normal urinary excretion of uronic acid-containing mucopolysaccharides. -

The Nature of Mutation in Krabbe Disease
Am J Hum Genet 30:644-652, 1978 The Nature of Mutation in Krabbe Disease YOAV BEN-YOSEPH,1 MELINDA HUNGERFORD, AND HENRY L. NADLER Krabbe disease (globoid cell leukodystrophy) is a disorder of galactolipid metabolism, inherited in an autosomal recessive manner [1]. Onset in early infancy is followed by rapidly progressive degeneration of the central nervous system, ending in death before the age of 2 years. The primary defect has been ascribed to a deficiency of galactosylceramide /3-galactosidase activity [2]. In addition, a deficiency of /3- galactosidase activities towards psychosine (galactosylsphingosine) [3], monogalac- tosyl diglyceride [4], and lactosylceramide [5] have been reported. The inability to degrade these substrates, found in tissues of children who died of Krabbe disease, indicates that the same enzyme may be acting on the four galactolipids. These activities are, however, normal in patients with GM, gangliosidosis. Hydrolysis of lactosyl- ceramide under different assay conditions [6] and /3-galactosidase activities towards GM, ganglioside, asialo-GMl ganglioside, and asialofetuin (ASF) are deficient in GM, gangliosidosis, but normal in Krabbe disease [7]. Thus, the mutation in Krabbe disease is not allelic with the GM, gangliosidosis mutation, and the observation that antibodies to GM, /3-galactosidase do not precipitate the activities of galactosylceramide 38- galactosidase [8, 9] supports the conclusion that these two /3-galactosidase enzymes are different proteins coded by separate loci. The present study defines the nature of the mutation in Krabbe disease. Using antibodies evoked against the normal galactosylceramide ,3-galactosidase enzyme purified from placenta, we found normal quantities of antigenically cross reacting material of the inactive mutant enzyme in brain, liver, and skin fibroblasts of patients with Krabbe disease. -

HHS Public Access Author Manuscript
HHS Public Access Author manuscript Author Manuscript Author ManuscriptJ Registry Author Manuscript Manag. Author Author Manuscript manuscript; available in PMC 2015 May 11. Published in final edited form as: J Registry Manag. 2014 ; 41(4): 182–189. Exclusion of Progressive Brain Disorders of Childhood for a Cerebral Palsy Monitoring System: A Public Health Perspective Richard S. Olney, MD, MPHa, Nancy S. Doernberga, and Marshalyn Yeargin-Allsopp, MDa aNational Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention (CDC) Abstract Background—Cerebral palsy (CP) is defined by its nonprogressive features. Therefore, a standard definition and list of progressive disorders to exclude would be useful for CP monitoring and epidemiologic studies. Methods—We reviewed the literature on this topic to 1) develop selection criteria for progressive brain disorders of childhood for public health surveillance purposes, 2) identify categories of disorders likely to include individual conditions that are progressive, and 3) ascertain information about the relative frequency and natural history of candidate disorders. Results—Based on 19 criteria that we developed, we ascertained a total of 104 progressive brain disorders of childhood, almost all of which were Mendelian disorders. Discussion—Our list is meant for CP surveillance programs and does not represent a complete catalog of progressive genetic conditions, nor is the list meant to comprehensively characterize disorders that might be mistaken for cerebral -

Mouse Model of GM2 Activator Deficiency Manifests Cerebellar Pathology and Motor Impairment
Proc. Natl. Acad. Sci. USA Vol. 94, pp. 8138–8143, July 1997 Medical Sciences Mouse model of GM2 activator deficiency manifests cerebellar pathology and motor impairment (animal modelyGM2 gangliosidosisygene targetingylysosomal storage disease) YUJING LIU*, ALEXANDER HOFFMANN†,ALEXANDER GRINBERG‡,HEINER WESTPHAL‡,MICHAEL P. MCDONALD§, KATHERINE M. MILLER§,JACQUELINE N. CRAWLEY§,KONRAD SANDHOFF†,KINUKO SUZUKI¶, AND RICHARD L. PROIA* *Section on Biochemical Genetics, Genetics and Biochemistry Branch, National Institute of Diabetes and Digestive and Kidney Diseases, ‡Laboratory of Mammalian Genes and Development, National Institute of Child Health and Development, and §Section on Behavioral Neuropharmacology, Experimental Therapeutics Branch, National Institute of Mental Health, National Institutes of Health, Bethesda, MD 20892; †Institut fu¨r Oganische Chemie und Biochemie der Universita¨tBonn, Gerhard-Domagk-Strasse 1, 53121 Bonn, Germany; and ¶Department of Pathology and Laboratory Medicine, and Neuroscience Center, University of North Carolina, Chapel Hill, NC 27599 Communicated by Stuart A. Kornfeld, Washington University School of Medicine, St. Louis, MO, May 12, 1997 (received for review March 21, 1997) ABSTRACT The GM2 activator deficiency (also known as disorder, the respective genetic lesion results in impairment of the AB variant), Tay–Sachs disease, and Sandhoff disease are the the degradation of GM2 ganglioside and related substrates. major forms of the GM2 gangliosidoses, disorders caused by In humans, in vivo GM2 ganglioside degradation requires the defective degradation of GM2 ganglioside. Tay–Sachs and Sand- GM2 activator protein to form a complex with GM2 ganglioside. hoff diseases are caused by mutations in the genes (HEXA and b-Hexosaminidase A then is able to interact with the activator- HEXB) encoding the subunits of b-hexosaminidase A. -

