Chapter 2 EMERGENCY PATIENT ASSESSMENT Learning Objectives: • Perform Initial Patient Assessment in a Uniform Manner by All Healthcare Providers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Baseline Vitals &
Baseline Vitals and Sample History Company Drill Instructor Guide Session Reference: 1 Topic: Baseline Vitals and Sample History Company Drill Level of Instruction: 2 Time Required: Three Hours Materials Blood Pressure cuff & stethoscope Pen light Clock or wrist watch with second hand Writing paper Writing pencil Personal protective equipment: gloves References Brady Emergency Care, 11th Edition, The Maryland Medical Protocols for Emergency Medical Services Providers, Effective July 1, 2011, Maryland Institute for Emergency Medical Services Systems Preparation Motivation The Baseline Vitals and SAMPLE History are part of the essential information necessary to obtain and document in order to give a patient the best possible care in the field. This information can alert the provider to call for additional resources if necessary and can give those accepting care of the patient at the next level of patient care a good idea of what may be going on inside the patient’s body. Objective (SPO) 1-1: Given a live victim; blood pressure cuff; stethoscope; pencil; paper; pen light; clock or wrist watch, the student will be able to demonstrate, from memory and without assistance, the proper procedures in obtaining a set of Baseline Vitals, to include: pulse, respirations, skin color, skin temperature and condition, pupil appearance, blood pressure and be able to document the same at a practical station, as governed by The Maryland Medical Protocols for Emergency Medical Services Providers, Effective January 1, 2002 and the Brady Emergency Care, 7th Edition, EMT-Basic National Standard Curriculum. The student will also be able to score a 70% or above on a written exam. -

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
TCCC CLS Skill Instructions Mod 7 25 JAN 20
MODULE 07: AIRWAY MANAGEMENT IN TFC SKILL INSTRUCTIONS 25 JAN 2020 COMBAT LIFESAVER (CLS) TACTICAL COMBAT CASUALTY CARE SKILL INSTRUCTIONS HEAD-TILT/CHIN-LIFT INSTRUCTION TASK: Open an airway using the head-tilt/chin-lift maneuver CONDITION: Given a simulated scenario where a casualty and responder are in combat gear and the casualty is unconscious without a patent airway STANDARD: EffeCtively open the airway by performing the head-tilt/chin-lift maneuver following all steps and measures correctly without Causing further harm to the Casualty EQUIPMENT: N/A PERFORMANCE MEASURES: step-by-step instructions NOTE: Do not use if a spinal or neck injury is suspected. 01 Roll the Casualty onto their back, if necessary, and place them on a hard, flat surface. 02 Kneel at the level of the Casualty’s shoulders. Position yourself at the side of the Casualty. 03 Open the mouth and looK for visible airway obstruCtions (e.g., laCerations, obstructions, broken teeth, burns, or swelling or other debris, such as vomit). NOTE: If foreign material or vomit is in the mouth, remove it as quiCKly as possible. NOTE: Do not perform a blind finger sweep. 04 PlaCe one hand on the Casualty's forehead and apply firm, backward pressure with the palm to tilt the head back. 05 PlaCe the fingertips of the other hand under the bony part of the lower jaw and lift, bringing the Chin forward. NOTE: Do not use the thumb to lift the chin. 06 While maintaining the open airway position, place an ear over the casualty's mouth and nose, looking toward the chest and stomaCh. -

