Victorian Aboriginal Children and Young People's Alliance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chapter 8. Aboriginal Water Values and Uses
Chapter 8. Aboriginal water values and uses Department of Environment, Land, Water and Planning 8. Aboriginal water values and uses The Murray-Darling Basin Plan requires Basin states to identify objectives and outcomes of water, based on Aboriginal values and uses of water, and have regard to the views of Traditional Owners on matters identified by the Basin Plan. Victoria engaged with Traditional Owner groups in the Water Resource Plan for the northern Victoria area to: • outline the purpose, scope and opportunity for providing water to meet Traditional Owner water objectives and outcomes through the Murray-Darling Basin Plan • define the role of the water resource plans in the Basin, including but not limited to the requirements of the Basin Plan (Chapter 10, Part 14) • provide the timeline for the development and accreditation of the Northern Victoria Water Resource Plan • determine each Traditional Owner group’s preferred means of engagement and involvement in the development of the Northern Victoria Water Resource Plan • continue to liaise and collaborate with Traditional Owner groups to integrate specific concerns and opportunities regarding the water planning and management framework. • identify Aboriginal water objectives for each Traditional Owner group, and desired outcomes The Water Resource Plan for the Northern Victoria water resource plan area, the Victorian Murray water resource plan area and the Goulburn-Murray water resource plan area is formally titled Victoria’s North and Murray Water Resource Plan for the purposes of accreditation. When engaging with Traditional Owners this plan has been referred to as the Northern Victoria Water Resource Plan and is so called in Chapter 8 of the Comprehensive Report. -
Click Here to View Asset
Published by Arts Victoria. The views expressed in this publication are based on information provided by third party authors. Arts Victoria does not necessarily endorse the views of a particular author. All information contained in this publication is considered correct at the time of printing. Arts Victoria VIAA PRE -SELECTION PANEL EXHIBITION CURATORS , Private Bag No. 1 Maree Clarke, Curatorial Manager, DESIGN AND HANGING South Melbourne 3205 Koorie Heritage Trust; Stephen Boscia Galleries Victoria Australia Gilchrist, Curator – Indigenous Art, PHOTOGRAPHY TELEPHONE 03 9954 5000 National Gallery of Victoria; Jirra Harvey, Freelance Curator. Ponch Hawkes FACSIMILE 03 9686 6186 CATALOGUE DESIGN TTY 03 9682 4864 VIAA FINAL JUDGING PANEL AND SPONSORS Actual Size TOLL FREE 1800 134 894 Lorraine Coutts, Indigenous Curator; (Regional Victoria only) Kevin Williams, Indigenous artist; PRINTED BY [email protected] Zara Stanhope, freelance Curator; Gunn and Taylor Printers www.arts.vic.gov.au Stephen Gilchrist, Curator – Indigenous Art, National Gallery The VIAA exhibition runs from of Victoria; Judith Ryan, Senior 29 November to 20 December Curator – Indigenous Art, National 2008, Boscia Galleries, Melbourne Gallery of Victoria; Jason Eades, Victoria, 3000. CEO – Koorie Heritage Trust; Nerissa The exhibition is free and open to Broben, Curatorial Manager – Koorie the public. Heritage Trust; Chris Keeler, Curatorial Assistant – Koorie Artworks featured in the VIAA Heritage Trust. exhibition are available for purchase. This publication is copyright. No part SPONSORS ’ REPRESENTATIVES Michele and Anthony Boscia, may be reproduced by any process Boscia Galleries. except in accordance with provisions of the Copyright Act 1968. Thank you to all the artists who entered the awards. -
Yuranga Aboriginal Network Mildura Local Aboriginal Network
