USCS Data Visualizations Tool Technical Notes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How the House of Morgan Cooperated to Develop the Large-Cap US Multinational Corporation, 1895-1913
How the House of Morgan Cooperated to Develop the Large-Cap US Multinational Corporation, 1895-1913 The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Sawe, Joseph. 2015. How the House of Morgan Cooperated to Develop the Large-Cap US Multinational Corporation, 1895-1913. Master's thesis, Harvard Extension School. Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:24078367 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA ! How the House of Morgan Cooperated to Develop the Large-Cap US Multinational Corporation, 1895-1913 Joseph Sawe A Thesis in the Field of International Relations for the Degree of Master of Liberal Arts in Extension Studies Harvard University November 2015 ! ! ! ! ! ! Abstract The following investigation is intended to determine how the large-cap US multinational corporation was further advanced during the pivotal years of 1895-1913 by a leading private unincorporated institution—House of Morgan. Historical review and assessment focused on the broader US society, government, monetary landscape, the House of Morgan, leading large cap US multinationals; looking at both the key organizations and underlying people in power. The report framework focuses upon the development of the US super structure within which all major companies work down to the way actual institutions organize economic assets in the form of a multinational corporation. Questions that have been considered include: how was business conducted globally with so little formal mechanisms in place, the importance of the various forms of capital for business, and the various roles politics played in business development. -
African Americans Have Been a Part of the Diverse Population of South Sound Since American Settlers Arrived in 1845. However
African Americans have been a part the Frost Family Plot. “Henrietta,” of the diverse population of South domestic servant for Elisha Ferry Sound since American settlers who later became governor of arrived in 1845. However, records Washington, only appears once in regarding early African Americans Olympia’s census. Leander Bushon’s in the Olympia area are scant. The apparent business success beyond fragments of stories that survive Olympia after apprenticing in offer a window into the daily life Samuel Stork’s mercantile remains of Washington’s Capital City and to be researched. The women of environs. Most came of their own color identified as prostitutes in accord, looking for a place to improve the census disappear as abruptly as their chances for a better life. They they appear in local records. Yet worked as laborers, domestic all of their stories show the South servants, or as stewards on Puget Sound’s population is more complex Sound’s “Mosquito Fleet” steamboats. and interconnected than many early Others became business owners, histories indicate. worked as restaurateurs, barbers or bootblacks. Despite their struggles While few structures associated against discrimination, they made with their lives survive, the stories their homes here and were an connected to these sites reflect integral part of the social fabric. the diversity of experiences that This brochure will introduce you to make up African American history in some of these people. Olympia and the Pacific Northwest. Thomas Park, a brick mason by In some cases first names are used trade, was a lifelong associate of the to avoid confusion with relatives of Robert Frost Family and is buried in the same last name. -

Landscape Medallion in Washington State