Prevalence of Lysosomal Storage Diseases in Portugal
European Journal of Human Genetics (2004) 12, 87–92 & 2004 Nature Publishing Group All rights reserved 1018-4813/04 $25.00 www.nature.com/ejhg ARTICLE Prevalence of lysosomal storage diseases in Portugal Rui Pinto1,2, Carla Caseiro1, Manuela Lemos1, Lurdes Lopes1, Augusta Fontes1, Helena Ribeiro1, Euge´nia Pinto1, Elisabete Silva1,So´nia Rocha1, Ana Marca˜o2, Isaura Ribeiro1,2,Lu´cia Lacerda1,2, Gil Ribeiro1,2, Olga Amaral1,2,MCSa´ Miranda*,1,2 1Instituto de Gene´tica Me´dica Jacinto de Magalha˜es, Porto, Portugal; 2Instituto de Biologia Molecular & Celular (IBMC), Portugal Lysosomal storage diseases (LSDs) are a group of inherited metabolic disorders individually considered as rare, and few data on its prevalence has been reported in the literature. The overall birth prevalence of the 29 different LSDs studied in the Portuguese population was calculated to be 25/100 000 live births, twice the prevalence previously described in Australia and in The Netherlands. The comparison of the prevalence profile of the LSDs presenting a prevalence higher than 0.5/100 000 in the Portuguese, Dutch and Australian populations showed, in the Portuguese, the existence of a higher prevalence of GM2 gangliosidoses (B variant), mucolipidoses (II and III), Niemman-Pick type C and metachromatic leukodystrophy (MLD), and a lower prevalence of Pompe and Fabry. The highest prevalence value for a single LSD is the one of GM2 gangliosidoses (B variant), corresponding to 3/100 000, a value which is significantly higher than the prevalence of the most frequent LSD in Dutch, Pompe disease (2/100 000) and Australians, Gaucher’s disease (GD) (1.8/100 000). -

Diagnosis of Metachromatic Leukodystrophy, Krabbe Disease, and Farber Disease After Uptake of Fatty Acid-Labeled Cerebroside Sulfate Into Cultured Skin Fibroblasts
Diagnosis of Metachromatic Leukodystrophy, Krabbe Disease, and Farber Disease after Uptake of Fatty Acid-labeled Cerebroside Sulfate into Cultured Skin Fibroblasts Tooru Kudoh, David A. Wenger J Clin Invest. 1982;70(1):89-97. https://doi.org/10.1172/JCI110607. Research Article [14C]Stearic acid-labeled cerebroside sulfate (CS) was presented to cultured skin fibroblasts in the media. After endocytosis into control cells 86% was readily metabolized to galactosylceramide, ceramide, and stearic acid, which was reutilized in the synthesis of the major lipids found in cultured fibroblasts. Uptake and metabolism of the [14C]CS into cells from typical and atypical patients and carriers of metachromatic leukodystrophy (MLD), Krabbe disease, and Farber disease were observed. Cells from patients with late infantile MLD could not metabolize the CS at all, while cells from an adult MLD patient and from a variant MLD patient could metabolize ∼40 and 15%, respectively, of the CS taken up. These results are in contrast to the in vitro results that demonstrated a severe deficiency of arylsulfatase A in the late infantile and adult patient and a partial deficiency (21-27% of controls) in the variant MLD patient. Patients with Krabbe disease could metabolize nearly 40% of the galactosylceramide produced in the lysosomes from the CS. This is in contrast to the near zero activity for galactosylceramidase measured in vitro. Carriers of Krabbe disease with galactosylceramidase activity near half normal in vitro and those with under 10% of normal activity were found to metabolize galactosylceramide in cells significantly slower than controls. This provides a method for differentiating affected patients from carriers with low enzyme […] Find the latest version: https://jci.me/110607/pdf Diagnosis of Metachromatic Leukodystrophy, Krabbe Disease, and Farber Disease after Uptake of Fatty Acid-labeled Cerebroside Sulfate into Cultured Skin Fibroblasts TOORU KUDOH and DAVID A. -