Emergency Medical Responder Febuary Pre Work
EMERGENCY MEDICAL RESPONDER FEBUARY PRE WORK Name___________________________________ MULTIPLE CHOICE. Choose the one alternative that best completes the statement or answers the question. 1) When moving or lifting a patient, you should: 1) A) determine the patient's chief complaint. B) ask bystanders to help. C) use good body mechanics. D) provide emotional support. 2) You have an ethical responsibility to: 2) A) read professional publications. B) maintain your skills and knowledge. C) be ready to perform at all times. D) all of the above. 3) As an Emergency Medical Responder you may be at risk of exposure to an infectious disease when 3) you: A) are talking on the phone. B) handle equipment that has blood on it. C) wear gloves when you care for a patient. D) respond to an emergency. 4) In the anatomical position, the respiratory system would be ________ to the digestive system. 4) A) superior B) anterior C) posterior D) inferior 5) You have a patient with a suspected spinal injury. The best method for movement to the backboard 5) device would be: A) direct carry. B) log roll. C) shoulder drag. D) extremity lift. 6) For patients who have a suspected spinal injury, you should use: 6) A) head-tilt. B) jaw thrust. C) head-tilt, chin-lift. D) chin-lift. 7) You have a patient who experienced an approximately 16-foot fall from the roof while working on 7) the gutters. He is found supine on the driveway and does not respond to verbal or painful stimuli. After assessing the scene and taking spinal restriction, you should proceed to the: A) initial assessment. -

Clinical Handbook Health Care for Children Subjected to Violence Or Sexual Abuse
KINGDOM OF CAMBODIA NATION RELIGION KING MINISTRY OF HEALTH CLINICAL HANDBOOK HEALTH CARE FOR CHILDREN SUBJECTED TO VIOLENCE OR SEXUAL ABUSE 2017 PREFACE Violence against children is a serious public health concern and a human rights violation with consequences that impact their lives in various ways. Violence and sexual abuse suffered in childhood adversely affects the body as well as the mind, which can lead to a broad range of behavioral, psychological and physical problems that persist into adulthood. Healthcare practitioners play a significantly important role in prevention and response to violence against children. They are often the first or only point of reference for children who have experienced violence, detecting abuse and providing immediate and longer-term care and support to children and families. In 2015, the Ministry of Health developed “the National Guidelines for Management of Violence Against Women and Children in the Health Sector”, which provides health care centers and referral hospitals with an overview of prevention and response in the health sector to violence against women and children. This “Clinical Handbook on Health Care for Children Subjected to Violence or Sexual Abuse” elaborates on knowledge and skills required to implement the National Guidelines. It aims to serve as a guide to ensure a prompt and adequate response to child victims of violence or sexual abuse for all healthcare practitioners. It provides further guidance on first line support, medical treatment, psychosocial support, and referral to key social and legal protection services. It can be also used as a resource manual for capacity development and training. Phnom Penh, 30th January 2017 Prof. -

Vital Signs and SAMPLE History
CHAPTER 9 Vital Signs and SAMPLE History Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Overall Assessment Scheme Scene SizeSize--UpUp Initial Assessment Trauma Medical Physical Exam SAMPLE History Vital Signs & Physical Exam SAMPLE History & Vital Signs HOSP Detailed Ongoing Physical Exam Assessment Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Baseline Vital Signs Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Baseline Vital Signs Pulse Respirations Skin Pupils Blood Pressure Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Pulse Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Pulse Rate Adults generally 60-100/minute. Tachycardia is pulse more than 100/minute. Bradycardia is pulse less than 60/minute. More than 120 or less than 50 may be a critical finding. Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Pulse Quality Strong or weak Regular or irregular Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ If you cannot feel a radial or brachial pulse, check the carotid pulse. Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Respirations Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. Upper Saddle River, NJ Respiratory Quality Normal Shallow Labored Noisy Limmer et al., Emergency Care Update, 10th Edition © 2007 by Pearson Education, Inc. -

