Item-8.3-Covid-19-An
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Review of Bus Services in the East Riding (Revised Following Public Consultation)
East Riding of Yorkshire Council Review of Bus Services in the East Riding (Revised following Public Consultation) December 2016 1 Review of Bus Services in the East Riding 2016 (Revised following Public Consultation) Table of Contents Page SECTION 1 The Review of Bus Services in the East Riding 2016: Background and Context. 5 SECTION 2 The Public Consultation on our proposals in the Review of Bus Services in the 7 East Riding 2016: Results and Analysis. SECTION 3 Summary by contract of our conclusions following analysis of the results of the 12 public consultation SECTION 4 Our Finalised Proposal for the future of supported bus services in the East 16 Riding and individual Bus Timetables for services which would be affected. 3 4 Section 1 The Review of Bus Services in the East Riding 2016: BACKGROUND AND CONTEXT 1.1 Following a comprehensive Parish Transport Needs Assessment journeys. We stated our intention to seek to develop alternative process the council developed a proposal for the future of mitigating transport options for the loss of these 59 contracts. supported bus services in the East Riding of Yorkshire. This These potential mitigation measures included either existing or proposal was subject to a full public consultation which ran proposed demand responsive transport options, or the possibility for 8 weeks from 27 June 2016 to 28 August 2016. We have of travelling on a different bus or at a different time. given due regard to what residents have told us through the consultation process, and have revised our original proposal to 1.7 We consulted on this proposal, through advertising a survey ensure that we can maintain a public and community transport online at: www.eastriding.gov.uk/haveyoursay network that meets people’s strategic transport needs. -

Hull Driving Test Centre Routes
Hull Driving Test Centre Routes To make driving tests more representative of real-life driving, the DVSA no longer publishes official test routes. However, you can find a number of recent routes used at the Hull driving test centre in this document. While test routes from this centre are likely to be very similar to those below, you should treat this document as a rough guide only. Exact test routes are at the examiners’ discretion and are subject to change. Route Number 1 Road Direction Driving Test Centre Reservoir Rd Left Clough Rd Roundabout right Bankside Roundabout right Air St/Sculcoates Lane Traffic light right Beverley Rd Traffic light left Cottingham Rd 3rd traffic light 2nd right Cottingham Grove Ahead Skidby Grove End of road right Inglemire Lane 2nd left Oldstead Avenue 2nd light Grangeside Avenue End of road right Oldstead Avenue End of road right Endike Lane Roundabout ahead, end of road left Beverley Rd Right traffic light Sutton Rd Roundabout ahead, roundabout right Holwell Rd Roundabout ahead Stoneferry Roundabout right Ferry Lane Roundabout ahead Clough Rd Right Reservoir Rd Driving Test Centre Chamberlain Rd 2nd right Driving Test Centre Route Number 2 Road Direction Driving Test Centre Reservoir Rd Left Clough Rd Roundabout ahead Ferry Lane Roundabout right Stoneferry Rd Roundabout left Chamberlain Rd Roundabout ahead Laburnum Avenue 1st right Lilac Avenue 3rd left Elm Avenue End of road left James Reckitt Avenue Roundabout left Mount Pleasant Right traffic light Holderness Rd 1st left Brazil St End of road right -

The Kingston Upon Hull (Bransholme Area) Education Action Zone (Extension and Variation) Order 2001
Status: This is the original version (as it was originally made). This item of legislation is currently only available in its original format. STATUTORY INSTRUMENTS 2001 No. 3840 EDUCATION, ENGLAND The Kingston upon Hull (Bransholme Area) Education Action Zone (Extension and Variation) Order 2001 Made - - - - 28th November 2001 Laid before Parliament 3rd December 2001 Coming into force - - 1st January 2002 Whereas an application for the purpose of extending and varying an Education Action Zone has been made to the Secretary of State with the consent of the governing bodies of every school participating in the zone. Now, therefore, in exercise of the powers conferred on the Secretary of State by sections 10(2), 10(3) and 138(7) of the Schools Standards and Framework Act 1998(1), the Secretary of State for Education and Skills hereby makes the following order: Citation and Commencement 1. This order shall be cited as the Kingston upon Hull (Bransholme Area) Education Action Zone (Extension and Variation) Order 2001 and shall come into force on 1st January 2002. Interpretation 2. In this order— “Kingston upon Hull (Bransholme Area) Education Action Zone” means the Education Action Zone established by the Kingston upon Hull (Bransholme Area) Education Action Zone Order 1998(2). Extension of the Kingston upon Hull (Bransholme Area) Education Action Zone Order 1998 3. The Kingston upon Hull (Bransholme Area) Education Action Zone is extended for a further period of two years beginning with 1st January 2002. Variation of the Kingston upon Hull (Bransholme Area) Education Action Zone Order 1998 4. There shall be inserted after article 9 of the Kingston upon Hull (Bransholme Area) Education Action Zone Order 1998 the following article— (1) 1998 c. -