Morphologic Changes in the Nervous System in Gaucher's Disease, GM2
ANNALS OF C LINICAL AND LABORATORY SCIEN CE, Vol. 5, No. 6 Copyright © 1975, Institute for Clinical Science The Lipidoses: Morphologic Changes in the Nervous System in Gaucher’s Disease, GM2 Gandliosidoses and Niemann-Pick Disease JAMES B. AREY, M.D., Ph.D. St. Christopher’s Hospital for Children, Department of Pediatrics and Pathology, Temple University School of Medicine, Philadelphia, PA. 19140 ABSTRACT The present paper presents, in tabular form, most of the inborn errors of lipid metabolism (exclusive of the hyperlipoproteinemias); some may, with further studies, be removed from this category. Three of the lipidoses and their subtypes which are associated with severe neurologic disorders are discussed, i.e., infantile Gaucher’s disease, Niemann-Pick disease and the GM2 gangliosidoses. Particular emphasis is placed on the importance of careful biochemical and enzymatic studies of either surgical or autopsy material of any patient suspected of having one of the lipidoses. Only by such studies can an exact diagnosis of virtually all of these inborn errors of lipid metabolism be established. Such a diagnosis is im portant, since in many instances an antenatal diagnosis is possible by demon stration of the enzymatic defect in cells grown in tissue culture from the amniotic fluid. Introduction cludes their normal catabolic cycle; the nature of many of these enzymatic defects The lipidoses, here defined as inborn er has been elucidated only within the past 5 to rors of metabolism characterized by an in 10 years and can often be demonstrated not crease of one or more lipids in the tissues, only in the tissues in which the major mor and sometimes in the plasma as well, are phologic changes are present but also in usually transmitted as autosomal recessive other viscera, in circulating leukocytes, in characteristics, with only the homozygously fibroblasts grown in tissue culture and in involved person having the overt disease. -
EGL Test Description
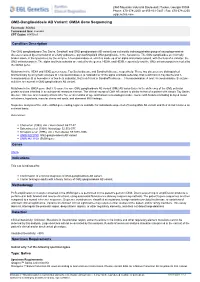
2460 Mountain Industrial Boulevard | Tucker, Georgia 30084 Phone: 470-378-2200 or 855-831-7447 | Fax: 470-378-2250 eglgenetics.com GM2-Gangliosidosis AB Variant: GM2A Gene Sequencing Test Code: SGM2A Turnaround time: 4 weeks CPT Codes: 81479 x1 Condition Description The GM2 gangliosidoses (Tay Sachs, Sandhoff, and GM2 gangliosidosis AB variant) are a clinically indistinguishable group of neurodegenerative diseases caused by accumulation of a fatty substance, glycosphingolipid GM2 ganglioside, in the lysosomes. The GM2 gangliosides are normally broken down, in the lysosomes, by the enzyme ?-hexosaminidase A, which is made up of an alpha and a beta subunit, with the help of a cofactor, the GM2 activator protein. The alpha and beta subunits are coded by the genes, HEXA, and HEXB, respectively and the GM2 activator protein is coded by the GM2A gene. Mutations in the HEXA and HEXB genes cause Tay Sachs disease and Sandhoff disease, respectively. These two diseases are distinguished biochemically by enzymatic analysis of ?-hexosaminidase A (a heterodimer of the alpha and beta subunits), that is deficient in Tay Sachs and ?- hexosaminidase B (a homodimer of two beta subunits), that is deficient in Sandhoff’s disease. ?-hexosaminidase A and ?-hexosaminidase B enzyme activities are normal in GM2 gangliosidosis AB variant. Mutations in the GM2A gene (5q33.1) cause the rare GM2 gangliosidosis AB variant (GM2 AB variant) due to the deficiency of the GM2 activator protein and are inherited in an autosomal recessive manner. The clinical course of GM2 AB variant is similar to that of a patient with classic Tay Sachs disease. Disease onset usually occurs after five or six months of age and follows a neurodegenerative course with features including delayed motor milestones, hypotonia, macular cherry red spots, and abnormal MRI findings. -

Consensus Recommendation for a Diagnostic Guideline for Acid Sphingomyelinase Deficiency
Official journal of the American College of Medical Genetics and Genomics SPECIAL ARTICLE Open Consensus recommendation for a diagnostic guideline for acid sphingomyelinase deficiency Margaret M. McGovern, MD, PhD1, Carlo Dionisi-Vici, MD2, Roberto Giugliani, MD, PhD3, Paul Hwu, MD, PhD4, Olivier Lidove, MD5, Zoltan Lukacs, PhD6, Karl Eugen Mengel, MD7, Pramod K. Mistry, MD, PhD8, Edward H. Schuchman, PhD9 and Melissa P. Wasserstein, MD10 Background: Acid sphingomyelinase deficiency (ASMD) is a rare, base and share personal experience in order to develop a guideline progressive, and often fatal lysosomal storage disease. The underlying for diagnosis of the various ASMD phenotypes. metabolic defect is deficiency of the enzyme acid sphingomyelinase that results in progressive accumulation of sphingomyelin in target Conclusions: Although care of ASMD patients is typically provided tissues. ASMD manifests as a spectrum of severity ranging from rap- by metabolic disease specialists, the guideline is directed at a wide idly progressive severe neurovisceral disease that is uniformly fatal to range of providers because it is important for primary care providers more slowly progressive chronic neurovisceral and chronic visceral (e.g., pediatricians and internists) and specialists (e.g., pulmonolo- forms. Disease management is aimed at symptom control and regular gists, hepatologists, and hematologists) to be able to identify ASMD. assessments for multisystem involvement. Genet Med advance online publication 13 April 2017 Purpose and methods: An