Sample History and Physical Note for Gout
Sample History and Physical Note Charting Plus™ - Electronic Medical Records www.medinotes.com Note for Jane Doe on 2/27/04 - Chart 5407 Chief Complaint: This 31 year old female presents today with abdominal pain. Duration: Condition has existed for one month. Modifying Factors: Patient indicates lying down improves condition and standing worsens condition. Severity: The severity has worsened over the past 3 months. LMP: 4-05-2002. Allergies: Patient admits allergies to penicillin. Medication History: None. Past Medical History: Past medical history is unremarkable. Past Surgical History: Patient admits past surgical history of (+) cholecystectomy in 1998. Social History: Patient denies alcohol use. Patient denies illegal drug use. Patient denies STD history. Patient denies tobacco use. Family History: Patient admits a family history of cancer of breast associated with mother. Review of Systems: Cardiovascular: (-) cardiovascular problems or chest symptoms Constitutional Symptoms: (-) constitutional symptoms such as fever, headache, nausea, dizziness Genitourinary: (-) GU symptoms Physical Exam: BP Standing: 118/72 Resp: 18 HR: 68 Height: 5 ft. 7 in. Weight: 134 lbs. Patient is a 31 year old female who appears pleasant, in no apparent distress, her given age, well developed, well nourished and with good attention to hygiene and body habitus. Eyes: Conjunctiva and lids reveal no signs or symptoms of infection. Pupil exam reveals round and reactive pupils without afferent pupillary defect. Optic discs with normal color, contour and cupping bilaterally. Retinas are flat with normal vasculature out to the far periphery with no peripheral holes, breaks or tears observed. ENT: Gross hearing test reveals normal hearing. Inspection of bilateral ears reveals no masses, swelling, redness or drainage. -

Patient Assessment?
EMERGENCY MEDICAL TECHNICIAN ‐ BASIC What is Patient Assessment? Why is Patient Assessment important? MECTA EMS Learning Assistant 2 What are the phases of patient assessment? Review of Dispatch Information Scene Survey Initial Assessment Focused History and Physical Exam Detailed Physical Exam Ongoing Assessment Communication Documentation MECTA EMS Learning Assistant 3 Why is the order of Patient Assessment important? Why is it necessary to develop a method of assessment and use that method on all patients? MECTA EMS Learning Assistant 4 SCENE SIZE‐UP INITIAL ASSESSMENT Trauma FOCUSED HISTORY & FOCUSED HISTORY & PHYSICAL EXAM PHYSICAL EXAM Patient Patient DETAILED DETAILED PHYSICAL EXAM PHYSICAL EXAM Medical ON‐GOING ASSESSMENT MECTA EMS Learning Assistant 5 Begin with receipt of call Location Incident Injured/Injuries MECTA EMS Learning Assistant 6 Continue En Route Further info from dispatcher Observe ▪ Smoke? ▪ Fire? ▪ High line wires? ▪ Railroads? ▪ Water? ▪ Industry? ▪ Other Public Safety units? MECTA EMS Learning Assistant 7 Upon Arrival Observe ▪ Overall scene ▪ Location of victim(s) ▪ Possible Mechanisms of Injury MECTA EMS Learning Assistant 8 Upon Arrival Observe ▪ Hazards ▪ Crowds ▪ HazMat ▪ Electricity ▪ Gas ▪ Fire ▪ Glass ▪ Jagged metal ▪ Stability of environment ▪ Traffic ▪ Environment MECTA EMS Learning Assistant 9 Ensure Safety ▪ Yourself ▪ Partner ▪ Other rescuers/Bystanders ▪ Patient MECTA EMS Learning Assistant 10 Call for assistance ▪ Other EMS Units ▪ Law Enforcement ▪ Fire Department ▪ -
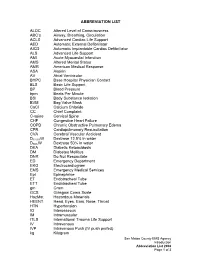
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Pediatric First Aid for Caregivers and Teachers, Second Edition
Pediatric First Aid for Caregivers and Teachers, Second Edition Check Your Knowledge: Answer Key TOPIC 1 1. Pediatric first aid is: a. Cardiopulmonary resuscitation (CPR) b. Immediate medical care given to a child who is injured or suddenly becomes sick c. Required only if a child’s parent or guardian cannot arrive quickly d. Provided only by physicians, nurses, and paramedics 2. Good Samaritan laws: a. Protect a person from legal responsibility when giving first aid in an emergency b. Cover physicians and nurses from malpractice lawsuits c. Do not apply in Texas and Georgia d. Require that someone who comes on the scene of an accident must stop and offer to help 3. Training in pediatric first aid, CPR, and choking relief is: a. Recommended only for caregivers of children younger than 3 years b. Recommended only for caregivers who supervise wading and swimming activities c. Recommended only for caregivers who are caring for a child with a heart condition d. Recommended for all caregivers 4. The 4Cs of Pediatric First Aid are: a. Call, Care, Complete, Collaborate b. Check, Call, Care, Complete c. Call, Check, Care, Complete d. Care, Call, Check, Complete 5. Every child care facility should have policies for: a. Care of children and staff who are ill b. Urgent medical situations c. Disasters d. All of the above. Copyright © 2014 Jones & Bartlett Learning, LLC, an Ascend Learning Company and the American Academy of Pediatrics 1 41894_ANSx_PASS02.indd 1 18/02/13 9:42 AM Pediatric First Aid for Caregivers and Teachers, Second Edition Check Your Knowledge: Answer Key TOPIC 2 1. -