Architect of the Capitol Landscape medallion (detail), Brumidi Corridors. Brumidi’s landscape medallions relate to the federally sponsored Pacific Railroad Report and depict scenes from the American West, such as this view of Mount Baker in Washington State. The “MostBrumidi’s Landscapes andPracticable the Transcontinental Railroad ”Route Amy Elizabeth Burton or 150 years, senators, dignitaries, and visitors to the U.S. Capitol have bustled past 8 Flandscape medallions prominently located in the reception area of the Brumidi Corridors on the first floor of the Senate wing. For most of this time, very little was understood about these scenes of rivers and mountains. The locations depicted in the landscapes and any relevance the paintings once held had long faded from memory. The art of the Capitol is deeply rooted in symbolism and themes that reflect national pride, which strongly suggested that the medallions’ significance extended beyond their decorative value. Ultimately, a breakthrough in scholarship identified the long-forgotten source of the eight landscapes and reconnected them to their his- torical context: a young nation exploring and uniting a vast continent, as well as a great national issue that was part of this American narrative—the first transcontinental railroad. THE “MOST PRACTICABLE” ROUTE 53 Starting in 1857, the Brumidi Corridors in the newly con- From roughly 1857 to 1861, Brumidi and his team structed Senate wing of the Capitol buzzed with artistic of artists decorated the expansive Brumidi Corridors activity. Development of the mural designs for the Sen- with Brumidi’s designs, while one floor above, the Senate ate’s lobbies and halls fell to artist Constantino Brumidi, deliberated about the building of the nation’s first trans- under the watchful eye of Montgomery C. -

How to Cite Complete Issue More Information About This
Diálogos Revista Electrónica de Historia ISSN: 1409-469X Escuela de Historia. Universidad de Costa Rica León, Jorge Nineteenth Century Navies’ Role in developing an understanding of The Pacific Coast Of Central America (1730-1900)/1 Diálogos Revista Electrónica de Historia, vol. 19, no. 2, 2018, July-December, pp. 58-100 Escuela de Historia. Universidad de Costa Rica DOI: 10.15517/dre.v19i2.33352 Available in: http://www.redalyc.org/articulo.oa?id=43956436003 How to cite Complete issue Scientific Information System Redalyc More information about this article Network of Scientific Journals from Latin America and the Caribbean, Spain and Journal's webpage in redalyc.org Portugal Project academic non-profit, developed under the open access initiative NINETEENTH CENTURY NAVIES’ ROLE IN DEVELOPING AN UNDERSTANDING OF THE PACIFIC COAST OF CENTRAL AMERICA (1730-1900)1 Jorge León Resumen A inicios del siglo XIX, los conocimientos sobre la navegación en la costa del Pacífico de América eran escasos. Antes de 1800, las principales fuentes de información náutica fueron los derroteros españoles. Entre 1808 y 1826, los intereses marítimos y comerciales ingleses, sustituyeron a los de España en la región. Los barcos británicos que comerciaban por la costa, necesitaban de mejores cartas marinas y derroteros, lo cual llevó a la Marina Real a asumir la tarea de levantar cartas marinas. A partir de mediados de los años 1830, el Almirantazgo inglés se convirtió en la principal fuente de información náutica. Más tarde las marinas de Francia y de los Estados Unidos se unieron a esta labor de levantar cartas de los puertos del Pacífico. -
History of the Pacific Islands Studies Program at the University of Hawaii: 1950-198
HISTORY OF THE PACIFIC ISLANDS STUDIES PROGRAM AT THE UNIVERSITY OF HAWAII: 1950-198 by AGNES QUIGG Workinq Paper Series Pacific Islands Studies Program canters for Asian cmd Pacific Studies University of Hawaii at Manoa EDITOR'S OOTE The Pacific Islands Studies Program. often referred to as PIP, at the University of Hawaii had its beginnings in 1950. These were pre-statehood days. The university was still a small territorial institution (statehood came in 1959), and it is an understatement to say that the program had very humble origins. Subsequently, it has had a very checkered history and has gone through several distinct phases. These and the program's overall history are clearly described and well analyzed by Ms. Agnes Quigg. This working paper was originally submitted by Ms. Quigg as her M.A. thesis in Pacific Islands Studies. Ms. Quigg' is a librarian in the serials division. Hamnlton Library, University of Hawaii. Earlier in this decade, she played a crucial role in the organization of the microfilming of the archives of the U.S. Trust Territory of the Pacific Islands, Office of the High CommiSSioner, Saipan, Northern Marianas. The archives are now on file at Hamilton Library. Formerly, Ms. Quigg was a librarian for the Kamehameha Schools in Honolulu. R. C. Kiste Director Center for Pacific Islands Studies THE HISTORY OF THE PACIFIC ISLANDS STUDIES PROGRAM AT THE UNIVERSITY OF HAWAII: 1950-1986 By Agnes Quigg 1987 ii ACKNOWLEDGEMENTS I am indebted to a number of people who have helped me to complete my story. Judith Hamnett aided immeasurably in my knowledge of the early years of PIP, when she graciously turned over her work covering PIP's first decade. -