FID Sheet1__Di 0 Lonsdale Community Centre 1 4 Seasons 2 4
FID Sheet1__Di 0 Lonsdale Community Centre 1 4 Seasons 2 4 Seasons 3 Unity in Community 4 URBaN 5 Goodwin Development Trust 6 The Lemon Tree Children's Centre 7 Pickering and Newington Development Association 8 Job Centre Plus 9 The Freedom Centre 10 Marfleet Children's Centre 11 Sight Support Hull & East Yorkshire 12 Fenchurch Children's Centre 13 Parks Children's Centre 14 Priory Children's Centre 15 Avenue's Library 16 Bransholme Library 17 Fred Moore Library 18 Freedom Centre Library 19 Gipsyville Library 20 Greenwood Avenue Library 21 Ings Library 22 Longhill Library 23 Waudby Library 24 Western Library 25 East Park Library 26 Hull Central Library 27 Bransholme Customer Service Centre 28 Orchard Customer Service Centre 29 The Wilson Centre Customer Service Centre 30 Autism Plus Sheet1__F2 8 Lonsdale Street, Hull HU3 6PA HU9 3QB HU1 3SQ 501 Endike Lane, Hull, HU6 8AQ 9 Appin Close, North Bransholme, Hull HU7 5BB The Octagon, Walker Street, Hull, HU3 2RE Lothian Way, Hull, HU7 5DD Gipsyville Multi Purpose Centre, 729-730 Hessle Road, Hull HU4 6JA Britannia House, 2 Ferensway, Hull, HU2 8NF 97 Preston Road, Hull HU9 3QB Preston Road, Hull, HU9 5AN 466 Beverley Road, Hull HU5 1NF Fenchurch Street, Hull HU5 1JF Treehouse, Courtway Road, Hull HU6 9TA Priory Road, Hull HU5 5RU 76 Chanterlands Avenue, Hull HU5 3TD North Point Shopping Centre, Hull HU7 4EF Wold Road, Hull HU5 5UN 97 Preston Road, Hull HU9 3QB Gipsyville Multi-Purpose Centre, Hull, HU4 6JA 220 Greenwood Avenue, Hull HU6 9RU Savoy Road, Hull HU8 0TY St Margaret's Church, Shannon Road, Hull HU8 9PD Waudby Centre, Hull HU9 5LD 254 Boulevard, Hull HU3 3ED Central Pavilion, Holderness Road, Hull HU8 8JE Albion Street, Hull HU1 3TF The Bransholme Health Centre, Goodhart Road, Hull, HU7 4DW The Orchard Centre, Orchard Park Road, Hull, HU6 9BX Alfred Gelder Street, Hull, HU1 2AG Ings Plus, Savoy Road, Hull, HU8 0TX Sheet1__F3 Sheet1__F9 LLPG_FID LLPG_UPRN LLPG_Easti Newington & Gipsyville 010000201796 83783 010000201796 507290 Southcoates - Freedom Centre 010070551198 105068 010070551198 513190 St. -
Putting Music at the Heart of Hull 2019 – 2020 REPORT
Putting Music at the Heart of Hull 2019 – 2020 REPORT Hull Music Service – putting music at the heart of Hull Each Local Authority Area has a Music Education Hub. The national funding for Music Education Hubs comes from the Department for Education and is administered by Arts Council England (ACE). Hull Music Service is the Lead Partner for Hull Music Hub and commits to delivering on 4 Core Roles and 3 Extension Roles: National Plan for Music Education Core Roles 1. Ensure that every child aged 5 to 18 has the opportunity to learn a musical instrument (other than voice) through whole-class ensemble teaching programmes for ideally a year (but for a minimum of a term) of weekly tuition on the same instrument 2. Provide opportunities to play in ensembles and to perform from an early stage 3. Ensure that clear progression routes are available and affordable to all young people 4. Develop a singing strategy to ensure that every pupil sings regularly and that choirs and other vocal ensembles are available in the area Extension Roles 1. Offer continuing professional development to school staff, particularly in supporting schools to deliver music in the curriculum 2. Provide an instrument loan service, with discounts or free provision for those on low incomes 3. Provide access to large-scale and/or high-quality music experiences for pupils, working with professional musicians and/or venues. This may include undertaking work to publicise the opportunities available to schools, parents/carers and students Hull City Council Corporate Plan At a local level, the Hull Music Hub appears strategically in the Hull City Council Corporate Plan 2018 – 2022. -