Career Technical Credit Transfer (CT²) Emergency Medical Technician-Basic (EMT-B) Career Technical Assurance Guide (CTAG) October 17, 2008
Adopted Career Technical Credit Transfer (CT²) Emergency Medical Technician-Basic (EMT-B) Career Technical Assurance Guide (CTAG) October 17, 2008 The following course or Career-Technical Assurance Number (CTAN) is eligible for transfer between career-technical education, adult workforce education, and post-secondary education. CTEMTB002 – Emergency Medical Technician – Basic (EMT-B) Credits: 7 Semester/10 Quarter Hours Advising Notes: Submitted course work must include proof of laboratory and clinical components. Those persons holding current Ohio certification as an EMT-Basic will be given what the receiving institution is offering as credit for its CT² approved EMT-B course. The awarding of credit for the EMT-B course of s t u d y m a y decrease the time to associate degree completion, when such a degree is offered, but will not replace any portion of the EMT-Intermediate or EMT- Paramedic curricula as the later two are separate courses of study. Prerequisite: Current Ohio EMT-Basic Certification Module I Preparatory Module II Patient Assessment Module III Airway and Cardiac Arrest Management Module IV Trauma Patient Management Module V Medical Patient Management Clinical Experience and/or Pre-Hospital Internship Minimum Hours = 120 Didactic 10 Clinical Experience and/or Pre-Hospital Internship Note: Credit hours assigned to CTANs are “relative values,” which are used to help determine the equivalency of submitted coursework or content. Once approved by a validation panel as a CT² course, students will be given what the receiving institution is offering as credit for its CT² approved course. The CTAN illustrates the learning outcomes that are equivalent or common in introductory technical courses. -
NY State-Wide EMT/AEMT BLS Protocols
STATE OF NEW YORK DEPARTMENT OF HEALTH Corning Tower The Governor Nelson A. Rockefeller Empire State Plaza Albany, New York 12237 Antonia C. Novello, M.D., M.P.H., Dr.P.H. Dennis P. Whalen Commissioner Executive Deputy Commissioner February 1, 2003 Dear EMS Agency: EMS Agencies and Course Sponsors in the State of New York will be receiving copies of the 2003 version of the New York State Basic Life Support Protocols for Emergency Medical Technicians and Advanced Emergency Medical Technicians. The protocols were developed by the State Emergency Medical Advisory Committee and approved by the State EMS Council. The new protocols have been updated to meet the current standard of care within New York State and to reflect all recent curriculum changes. These new protocols do not pertain to Certified First Responders. A separate protocol book for CFRs is in the final development stages at the State Emergency Medical Advisory Committee. Until the new CFR protocols are released, CFRs may use the new EMT/AEMT BLS protocols up to their level of training and scope of care within the State of New York. CFRs may also refer to their Regional Emergency Medical Advisory Committee and their agency Medical Director for clarification and advise. The new EMT/AEMT BLS protocols will be implemented in the following manner: 1. First, all EMS agencies in New York State must update all of their NYS EMS certified personnel to the new protocols by August 1st, 2003. On August 1st, 2003 the protocols will be in use by all EMS agencies across the state.