Birth Control
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A History of Birth Control Methods
Report Published by the Katharine Dexter McCormick Library and the Education Division of Planned Parenthood Federation of America 434 West 33rd Street, New York, NY 10001 212-261-4716 www.plannedparenthood.org Current as of January 2012 A History of Birth Control Methods Contemporary studies show that, out of a list of eight somewhat effective — though not always safe or reasons for having sex, having a baby is the least practical (Riddle, 1992). frequent motivator for most people (Hill, 1997). This seems to have been true for all people at all times. Planned Parenthood is very proud of the historical Ever since the dawn of history, women and men role it continues to play in making safe and effective have wanted to be able to decide when and whether family planning available to women and men around to have a child. Contraceptives have been used in the world — from 1916, when Margaret Sanger one form or another for thousands of years opened the first birth control clinic in America; to throughout human history and even prehistory. In 1950, when Planned Parenthood underwrote the fact, family planning has always been widely initial search for a superlative oral contraceptive; to practiced, even in societies dominated by social, 1965, when Planned Parenthood of Connecticut won political, or religious codes that require people to “be the U.S. Supreme Court victory, Griswold v. fruitful and multiply” — from the era of Pericles in Connecticut (1965), that finally and completely rolled ancient Athens to that of Pope Benedict XVI, today back state and local laws that had outlawed the use (Blundell, 1995; Himes, 1963; Pomeroy, 1975; Wills, of contraception by married couples; to today, when 2000). -

Birth Control
Call 311 for Women’s Healthline Free, confidential information and referrals Birth Control New York City Human Resources Administration Infoline Or visit www.nyc.gov/html/hra/pdf/medicaid-offices.pdf What’s Right for You? Information on public health insurance (including Medicaid) for family planning services Other Resources Planned Parenthood of New York City 212-965-7000 or 1-800-230-PLAN (1-800-230-7526) www.ppnyc.org National Women’s Information Center 1-800-994-WOMAN (1-800-994-9662) www.4woman.gov National Family Planning Reproductive Health Association www.nfprha.org Sexuality Information and Education Council of the United States www.siecus.org TAKE CONTROL The New York City Department of Health and Mental Hygiene Michael R. Bloomberg, Mayor Thomas R. Frieden, M.D., M.P.H., Commissioner nyc.gov/health Contents Why Use Birth Control?................................................. 2 Non-Hormonal Methods Male Condoms............................................................. 4 Female Condoms........................................................... 5 Diaphragms and Cervical Caps............................................. 6 Spermicides................................................................ 7 Copper IUDs (Intrauterine Devices)........................................ 8 Fertility Awareness and Periodic Abstinence............................... 9 Hormonal Methods Birth Control Pills (Oral Contraceptives)...................................10 The Birth Control Patch....................................................12 Vaginal -

Natural Family Planning Fact Sheet
Natural Family Planning Fact Sheet ____________________________________________________________________________ 24-hour Emergency Number/Location WHAT’S INSIDE: SOURCES: What is the natural family planning? Office on Women’s Health Basal body temperature method Calendar Method Birth Control Methods: Frequently Cervical Mucus Method Asked Questions How effective are natural family Fertility Awareness planning methods? Advantages of natural family Centers for Disease Control and planning Prevention Drawbacks of natural family planning Unintended Pregnancy Prevention: Contraception U.S. Department of Health & Human Services 200 Independence Avenue, S.W. Washington, D.C. Oklahoma State Department of Health ODH Form 337 MCH/Perinatal & Reproductive Health Division/Family Planning Program Revised Oct 2014 Office of Population Affairs Natural Family Planning Fact Sheet How effective is natural family planning? Of 100 couples who use natural family planning methods each year, anywhere from 1 to 25 will become pregnant. Natural family planning can be an effective type of birth control if all three methods are used and if all are always used correctly. What is natural family planning? A woman with a normal menstrual cycle has about 8 days a month when she can get pregnant. These include the five days before she ovulates (when an egg is released), the day she ovulates, and about one to two days after ovulation. Natural family planning (sometimes known as fertility awareness or the rhythm method) is an approach to birth control some couples use to predict when these fertile days happen. It involves paying close attention to the menstrual cycle by using methods that include: Basal Body Temperature Method Calendar Method Cervical Mucus Method When all three methods are used together, it is known as the symptothermal method. -