A Moth for Amy Is an Amy Johnson Festival a Moth for Amy 40 APLE RD Project
THOMAS CLARKSON A1079 41 WA 9 42 WNE ROAD A Moth for Amy is an Amy Johnson Festival A Moth for Amy 40 APLE RD project. Amy was one of the most influential BARNST and inspirational women of the twentieth WA ROBSON century. She was the first woman to fly solo GREENWOOD AVENUE A Moth for Amy is an animal sculpture the original sculpture, from which Y GANSTEAD LANE GANSTEAD WA SUTTON PARK LANE GANSTEAD from England to Australia and set a string WELL RD trail with a dierence. our flutter of Moths has hatched. The ENDYKE LANE SUTTON ROAD Y GOLF COURSE of other records throughout her career. Our HOL 59 Moths, each measuring almost SHANNON RD 43 MAIN ROAD festival over the summer of 2016 celebrated Inspired by Amy Johnson’s de 1.5m across, have been decorated by LEADS ROAD Amy’s life, achievements and legacy on the Havilland Gipsy Moth plane, in which artists and community groups, making INGLEMIRE LANE 75th anniversary of her death. The festival BEVERLEY ROAD SAL she made her epic flight to Australia each Moth a unique work of art. The SUTTON ROAD TSHOUSE ROAD HULL ROAD aimed to raise awareness of Amy Johnson’s in 1930, a flutter of exotic giant moths designs are inspired by Amy Johnson’s achievements as an aviator, as an engineer has alighted on walls and plinths achievements, her flight to Australia UNIVERSITY and as a woman of her time, one of the first LEADS ROAD across Hull, East Yorkshire and beyond! and the era in which she lived. -

INTERNAL POST Members Information INTERNAL POST
HUMBER BRIDGE Councillor L Redfern Councillor D Gemmell BOARD North Lincolnshire Council, Civic Kingston upon Hull City Council Centre Ashby Road Scunthorpe DN16 1AN Councillor S Parnaby OBE, Councillor C Shaw Lord C Haskins East Riding of Yorkshire Council North East Lincolnshire Council Quarryside Farm, County Hall Skidby, Beverley Cottingham, HU17 9BA East Yorkshire, HU16 5TG Mr S Martin Professor D Stephenson Mr J Butler Chief Executive, Clugston Clerk to the Humber Bridge 33 Hambling Drive Group Ltd Board Molescroft St Vincent House, Normanby Beverley Road, Scunthorpe HU17 9GD DN15 8QT Mr P Hill Mr P Dearing Anita Eckersley General Manager and Legal Services Committee Clerk to the Humber Bridgemaster Kingston upon Hull City Council Bridge Board Humber Bridge Administration Offices Ferriby Road, Hessle HU13 0JG Councillor Turner MBE, Other recipients for Mrs J Rae, Audit Commission Lincolnshire County Council information, Audit Commission c/o Hull City Council, Floor 2 Wilson Centre, Alfred Gelder Street, Hull HU1 2AG Nigel Pearson Simon Driver Shaun Walsh, Chief Executive Chief Executive Chief Executive East riding of Yorkshire Council North Lincolnshire Council North East Lincolnshire Council Civic Centre, Ashby Road Municipal Offices, Town Hall Scunthorpe Square, Grimsby DN16 1AN DN31 1HU INTERNAL POST INTERNAL POST Members Information Reference Library APPEALS COMMITTEE Councillor Abbott Councillor Conner Councillor P D Clark INTERNAL MAIL INTERNAL MAIL G Paddock K Bowen Neighbourhood Nuisance Team Neighbourhood Nuisance Team HAND -