YURANGA ABORIGINAL NETWORK MILDURA LOCAL ABORIGINAL NETWORK COMMUNITY PLAN 2020 OFFICIAL ACKNOWLEDGEMENT AND RESPECT TELKI NGAWINGI (Latji Latji for Good Day) We would like to take this opportunity to acknowledge the traditional owners of this Country and the Elders who have passed into the Dreaming and Elders present today who have survived the impacts of Colonisation. Our Elders are the Cornerstone of our communities and we pay our Respect to them, their journeys, their strength and their Resilience. If it were not for them, we would not be here. OFFICIAL The Yuranga Local Aboriginal Network in Mildura was established in 2008, as part of the then Victorian Government’s New Representative Arrangement for Aboriginal People living in Victoria. The LAN’s original Community Plan was Titled: “The Mildura Local Indigenous Network – The Yuranga Aboriginal Committee, Community Plan.” It’s overarching framework was the VIAF of the time. Local Aboriginal Networks (LANs) bring Aboriginal people together to set priorities develop community plans and improve social connection. Our Mildura LAN has an Aboriginal name, which means “bend in the river.” The LAN in Mildura has been active within the Mildura community and over the years has held a number of Projects and supported others, however we have worked with the local Mildura Rural City Council and have produced a video that sits on the AV Website. MRCC have endorsed our Community Plan and it also sits on their Website along with all of the Geographical Community Plans, as the Municipality’s first Cultural Plan. Our LAN now has approximately 212 participants and there are 39 LANs in the State of Victoria. -
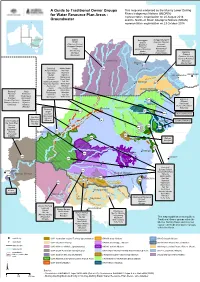
A Guide to Traditional Owner Groups For
A Guide to Traditional Owner Groups Th is m ap w as e nd orse d by th e Murray Low e r Darling Rive rs Ind ige nous Nations (MLDRIN) for Water Resource Plan Areas - re pre se ntative organisation on 20 August 2018 Groundwater and th e North e rn Basin Aboriginal Nations (NBAN) re pre se ntative organisation on 23 Octobe r 2018 Bidjara Barunggam Gunggari/Kungarri Budjiti Bidjara Guwamu (Kooma) Guwamu (Kooma) Bigambul Jarowair Gunggari/Kungarri Euahlayi Kambuwal Kunja Gomeroi/Kamilaroi Mandandanji Mandandanji Murrawarri Giabel Bigambul Mardigan Githabul Wakka Wakka Murrawarri Githabul Guwamu (Kooma) M Gomeroi/Kamilaroi a r a Kambuwal !(Charleville n o Ro!(ma Mandandanji a GW21 R i «¬ v Barkandji Mutthi Mutthi GW22 e ne R r i i «¬ am ver Barapa Barapa Nari Nari d on Bigambul Ngarabal C BRISBANE Budjiti Ngemba k r e Toowoomba )" e !( Euahlayi Ngiyampaa e v r er i ie Riv C oon Githabul Nyeri Nyeri R M e o r Gomeroi/Kamilaroi Tati Tati n o e i St George r !( v b GW19 i Guwamu (Kooma) Wadi Wadi a e P R «¬ Kambuwal Wailwan N o Wemba Wemba g Kunja e r r e !( Kwiambul Weki Weki r iv Goondiwindi a R Barkandji Kunja e GW18 Maljangapa Wiradjuri W n r on ¬ Bigambul e « Kwiambul l Maraura Yita Yita v a r i B ve Budjiti Maljangapa R i Murrawarri Yorta Yorta a R Euahlayi o n M Murrawarri g a a l rr GW15 c Bigambul Gomeroi/Kamilaroi Ngarabal u a int C N «¬!( yre Githabul R Guwamu (Kooma) Ngemba iv er Kambuwal Kambuwal Wailwan N MoreeG am w Gomeroi/Kamilaroi Wiradjuri o yd Barwon River i R ir R Kwiambul !(Bourke iv iv Barkandji e er GW13 C r GW14 Budjiti -

Groundwater) Groundwater Water Resource Plan Area Nations Groundwater Water Resource Plan Area Nations GW1 Ngunnawal/Ngunawal GW11 Cont
A Guide to Traditional Owner Groups for Water Resource Plan Areas (Groundwater) Groundwater Water Resource Plan Area Nations Groundwater Water Resource Plan Area Nations GW1 Ngunnawal/Ngunawal GW11 cont. Kunja Australian Capital Territory (groundwater) Wolgalu Kwiambul Ngambri Maljangapa Ngarigu Maraura GW2 Dhudhuroa Murrawarri Goulburn-Murray Dja Dja Wurrung Mutthi Mutthi Taungurung Nari Nari Waywurru Ngarabal Yaithmathang Ngemba Yorta Yorta Ngiyampaa GW3 Dja Dja Wurrung Nyeri Nyeri Wimmera-Mallee (groundwater) Latji Latji Tati Tati Ngintait Wadi Wadi Tati Tati Wailwan Wemba Wemba Wemba Wemba Watjobaluk Weki Weki Wergaia Wiradjuri GW4 First Peoples of the South East Yita Yita South Australian Murray Region Maraura Yorta Yorta Ngaduri GW12 Wailwan Ngarrindjeri Macquarie-Castlereagh Alluvium Wiradjuri Ngintait G13 Barkandji Peramangk NSW Great Artesian Basin Shallow Bigambul RMMAC Budjiti GW5 Kaurna Euahlayi Eastern Mount Lofty Ranges Peramangk Gomeroi/Kamilaroi GW6 Barkandji Guwamu (Kooma) NSW Murray-Darling Basin Porous Rock Barapa Barapa Kambuwal Gomeroi/Kamilaroi Kunja Maraura Kwiambul Mutthi Mutthi Maljangapa Nari Nari Murrawarri Ngarabal Ngarabal Ngiyampaa Ngemba Nyeri Nyeri Wailwan Tati Tati Wiradjuri Wadi Wadi GW14 Namoi Alluvium Gomeroi/Kamilaroi Wemba Wemba GW15 Gwydir Alluvium Gomeroi/Kamilaroi Weki Weki GW18 Bigambul Wiradjuri NSW Border Rivers Alluvium Githabul Yorta Yorta Kambuwal GW7 Barkandji Gomeroi/Kamilaroi Darling Alluvium Budjiti Kwiambul Euahlayi GW19 Bigambul Murrawarri Queensland Border Rivers - Moonie Githabul -