Birth Control Methods
F REQUENTLY ASKED QUESTIONS Q: What are the different types of birth control? Birth Control A: You can choose from many methods of birth control. They are grouped by how Methods they work: Types of Birth Control Q: What is the best method of Continuous Abstinence birth control (or contraception)? Natural Family Planning/ http://www.womenshealth.gov A: There is no “best” method of birth control. Each method has its pros and Rhythm Method 1-800-994-9662 cons. Barrier Methods TDD: 1-888-220-5446 All women and men can have control • Contraceptive Sponge over when, and if, they become parents. • Diaphragm, Cervical Cap, and Making choices about birth control, Cervical Shield or contraception, isn’t easy. There are many things to think about. To get • Female Condom started, learn about birth control meth- • Male Condom ods you or your partner can use to pre- Hormonal Methods vent pregnancy. You can also talk with • Oral Contraceptives — Combined your doctor about the choices. pill (“The pill”) Before choosing a birth control meth- • Oral Contraceptives — Progestin- od, think about: only pill (“Mini-pill”) • Your overall health • The Patch • How often you have sex • Shot/Injection • The number of sex partners you • Vaginal Ring have Implantable Devices • If you want to have children some- • Implantable Rods day • Intrauterine Devices • How well each method works to prevent pregnancy Permanent Birth Control Methods • Possible side effects • Sterilization Implant • Your comfort level with using the method • Surgical Sterilization Keep in mind, even the most effective Emergency Contraception birth control methods can fail. But your chances of getting pregnant are lowest if the method you choose always is used correctly and every time you have sex. -

6. Aftercare and Contraception
6. AFTERCARE AND CONTRACEPTION This chapter will help you to provide routine aftercare and contraception following first trimester uterine aspiration. CHAPTER LEARNING OBJECTIVES Following completion of this chapter, you should be better able to: □ Appropriately prescribe post-procedure medications. □ Provide post-procedure counseling, including instructions about home care, warning signs for complications, and emergency contact information. □ Describe post-aspiration contraceptive options and contraindications to specific methods. READINGS / RESOURCES □ National Abortion Federation (NAF). Management of Unintended and Abnormal Pregnancy (Paul M. et al, Wiley-Blackwell, 2009) • Chapter 14: Contraception and surgical abortion aftercare □ Useful handouts for physicians and patients: • Reproductive Health Access Project: www.reproductiveaccess.org • RHEDI: http://rhedi.org/patients.php □ Related Chapter Content: • Chapter 5: Delayed post-procedure complications • Chapter 7: Medication abortion follow-up visit • Chapter 8: Early pregnancy loss follow-up visit SUMMARY POINTS SKILL • Providing women with instructions for home care, medications, contraception, warning signs for complications, and emergency contact information may help minimize patient stress, phone calls, and the need for a routine follow-up appointment following aspiration. • A critical component of abortion care involves contraceptive counseling, method selection, and timing of initiation. SAFETY • Be familiar with the medical eligibility criteria for safely initiating contraceptive methods for women with medical conditions. ROLE • Women with a history of abortion remain at risk for unintended pregnancy; 47% of procedures are repeat procedures. • Starting contraception on the day of uterine aspiration increases initiation and adherence to the method. • Most women are candidates for long acting reversible contraceptives (LARC, including IUDs and implants), which are highly effective, can be placed the day of aspiration, have no estrogen, and users have lower rates of repeat abortion. -

The Femcap Birth Control Method Information and Instructions
The FemCap Birth Control Method Information and Instructions The FemCap works as a method of birth control by creating a physical barrier against sperm entering the cervix (opening to the uterus). It is a reusable, FDA approved, non-hormonal, and latex-free birth control device. If combined with spermicidal gel placed in the groove on the outside of the cap, it is also a chemical barrier, further decreasing the chance of sperm entering the cervix and uterus causing pregnancy. Women’s Health Specialists provides FemCap fittings and prescriptions in our clinics. FemCaps require a prescription in the United States and then can be ordered from FemCap Inc. Advantages of the FemCap: Disadvantages of the FemCap Controlled by the woman Possible allergies/sensitivity to silicone or Can be inserted up to 40 hours before sex spermicide Does not alter menstrual cycle The cap is reusable Cap is latex-free and hypoallergenic Does not change your body’s natural chemistry Is instantly reversible – when you’re ready to get pregnant just stop using it. Tips for Use: We suggest that you: Practice insertion and check to make sure the cap is covering the cervix. Squatting can make your cervix easier to feel. Check cap placement after intercourse the first few times to make sure it hasn’t slipped off the cervix during intercourse. If this happens you may need a different sized cap. If your partner feels the cap during intercourse, you may want to try a different position. You may want to use emergency contraceptives if the cervical cap was not used or if it slipped off the cervix during intercourse. -
Birth Control and You Version 3
Information from your Patient Aligned Care Team Birth Control and You What is Birth Control? Birth Control or contraception is a method of preventing unwanted pregnancy. Throughout history, women and men have used various methods of contraception. Today, there are many low risk and affordable types of birth control that are available for use. Types of Birth Control The main methods of birth control are: Abstinence, Natural Family Planning, Barrier, Hormonal, Withdrawl, and Surgical removal. See Table 1 below for examples of these methods and how to use them. Abstinence Abstinence is the only 100% effective method that prevents pregnancy. Abstinence is the voluntary refrain from sexual activity. Fertility Awareness This method uses the body’s natural rhythms to help prevent pregnancy. Fertility Awareness does not use any device or medication-it is completely natural. Types of fertility awareness include: calendar/rhythm method, the basal body temperature method, and the cervical mucus method. This method can also be used to help predict a woman’s optimal fertility to help get pregnant. Barrier The barrier method is a physical or chemical type of contraception that functions to stop sperm from fertilizing with a woman’s egg. Women AND men can use barriers to prevent unwanted pregnancy. Hormonal Hormonal methods of contraception are available in many forms (see Table 1.). Hormonal contraceptives contain the hormones estrogen and/or progesterone. They work by: 1) Helping to stop a woman's ovaries from releasing an egg each month 2) Causing the cervical mucus to thicken helping to prevent the sperm to reach and penetrate the egg 3) Thinning the lining of the uterus which reduces the likelihood that a fertilized egg will implant in the uterus wall Withdrawl This method refers to the manual removal of an erect penis from the vagina prior to ejaculation. -