Attachment A
Attachment K: List of Documents and Sources Maytown Land Use Evaluation: Documents and Sources Reviewed Documents and studies reviewed for this amendment include but are not limited to the following: 1. 971854 SUPT, Prairie Green Golf Course. 1997. Case File. Thurston County. Olympia, WA. 2. 971855 SUPT, Prairie Green Country Inn. 1997. Case File. Thurston County. Olympia, WA. 3. 020612 SUPT, Allen & Company LLC, Maytown Aggregates. 2005. Case File. Thurston County. Olympia, WA. 4. Beier, P., and R. F. Noss. 1998. Do habitat corridors provide connectivity? Conservation Biology 12:1241-1252. Available: http://oak.ucc.nau.edu/pb1/vitae/Beier-Noss_1998.pdf 5. Century Pacific, L.P. 2009. Maytown Development Property Thurston County, WA Offering Memorandum. Seattle, WA. 17 pp. 6. Dunn, P., and Ewing, K. editors. 1997. Ecology and conservation of the south Puget Sound prairie landscape. The Nature Conservancy, Seattle. 289 pp. 7. Ellis, David V. Nov. 17, 2005. Archaeological survey, Proposed Maytown Aggregates Development AINW Report No. 1584. Portland, OR. 8. Fall Creek Environmental, Inc. 1996. Wetland Delineation and Analysis Report for the Pacific Powder Site Thurston County, WA. T-96-063 Thurston County Case File. Longview, WA. 9. Germiat, Steve J. March 2006. Environmental Characterization Report for Area Proposed for Removal From Site Former Pacific Powder Site, Maytown Washington. Aspect Consulting. Seattle, WA. http://www.ecy.wa.gov/programs/TCP/sites/citifor/citifor_3-6-06.pdf 10. Larsen, E. 1995. Management Recommendations for Washington’s Priority Species Volume I: Invertebrates. Washington Department of Fish and Wildlife, Olympia. 87 pp. 11. Larsen, E. M., and J. T. -

Atlantic Salmon, Pacific Bound: Initiative, Defiance, Courage, and Indian Tribes in Environmenal Law William H
Ocean and Coastal Law Journal Volume 8 | Number 1 Article 2 2002 Atlantic Salmon, Pacific Bound: Initiative, Defiance, Courage, And Indian Tribes In Environmenal Law William H. Rodgers, Jr. Follow this and additional works at: http://digitalcommons.mainelaw.maine.edu/oclj Recommended Citation William H. Rodgers, Jr., Atlantic Salmon, Pacific Bound: Initiative, Defiance, Courage, And Indian Tribes In Environmenal Law, 8 Ocean & Coastal L.J. (2002). Available at: http://digitalcommons.mainelaw.maine.edu/oclj/vol8/iss1/2 This Lecture is brought to you for free and open access by the Journals at University of Maine School of Law Digital Commons. It has been accepted for inclusion in Ocean and Coastal Law Journal by an authorized administrator of University of Maine School of Law Digital Commons. For more information, please contact [email protected]. ATLANTIC SALMON, PACIFIC BOUND: INITIATIVE, DEFIANCE, COURAGE, AND INDIAN TRIBES IN ENVIRONMENTAL LAW William H. Rodgers, Jr I. INTRODUCTION It is an honor to deliver this lecture at the University of Maine School of Law, as the Edward S. Godfrey Visiting Professor of Law.' My visit here has been filled with wonder and excitement. My new colleagues have been splendidly supportive, and the students a delight to work with. I would like to give a special word of thanks to Dean Colleen Khoury who has done much to welcome this stranger into the mysteries of Maine; and to Dean Edward S. Godfrey, who has been a special inspiration to me as he has to literally every graduate of the law school here in Maine. I want to address my remarks to the students of this law school who will face a great deal of unfinished legal business on the topics of salmon, Indian tribes, and environmental law. -

Asian Americans and Pacific Islanders in California, 1850-1970 MPS