Indigenous Knowledge in the Built Environment a Guide for Tertiary Educators
Indigenous Knowledge in The Built Environment A Guide for Tertiary Educators David S Jones, Darryl Low Choy, Richard Tucker, Scott Heyes, Grant Revell & Susan Bird Support for the production of this publication has been 2018 provided by the Australian Government Department of Education and Training. The views expressed in this report do ISBN not necessarily reflect the views of the Australian Government 978-1-76051-164-7 [PRINT], Department of Education and Training. 978-1-76051-165-4 [PDF], With the exception of the Commonwealth Coat of Arms, and 978-1-76051-166-1 [DOCX] where otherwise noted, all material presented in this document is provided under Creative Commons Attribution-ShareAlike 4.0 Citation: International License http://creativecommons.org/licenses/ Jones, DS, D Low Choy, R Tucker, SA Heyes, G Revell & S Bird by-sa/4.0/ (2018), Indigenous Knowledge in the Built Environment: A Guide The details of the relevant licence conditions are available on for Tertiary Educators. Canberra, ACT: Australian Government the Creative Commons website (accessible using the links Department of Education and Training. provided) as is the full legal code for the Creative Commons Attribution- ShareAlike 4.0 International License http:// Warning: creativecommons.org/licenses/by-sa/4.0/legalcode Aboriginal and Torres Strait Islander readers are warned that the following document may contain images and names of Requests and inquiries concerning these rights should be deceased persons. addressed to: Office for Learning and Teaching A Note on the Project’s Peer Review Process: Department of Education The content of this teaching guide has been independently GPO Box 9880, peer reviewed by five Australian academics that specialise Location code N255EL10 in the teaching of Indigenous knowledge systems within the Sydney NSW 2001 built environment professions, two of which are Aboriginal [email protected] academics and practitioners. -

Traditional Owner Objectives and Outcomes
Traditional Owner objectives and outcomes: Compilation of contributions to Victoria’s water resource plans Photos Cover: Mirring – Country, DELWPs Aboriginal Cultural Identity Artwork credit: Tom Day of the Gunditjmara, Yorta Yorta and Wemba Wemba tribes. Acknowledgment We acknowledge and respect Victorian Traditional Owners as the original custodians of Victoria's land and waters, their unique ability to care for Country and deep spiritual connection to it. We honour Elders past and present whose knowledge and wisdom has ensured the continuation of culture and traditional practices. We are committed to genuinely partner, and meaningfully engage, with Victoria's Traditional Owners and Aboriginal communities to support the protection of Country, the maintenance of spiritual and cultural practices and their broader aspirations in the 21st century and beyond. © The State of Victoria Department of Environment, Land, Water and Planning 2019 This work is licensed under a Creative Commons Attribution 4.0 International licence. You are free to re-use the work under that licence, on the condition that you credit the State of Victoria as author. The licence does not apply to any images, photographs or branding, including the Victorian Coat of Arms, the Victorian Government logo and the Department of Environment, Land, Water and Planning (DELWP) logo. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ Disclaimer This publication may be of assistance to you but the State of Victoria and its employees do not guarantee that the publication is without flaw of any kind or is wholly appropriate for your particular purposes and therefore disclaims all liability for any error, loss or other consequence which may arise from you relying on any information in this publication. -

Parliamentary Debates (Hansard)