Norplant: the New Scarlet Letter?
Journal of Contemporary Health Law & Policy (1985-2015) Volume 8 Issue 1 Article 15 1992 Norplant: The New Scarlet Letter? Michael T. Flannery Follow this and additional works at: https://scholarship.law.edu/jchlp Recommended Citation Michael T. Flannery, Norplant: The New Scarlet Letter?, 8 J. Contemp. Health L. & Pol'y 201 (1992). Available at: https://scholarship.law.edu/jchlp/vol8/iss1/15 This Essay is brought to you for free and open access by CUA Law Scholarship Repository. It has been accepted for inclusion in Journal of Contemporary Health Law & Policy (1985-2015) by an authorized editor of CUA Law Scholarship Repository. For more information, please contact [email protected]. NORPLANT: THE NEW SCARLET LETTER? Michael T. Flannery* [W]hat is it but to laugh in the faces of our godly magistrates, and make a pride out of what they, worthy gentlemen, meant for a punishment?1 Hester Prynne lived in the eighteenth century in an early New England, Puritan colony and is a character of Nathaniel Hawthorne's classic Ameri- can novel, The Scarlet Letter.2 Darlene Johnson was born in 1964 and pres- ently lives in California.' Except for the decision of Judge Howard Broadman,4 these two women would have nothing in common. However, when Judge Broadman ordered Darlene Johnson to undergo the implanta- tion of Norplant5 to effectuate sterilization,6 the two women then shared a common bond: for the crime they each committed, both were sentenced, in effect, to shame. Hester's crime was adultery; Darlene's crime was child abuse." What is ironic is that in an age when criminals were chained to the * Assistant City Solicitor, Law Department, City of Philadelphia; B.A., The University of Delaware; J.D., The Catholic University of America, The Columbus School of Law. -

Preventive Care Services: Contraception
Preventive Care Services: Contraception Preventive Care Coverage at No Cost to You Effective Jan. 1, 2021 Your health plan may provide certain contraceptive coverage as a benefit of membership, at no cost to you when you use a pharmacy or doctor in your health plan's network. There is no copay, deductible or coinsurance, even if your deductible or out-of-pocket maximum has not been met. Coverage for contraceptives can vary depending on the type of plan you are enrolled in, as well as your prescription drug list. If you are using a contraceptive not listed under the Contraceptive Product Coverage, then copays, coinsurance or deductible may apply. Check your drug list or call the number listed on your member ID card to find out what products are covered at no cost share under your plan. Contraception* The following contraceptive items and services may be covered under the medical or pharmacy benefit without cost-sharing when provided by a pharmacy or doctor in your health plan's network. This list is not all inclusive. Additional products may be covered at no additional cost. • One or more prescribed products within each of the categories approved by the FDA for use as a method of contraception • FDA-approved contraceptives available over the counter (i.e. foam, sponge, female condoms), when prescribed by a physician • The morning after pill • Injections such as IM DEPO-PROVERA and DEPO-SUBQ PROVERA 104 may be covered under the medical or pharmacy benefit • Medical devices such as diaphragms, cervical caps and contraceptive implants may -