UNITED STATES DEPARTMENT OF THE INTERIOR NATIONAL PARK SERVICE NATIONAL REGISTER OF HISTORIC PLACES EVALUATION/RETURN SHEET Requested Action: COVER DOCUMENTATION Multiple Name: Asian Americans and Pacific Islanders in California, 1850-1970 MPS State & County: CALIFORNIA, San Francisco Date Received: Date of 45th Day: 11/29/2019 1/13/2020 Reference MC100004867 number: Reason For Review: Checkbox: Unchecked Appeal Checkbox:PDIL Unchecked Checkbox:Text/Data Issue Unchecked Checkbox: Unchecked SHPO Request LandscapeCheckbox: Unchecked PhotoCheckbox: Unchecked Checkbox: Unchecked Waiver Checkbox:National Unchecked Checkbox:Map/Boundary Unchecked Checkbox: Unchecked Resubmission Checkbox:Mobile Resource Unchecked PeriodCheckbox: Unchecked Checkbox:Other Unchecked Checkbox:TCP Unchecked Checkbox:Less than 50 Unchecked years CLGCheckbox: Unchecked Checkbox: Checked Accept ReturnCheckbox: Unchecked Checkbox:Reject Unchecked 1/10/2020 Date Abstract/Summary The Asian Americans and Pacific Islanders in California, 1850-1970 MPS cover document is Comments: an excellent resource for the evaluation, documentation and designation of historic ethnic resources in California. The MPS develops three fairly comprehensive thematic contexts and provides registration guidelines for several general and specific property types including historic districts, agricultural properties, industrial sites, community service properties, religious properties and properties associated with significant individuals. Additional contexts, time periods, and associated property types may be developed at a later date. NPS grant funded project. Recommendation/ Accept MPS Cover Documentation Criteria Reviewer Paul Lusignan Discipline Historian Telephone (202)354-2229 Date 1/10/2020 DOCUMENTATION: see attached comments: No see attached SLR: Yes If a nomination is returned to the nomination authority, the nomination is no longer under consideration by the National Park Service. NPS Form 10-900-a (Rev. -
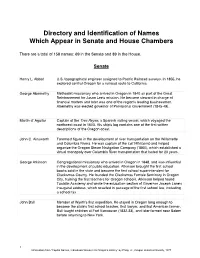
Inscribed Names in the Senate and House Chambers
Directory and Identification of Names Which Appear in Senate and House Chambers There are a total of 158 names: 69 in the Senate and 89 in the House. Senate Henry L. Abbot U.S. topographical engineer assigned to Pacific Railroad surveys. In 1855, he explored central Oregon for a railroad route to California. George Abernethy Methodist missionary who arrived in Oregon in 1840 as part of the Great Reinforcement for Jason Lee's mission. He became steward in charge of financial matters and later was one of the region's leading businessmen. Abernethy was elected governor of Provisional Government (1845-49). Martin d’ Aguilar Captain of the Tres Reyes, a Spanish sailing vessel, which voyaged the northwest coast in 1603. His ship's log contains one of the first written descriptions of the Oregon coast. John C. Ainsworth Foremost figure in the development of river transportation on the Willamette and Columbia Rivers. He was captain of the Lot Whitcomb and helped organize the Oregon Steam Navigation Company (1860), which established a virtual monopoly over Columbia River transportation that lasted for 20 years. George Atkinson Congregational missionary who arrived in Oregon in 1848, and was influential in the development of public education. Atkinson brought the first school books sold in the state and became the first school superintendent for Clackamas County. He founded the Clackamas Female Seminary in Oregon City, training the first teachers for Oregon schools. Atkinson helped found Tualatin Academy and wrote the education section of Governor Joseph Lane's inaugural address, which resulted in passage of the first school law, including a school tax. -

Asian and Pacific Islander Americans in Congress 1900–2017 H Introduction H
Asian and Pacific Islander Americans in Congress 1900–2017 H introduction H On December 15, 1900, two weeks into the second session of the 56th Congress (1899–1901) of the United States, one of the early Hispanic Members of Congress, Delegate Pedro Perea of New Mexico, escorted a tall man with a handlebar moustache into the well of the U.S. House of Representatives. Facing the marble rostrum, Robert W. Wilcox, the son of a New England sea captain and a Native-Hawaiian mother, took the oath of office as the first Delegate from the Territory of Hawaii. Wilcox, along with his wife, two children, and an aide, had just arrived that morning in Washington, DC, after a long transcontinental train trip. Quickly surrounded by well-wishers, the first Asian Pacific American (APA) Member of Congress and, in