EXTRACT FROM BOOK PARLIAMENT OF VICTORIA PARLIAMENTARY DEBATES (HANSARD) LEGISLATIVE COUNCIL FIFTY-EIGHTH PARLIAMENT FIRST SESSION Thursday, 21 June 2018 (Extract from book 9) Internet: www.parliament.vic.gov.au/downloadhansard By authority of the Victorian Government Printer The Governor The Honourable LINDA DESSAU, AC The Lieutenant-Governor The Honourable KEN LAY, AO, APM The ministry (from 16 October 2017) Premier ........................................................ The Hon. D. M. Andrews, MP Deputy Premier, Minister for Education and Minister for Emergency Services .................................................... The Hon. J. A. Merlino, MP Treasurer and Minister for Resources .............................. The Hon. T. H. Pallas, MP Minister for Public Transport and Minister for Major Projects .......... The Hon. J. Allan, MP Minister for Industry and Employment ............................. The Hon. B. A. Carroll, MP Minister for Trade and Investment, Minister for Innovation and the Digital Economy, and Minister for Small Business ................ The Hon. P. Dalidakis, MLC Minister for Energy, Environment and Climate Change, and Minister for Suburban Development ....................................... The Hon. L. D’Ambrosio, MP Minister for Roads and Road Safety, and Minister for Ports ............ The Hon. L. A. Donnellan, MP Minister for Tourism and Major Events, Minister for Sport and Minister for Veterans ................................................. The Hon. J. H. Eren, MP Minister for Housing, Disability and Ageing, Minister for Mental Health, Minister for Equality and Minister for Creative Industries .......... The Hon. M. P. Foley, MP Minister for Health and Minister for Ambulance Services ............. The Hon. J. Hennessy, MP Minister for Aboriginal Affairs, Minister for Industrial Relations, Minister for Women and Minister for the Prevention of Family Violence ............................................. The Hon. N. M. Hutchins, MP Special Minister of State ........................................ -

Aboriginal Affairs Victoria the Victorian Government Indigenous
Aboriginal Affairs Victoria The Victorian Government Indigenous Affairs Report July 2004 – June 2005 Figure 1: Front cover artwork Cover: “Walk With Me” Aunty Valda Cook, Wurundjeri/BoonurongReproduced courtesy of the artist. “The words on the painting says it all, however you will note that in the top left hand corner this area depicts an elders meeting council, you will also see the Sun rising from the east of Victoria as it goes over the bay and into the central Australia.” This publication is copyright. Apart from any fair dealing for the purposes of private study, research, criticism or review as permitted under the Copyright Act 1968, no part may be reproduced, copied, transmitted in any form or by any means (electronic, mechanical or graphic) without the prior written permission of the State of Victoria, Department for Victorian Communities. All requests and enquiries should be directed to the Copyright Officer, Department for Victorian Communities, 1 Spring Street, Melbourne, Victoria 3001. General Disclaimer: This publication may be of assistance to you but the State of Victoria and its employees do not guarantee that the publication is without flaw of any kind or is wholly appropriate for your particular purposes and therefore disclaims all liability for any error, loss or other consequence which may arise from you relying on any information in this publication. Foreword I am pleased to present the Victorian Government Indigenous Affairs Report: July 2004–June 2005. This report provides information on key initiatives in Indigenous affairs over the past year, a highlight of which was the amendment to Victoria’s Constitution recognising Aboriginal people’s unbroken connection to the land which became the colony of Victoria. -

Society Relies on Language to Communicate Ideas and Share Information, but As with Most Things, Language Can Be Used Positively Or Negatively
Society relies on language to communicate ideas and share information, but as with most things, language can be used positively or negatively. Unfortunately, language cannot be regarded as a neutral or unproblematic medium. Aboriginal and Torres Strait Islander people can experience language in negative ways, when it articulates the speaker’s unconscious bias, discrimination, prejudice, or racism. This document aims to clarify and inform the reader of appropriate uses of language and terms in relation to Indigenous Australian and Torres Strait Islander people/s. Appropriate and Inappropriate References and Terms Appropriate Terms Less Appropriate Terms ▪ Indigenous Australian people/s ▪ Aborigines or the Aborigines ▪ Aboriginal people/s ▪ Aboriginal, Aborigines ▪ Aboriginal person ▪ Blacks ▪ Torres Strait Islander people/s ▪ Coloured ▪ Torres Strait Islander person ▪ Native/s or the Native/s ▪ First Nations person ▪ Part-Aborigine ▪ First Nations people/s ▪ ‘full-blood’,’ half-caste’, ‘quarter-caste’ ▪ ‘octoroon’, ‘mulatto’, ‘hybrid’ There are also several slang terms that are still in use in modern vernacular, which are deemed to be racist and offensive. It is important to always keep in mind that different Aboriginal and Torres Strait Islander people have different ways of self-referral; for example, some people dislike the word Indigenous, as it can hark back to a time when Aboriginal people were included in the flora and fauna act. The best way to find out is to politely ask. Words that can be offensive to some Aboriginal and Torres Strait Islander people may be terms that others use for self-identification such as ‘Aborigine’. You may even see it in mainstream media, articles and papers, this does not, however this does not allow you to use that term(s). -

Cultural Water for Cultural Economies Report
CULTURAL WATER FOR CULTURAL ECONOMIES AUTHORS Dr Erin O’Donnell, Professor Lee Godden and Dr Katie O’Bryan. Final report of the The authors acknowledge the First Nations and Traditional Owners of Victoria Accessing water to meet Aboriginal economic and their elders past, present and emerging. First Nations and Traditional development needs Project. Published by Owners hold the knowledge, stories, custodial obligations and cultural University of Melbourne, 2021. knowledge that have always ensured the health of waterways and river Country. Each Nation and Traditional Owner group holds the cultural authority to speak for water, rivers and river Country within their traditional region. The Echuca Declaration states that ‘the Crown, Colonies, Commonwealth and States of Australia have been negligent in the management of the lands and waters of the Indigenous Nations causing ecosystem collapse, severe water quality degradation, extreme stress upon river ecologies and species extinction PROJECT PARTNERS at a scale and rate which is unprecedented.’ This negligence has brought ‘gross and widespread detriment to the cultural economy of the Indigenous Nations and degradation of significant landscapes and sites of spiritual and cultural importance’. We recognise that participation by First Nations and Traditional Owners in this project should not be taken as implying that any First Nation or Traditional Owner has approved of or authorised the settler-colonial water regime that has been imposed on their Country. This is the final report prepared for the Accessing Water to meet Aboriginal Economic Development Needs project (Program 1) and reflects the insights and key messages shared by Traditional Owners throughout Victoria during workshops and meetings throughout 2018-2020. -

A Guide to Traditional Owner Groups for Water Resource Plan Areas (Groundwater)
A Guide to Traditional Owner Groups for Water Resource Plan Areas (Groundwater) Groundwater Water Resource Plan Area Nations Groundwater Water Resource Plan Area Nations Australian Capital Territory Ngambri New South Wales Great Artesian Basin Shallow Barkindji GW1 Ngunnawal/Ngunawal GW13 Bigambul Ngarigu Budjiti Wulgalu Euahlayi Goulburn-Murray Bangerang Guwamu/Kooma GW2 Dhudhuroa Kambuwal Dja Dja Wurrung Gomeroi/Kamilaroi Taungurong Kunja Waywurru Kwiambul Yaithmathang Maljangapa Yorta Yorta Murrawarri Wimmera-Mallee Dja Dja Wurrung Ngarabal GW3 Latji Latji Ngemba Ngarket Wailwan Ngintait Wiradjuri Tati Tati Namoi Alluvium GW14 Gomeroi/Kamilaroi Wamba Wamba Gwydir Alluvium GW15 Gomeroi/Kamilaroi Watjobaluk Eastern Porous Rock Gomeroi/Kamilaroi Wergaia GW16 Ngarabal South Australian Murray Region Maraura Wiradjuri GW4 Ngarrindjeri New England Fractured Rock and Northern Basalts Bigambul Ngintait GW17 Githabul Eastern Mount Lofty Ranges GW5 Kaurna Kambuwal Western Porous Rock Barkindji Gomeroi/Kamilaroi GW6 Maraura Kwiambul Muthi Muthi Ngarabal Ngiyampaa New South Wales Border Rivers Alluvium Bigambul Nyeri Nyeri Githabul Tati Tati GW18 Kambuwal Wadi Wadi Gomeroi/Kamilaroi Wamba Wamba Kwiambul Weki Weki Queensland Border Rivers Bigambul Darling Alluvium Budjiti GW19 Githabul GW7 Euahlayi Kambuwal Murrawarri Gomeroi/Kamilaroi Ngemba Moonie Bigambul Wailwan Gomeroi/Kamilaroi Murray Alluvium Bangerang Mandandanji GW8 Barapa Barapa Condamine Balonne Barunggam Nyeri Nyeri GW21 Bidjara Tati Tati Bigambul Wadi Wadi Euahlayi Wamba Wamba Gomeroi/Kamilaroi