ESTROSTEP Fe (Norethindrone Acetate and Ethinyl Estradiol Tablets, USP and Ferrous Fumarate Tablets*) *Ferrous Fumarate Tablets Are Not USP for Dissolution and Assay
ESTROSTEP Fe (Norethindrone Acetate and Ethinyl Estradiol Tablets, USP and Ferrous Fumarate Tablets*) *Ferrous fumarate tablets are not USP for dissolution and assay. ESTROSTEP® Fe (Each white triangular tablet contains 1 mg norethindrone acetate and 20 mcg ethinyl estradiol; each white square tablet contains 1 mg norethindrone acetate and 30 mcg ethinyl estradiol; each white round tablet contains 1 mg norethindrone acetate and 35 mcg ethinyl estradiol; each brown tablet contains 75 mg ferrous fumarate.) Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases. DESCRIPTION ESTROSTEP® Fe is a graduated estrophasic oral contraceptive providing estrogen in a graduated sequence over a 21-day period with a constant dose of progestogen. ESTROSTEP Fe provides for a continuous dosage regimen consisting of 21 oral contraceptive tablets and seven ferrous fumarate tablets. The ferrous fumarate tablets are present to facilitate ease of drug administration via a 28-day regimen, are non-hormonal, and do not serve any therapeutic purpose. Each white triangle-shaped tablet contains 1 mg norethindrone acetate [(17 alpha)-17 (acetyloxy)-19-norpregna-4-en-20-yn-3-one] and 20 mcg ethinyl estradiol [(17 alpha)-19 norpregna-1,3,5(10)-trien-20-yne-3,17-diol]; each white square-shaped tablet contains 1 mg norethindrone acetate and 30 mcg ethinyl estradiol; and each white round tablet contains 1 mg norethindrone acetate and 35 mcg ethinyl estradiol. Each tablet also contains calcium stearate; lactose; microcrystalline cellulose; and starch. The structural formulas are as follows: Each brown tablet contains ferrous fumarate, mannitol, povidone, microcrystalline cellulose, sodium starch glycolate, magnesium stearate, sucralose and spearmint flavor. -

An Abortion Story from Both Sides of the Exam Table
Original article found online at: http://www.refinery29.com/my-story-on-both-sides-of-the- exam-table An Abortion Story From Both Sides Of The Exam Table Illustrated by Mary Galloway. Written by Debbie Bamberger, from her story "My Story From Both Sides Of The Exam Table". When I was 19 and a sophomore in college in Worcester, Massachusetts, I responded to an ad in the local paper for phone volunteers at Planned Parenthood. I already had an affinity for Planned Parenthood. My mother’s life story included a visit to the Margaret Sanger Clinic in Manhattan at 19 to get a diaphragm — she was having sex with her boyfriend — and I had gone to Planned Parenthood to get a diaphragm myself in my hometown of Poughkeepsie when I was still in high school. Volunteering at my local clinic was a life-changing experience for me. I met women working there who opened my eyes to sexism and misogyny. I loved speaking on the phone to women seeking an abortion, providing help to them, and I appreciated the easy availability of birth control and emergency contraception. I knew how to prevent pregnancy and wanted to, but I was also more careless in college than I had been in high school. I haven't thought too much about my reasons for this, but I may have been testing myself and my fertility, or I may have felt cocky about the ability to have an abortion if I needed one. I had a lot of sex and took emergency contraception many times, back at a time when that meant a huge dose of regular birth control pills and subsequent nausea. -
Barrier Methods How Barrier Methods Work Barrier Methods Create a Barrier, Either Physical Or Chemical, That Prevents Sperm from Reaching the Egg
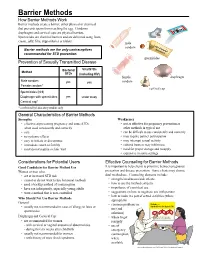
Barrier Methods How Barrier Methods Work Barrier methods create a barrier, either physical or chemical, that prevents sperm from reaching the egg. Condoms, diaphragms and cervical caps are physical barriers. Spermicides are chemical barriers and are delivered using foam, cream, jelly, film, suppositories or tablets. male condom Barrier methods are the only contraceptives recommended for STD prevention. spermicides Prevention of Sexually Transmitted Disease Bacterial Viral STDs Method STDs (including HIV) female diaphragm Male condom yes yes condom Female condom* cervical cap Spermicides (N-9) Diaphragm with spermicides yes under study Cervical cap* * confimred by laboratory studies only General Characteristics of Barrier Methods Strengths Weaknesses • effective at preventing pregnancy and some STDs • not as effective for pregnancy prevention as when used consistently and correctly other methods in typical use • safe • can be difficult to use consistently and correctly • no systemic effects • may require partner participation • easy to initiate or discontinue • may interrupt sexual activity • immediate return to fertility • cultural barriers may inhibit use • most do not require a clinic visit • need for proper storage and resupply • expensive in some settings Considerations for Potential Users Effective Counseling for Barrier Methods Good Candidates for Barrier Method Use It is important to help clients to prioritize between pregnancy Women or men who: prevention and disease prevention. Some clients may choose • are at increased STD risk