fact, the first individual to represent a constituency outside the continental United States, set to work.1 During the course of the next century, another 59 individuals of Asian or Pacific Islander ancestry followed Delegate Wilcox into the U.S. Congress.2 Their saga spans vast distances, stretching from Manila in the faraway Philippine archipelago to Capitol Hill in Washington, DC. Rooted in U.S. expansion into the Pacific Ocean, the story of APAs in Congress also was influenced by successive waves of immigrants and refugees who arrived on American shores. What follows is the story of how APAs moved from almost complete exclusion and marginalization to a rising influence at the center of American government. This certificate of election from 1900 formalizes Robert W. -
The New York and the Josephine: Two Steamships of the Charles
The New York and the Josephine: whose energy, "can-do" attitude, Two Steamships of the forcefulness and, sometimes, Charles Morgan Line ruthlessness came to symbolize the American spirit. Men such as Cornelius Jack B. Irion and David A. Ball Vanderbilt and Jay Gould drove the American economy and decided America's economic future. Such a man Introduction also, was Charles Morgan, whose During much of the 19th century, New influence on the process of resource Orleans, the "Queen of the South," vied allocation and economic development with northern cities such as Boston for can still be felt in the Gulf South over the spot behind New York as the second 100 years later. busiest port in the United States. It can be argued that the Crescent City rode to Charles Morgan this distinction on a cloud of steam since One of the foremost figures in the it was only after the introduction of the development of the steamship trade steamboat in Louisiana waters in 1811 along the Gulf Coast of the United States that vessels could easily stem the current was not a Southerner at all, but a New of the Mississippi to reach the city's York businessman, Charles Morgan wharves over 95 miles from the river's (Figure 1). Morgan was born in mouth. Prior to that, the major water route into the city followed shallow water passages through the Rigolets into Lake Pontchartrain and down Bayou St. John to the Mississippi River. With the introduction of the steam engine, vessels could travel directly from the Gulf of Mexico up the deep channel of the Mississippi to the very front door of the city, drastically reducing the time required by sail. -
HISTORICAL SITES and SHIPWRECKS ALONG the SACRAMENTO RIVER Between Sacramento City and Sherman Island
A Map and Record Investigation of HISTORICAL SITES AND SHIPWRECKS ALONG THE SACRAMENTO RIVER Between Sacramento City and Sherman Island 7G.9f/Tc. 'S.J..516.., Ca,fhenne ..MO.sher et .-l 76.99'/lc. 'I J :( .' ,,,1 ' ' -~ "''°\\ ·.;t,...O _,,,o. , ~\ 1'' A Map and Record Investigation of HISTORICAL SITES AND SHIPWRECKS ALONG THE SACRAMENTO RIVER Between Sacramento City and Sherman Island Prepared by Land Location and Boundary Section on the staff of the California State Lands Commission Until this material is reviewed and approved by the Executive Officer of the California State Lands Commission, it is to be considered as tentative and subject to revision. February 29, 1988 LEGISLATIVE CHARGE As part of the 1985/86 budget, the State Lands Commission was requested to locate, document, and investigate the significant ships and artifacts from California's rich historical heritage along the Sacramento River. In general, we were charged with: • Inventorying, mapping, and cataloging all known points of historical significance along the River, including ports, wharves, piers villages, and ship sinkings. • Preparing costs estimates for an electronic survey using magnetometers, side-scan sonars, and sub-bottom profilers for the purpose of locating historic ships and artifacts. • Preparing cost estimates of a program of field verification of selected locations. • Considering contracting all or part of the study with "outside entities" and shall consider contracting for consulting services with the State Historic Preservation Office. An exact copy of the authorizing budget item is included in this report. See the table of contents for the page. 1ll ROSTER OF STAFF WHO CONTRIBUTED TO THIS REPORT This report has no single author.