Local Area Map Taxis
Hull Paragon Station i Onward Travel Information Buses & Taxis & Cycles & Mobility Scooters Local area map Hull is a area. PlusBus Contains Ordnance Survey data © Crown copyright and database right 2018 & also map data © OpenStreetMap contributors, CC BY-SA Rail replacement buses/coaches depart from the Bus Interchange Stands PlusBus is a discount price ‘bus pass’ that you buy with your train ticket. It gives you unlimited bus travel around your A to D. chosen town, on participating buses. Visit www.plusbus.info Main destinations by bus (Data correct at July 2019) DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP 151, 152, 153, 75, 76, 77, 78, { Anlaby 8 18 Hedon 35 36 Setting Dyke 63 9 154, 155, X55 79, 277 2, 151, 152, 66, 155, 250, Skirlaugh 240 27 { Anlaby Park 6 8 { Hessle ^ 7 18 30 153, 154 350, X55 { Spring Cottage 11, 11A 24 29 Barton-upon-Humber 250, 350 30 { HM Prison Hull 75, 76, 77 36 Sproatley 277 35 Bilton 56, 57, 277 26 35 10 minutes walk from this (for Burton Constable Hall) { Hull Royal Infirmary Station or take any bus from { Sutton Park 7, 8, 8A, 8X 17 29 { Bilton Grange 4, 4A, 50 28 34 stand {6} {7} {8} or {9} 155, 250, 350, 1, 1W, 2, 51, Humber Bridge [ 18 30 { Sutton Village 11, 12 22 24 X55 { Boothferry Estate 66, 155, 250, 3 5 6 7 18 30 Swanland 153 8 350, X55 { Ings Road Estate 11, 11A 24 7, 7N, 8, 8A, "KCOM Craven Park Stadium" Thorngumbald 75, 76, 77 36 Bransholme (Interchange) & 8X, 9, 9A, 10, { 3, 3A 32 { 17 21 22 23 24 29 (for Hull Kingston Rovers RLFC) North -

933 Bus Time Schedule & Line Route
933 bus time schedule & line map 933 Burstwick - Wyke College View In Website Mode The 933 bus line (Burstwick - Wyke College) has 2 routes. For regular weekdays, their operation hours are: (1) Bricknell Estate <-> Burstwick: 4:15 PM (2) Burstwick <-> Bricknell Estate: 7:20 AM Use the Moovit App to ƒnd the closest 933 bus station near you and ƒnd out when is the next 933 bus arriving. Direction: Bricknell Estate <-> Burstwick 933 bus Time Schedule 57 stops Bricknell Estate <-> Burstwick Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 4:15 PM Bishop Alcock Road, Bricknell Estate Tuesday 4:15 PM Leyburn Avenue, Bricknell Estate Wednesday 4:15 PM Welton Grove, Bricknell Estate Thursday 4:15 PM Arram Grove, Inglemire Friday 4:15 PM Endyke Lane, Inglemire Saturday Not Operational Lastingham Close, Orchard Park 32nd Avenue, Orchard Park 933 bus Info 22nd Avenue, Orchard Park Direction: Bricknell Estate <-> Burstwick Stops: 57 Trip Duration: 71 min Greenwood Ave Library, Orchard Park Line Summary: Bishop Alcock Road, Bricknell Estate, Ada Holmes Circle, Kingston Upon Hull Leyburn Avenue, Bricknell Estate, Welton Grove, Bricknell Estate, Arram Grove, Inglemire, Endyke 6th Avenue, Orchard Park Lane, Inglemire, Lastingham Close, Orchard Park, 32nd Avenue, Orchard Park, 22nd Avenue, Orchard 2nd Avenue, Orchard Park Park, Greenwood Ave Library, Orchard Park, 6th Avenue, Orchard Park, 2nd Avenue, Orchard Park, Beverley Road, Ghost Estate Beverley Road, Ghost Estate, Elston Close, Ghost Estate, Ennerdale Leisure Centre, Sutton Park, -
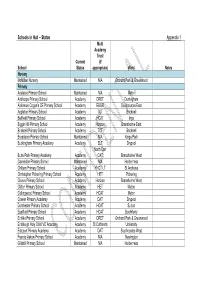
Schools in Hull – Status Appendix 1
Schools in Hull – Status Appendix 1 Multi Academy Trust Current (if School Status appropriate) Ward Notes Nursery McMillan Nursery Maintained N/A Orchard Park & Greenwood Primary Adelaide Primary School Maintained N/A Myton Ainthorpe Primary School Academy DRET Derringham Alderman Cogan's CE Primary School Academy EBOR Southcoates East Appleton Primary School Academy TCT Bricknell Bellfield Primary School Academy HCAT Ings Biggin Hill Primary School Academy Horizon Bransholme East Bricknell Primary School Academy TCT Bricknell Broadacre Primary School Maintained N/A Kings Park Buckingham Primary Academy Academy ELT Drypool North Carr Bude Park Primary Academy Academy CAT Bransholme West Cavendish Primary School Maintained N/A Holderness Chiltern Primary School Academy YHCT LT St Andrews Christopher Pickering Primary School Academy HET Pickering Cleeve Primary School Academy Horizon Bransholme West Clifton Primary School Academy HET Myton Collingwood Primary School Academy HCAT Myton Craven Primary Academy Academy DAT Drypool Dorchester Primary School Academy HCAT Sutton Eastfield Primary School Academy HCAT Boothferry Endike Primary School Academy DRET Orchard Park & Greenwood Endsleigh Holy Child VC Academy Academy St Cuthberts University Estcourt Primary Academy Academy DAT Southcoates West Francis Askew Primary School Academy N/A Newington Gillshill Primary School Maintained N/A Holderness Multi Academy Trust Current (if School Status appropriate) Ward Notes Griffin Primary School Academy VAT Marfleet Hall Road Academy Academy AET -

North Hull Local Travel
D A O R X U A E M M AI N S TR E EE AN T L EN RE G E A N 1 E L 1 2 0 /2 ARN 1 mile 1 / 2 Miles THE S H 0 1/2 1 km 11/2 2 kms 21/2 3 Kms U U T L T 10 minutes walking time L O R 11 N O 1 grid square = 1 Kilometre (0.6 miles) A If you walk at - 3 miles per hour (moderate) 4 mph (average) 5 mph (quick) D North Hull R O 10 minutes cycling time A D If you cycle at - 8 miles per hour (moderate) 10 mph (average) 12 mph (quick) Local Travel Map B E CUMBRIAN WAY VE RL EY Y ( S S A W O N U W A O T W H W - Holderness Drain W N D N North O E l O S E l D T N ) u Bransholme W B SN O R WAY Y- H P O A S r A S ve D Ri IAN TH WAY O L PEN 10 NIN E To Beverley W A Y Highlands B E Health Centre V E E R AY N N W Highlands L GRAMPIA A E L DU N Y R SWELL LA N O E N O R R I C NE O A M H MOND L Broadacre L A Y O H A T T D R Dunswell H R W U I O N P A N N E N E N Barmston Drain Y D N N Beverley and M Kingswood A N L I W Y N O E W A D A E M E Y A E H W V C D W I KIN E E G SB R U E . -

Hull Welcomes All Seafarers
PLACES OF WORSHIP SEAFARERS’ PORT HULL SEAFARERS’ CENTRE Roman Catholic: Sacred Heart, Southcoates Lane INFORMATION LEAFLET www.sacredhearthull.uk 01482 376 332 Anglican: Hull Minster, Market Place Open 24hrs a day / 7 days a week www.hullminster.org 01482 224 460 HULL Danish Seamen’s Church: 104 Osborne Street www.danchurchhull.co.uk 01482 225 469 WELCOMES ALL via access code C634XY SEAFARERS Internet Café • Free Wi-Fi Out of hours Emergency No: 07906 661 633 SEAFARERS’ INTERNET HULL SEAFARERS’ CENTRE DATA & SIM CARDS United House, King George Dock West, Hull, HU9 5PR Telephone cards are also available for purchase at the Hull Seafarers’ Tel: 01482 376 322 Centre and from Ship Welfare Visitors representing the centre. Seafarers Email:[email protected] are strongly advised to purchase telephone cards only from official Hull Seafarers’ Centre representatives or a Port Chaplain. SHIP WELFARE VISITING ORGANISATIONS Apostleship of the Sea SEAFARERS’ TELEPHONE HELPLINES Port Chaplain +44 (0) 7906 661 633 SeafarerHelp....the lifeline for seafarers The Mission to Seafarers 07387 022 375 wwww.seafarerhelp.org (All seafarers) +44 20 7323 2737 Port Chaplain A seafarer making use of the Wi-Fi in the Hull Seafarers’ Centre. Seafarer Support Referral Helpline Fishermen’s Mission +44 (0) 1482 323 440 PORT OFFICE & SECURITY www.seafarersupport.org (UK seafarers only) 0800 121 4765 07917 754 527 ABP House 01482 327 171 Danish Seamen’s Church 01482 225 469 Port Security (24hr service) 01482 781 867 LOCAL PORT HEALTH AUTHORITY Nautilus International 020 8989 6677 Hull & Goole Port Health Authority 01482 324 776 RMT 020 7387 4771 [email protected] Produced by the Merchant Navy Welfare Board, registered as a charity No.212799 in England & Wales, and No.SC039669 in Scotland.