P53, Cancer and the Immune Response Julianna Blagih, Michael D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Female Fellows of the Royal Society
Female Fellows of the Royal Society Professor Jan Anderson FRS [1996] Professor Ruth Lynden-Bell FRS [2006] Professor Judith Armitage FRS [2013] Dr Mary Lyon FRS [1973] Professor Frances Ashcroft FMedSci FRS [1999] Professor Georgina Mace CBE FRS [2002] Professor Gillian Bates FMedSci FRS [2007] Professor Trudy Mackay FRS [2006] Professor Jean Beggs CBE FRS [1998] Professor Enid MacRobbie FRS [1991] Dame Jocelyn Bell Burnell DBE FRS [2003] Dr Philippa Marrack FMedSci FRS [1997] Dame Valerie Beral DBE FMedSci FRS [2006] Professor Dusa McDuff FRS [1994] Dr Mariann Bienz FMedSci FRS [2003] Professor Angela McLean FRS [2009] Professor Elizabeth Blackburn AC FRS [1992] Professor Anne Mills FMedSci FRS [2013] Professor Andrea Brand FMedSci FRS [2010] Professor Brenda Milner CC FRS [1979] Professor Eleanor Burbidge FRS [1964] Dr Anne O'Garra FMedSci FRS [2008] Professor Eleanor Campbell FRS [2010] Dame Bridget Ogilvie AC DBE FMedSci FRS [2003] Professor Doreen Cantrell FMedSci FRS [2011] Baroness Onora O'Neill * CBE FBA FMedSci FRS [2007] Professor Lorna Casselton CBE FRS [1999] Dame Linda Partridge DBE FMedSci FRS [1996] Professor Deborah Charlesworth FRS [2005] Dr Barbara Pearse FRS [1988] Professor Jennifer Clack FRS [2009] Professor Fiona Powrie FRS [2011] Professor Nicola Clayton FRS [2010] Professor Susan Rees FRS [2002] Professor Suzanne Cory AC FRS [1992] Professor Daniela Rhodes FRS [2007] Dame Kay Davies DBE FMedSci FRS [2003] Professor Elizabeth Robertson FRS [2003] Professor Caroline Dean OBE FRS [2004] Dame Carol Robinson DBE FMedSci -

The Ubiquitin Proteasome System and Its Involvement in Cell Death Pathways
Cell Death and Differentiation (2010) 17, 1–3 & 2010 Macmillan Publishers Limited All rights reserved 1350-9047/10 $32.00 www.nature.com/cdd Editorial The ubiquitin proteasome system and its involvement in cell death pathways F Bernassola1, A Ciechanover2 and G Melino1,3 Cell Death and Differentiation (2010) 17, 1–3; doi:10.1038/cdd.2009.189 Following the awarding of the 2004 Nobel Prize in Chemistry Inactivation of the proteasome following caspase-mediated to Aaron Ciechanover, Avram Hershko, and Irwin A Rose cleavage may disable the proteasome, interfering with its for the discovery of ubiquitin (Ub)-mediated degradation, role in the regulation of key cellular processes and thereby Cell Death and Differentiation has drawn the attention of facilitating induction of apoptosis. The noted recent develop- its readers to the Ub Proteasome System (UPS) and its ments show how understanding of these functions is just involvement in regulating cell death pathways.1–4 The current starting to emerge. For example, why does dIAP1 associate set of reviews is an update on this theme.5–16 with multiple E2s via its RING finger? Does dIAP1 also interact From previous review articles published in Cell Death and with the E3 – the F-box protein Morgue, which is a part of an Differentiation, it was apparent that the UPS has a major SCF E3 complex? Why does dIAP1, which is an E3, have to mechanistic role in regulating cell death via modification and interact with other ligases such as the N-end rule UBR1 and degradation of key regulatory proteins involved in -

A Conversation with Karen Vousden
A Conversation with Karen Vousden INTERVIEWER:JAN WITKOWSKI Executive Director, Banbury Center at Cold Spring Harbor Laboratory Karen Vousden is Director of the Cancer Research UK Beatson Institute. Jan Witkowski: Over the past few years, there’s been a tomography) imaging. It certainly is the case that many markedly increasing emphasis and interest in the metab- cancers have a high rate of glucose uptake, which is olism and biochemistry of cancers. It’s moving away what we measure when we do functional imaging, or a from just the genes and proteins. Am I right in thinking PET scan. that? However, over recent years our understanding of the Warburg effect has become more sophisticated, although Dr. Vousden: Yes, I think you’re absolutely right. we still don’t quite understand it. We know now that there There’s been a resurgence of interest in metabolism. In probably are changes in the metabolism of almost all the middle of the last century a lot of energy was spent on cancers. We’re interested in understanding that and then understanding metabolism and biochemists at this time asking, “Can we harness any of this information to were making huge progress. Many metabolic pathways develop new therapies?” were worked out in exquisite detail in the ’50s and the ’60s. Then came the oncogene revolution, and much of Jan Witkowski: Can you tell me a little about your the emphasis switched to understanding the regulation current work? of the cell cycle and signal transduction. At this point, metabolism was almost forgotten in cancer biology until Dr. -

3718 Issue63july2010 1.Pdf
Issue 63.qxd:Genetic Society News 1/10/10 14:41 Page 1 JULYJULLYY 2010 | ISSUEISSUE 63 GENETICSGENNETICSS SOCIETYSOCIEETY NENEWSEWS In this issue The Genetics Society NewsNewws is edited by U Genetics Society PresidentPresident Honoured Honoured ProfProf David Hosken and items ittems for future future issues can be sent to thee editor,editor, preferably preferably U Mouse Genetics Meeting by email to [email protected],D.J.Hosken@@exeter.ac.uk, or U SponsoredSponsored Meetings Meetings hardhard copy to Chair in Evolutionary Evoolutionary Biology, Biology, UniversityUniversity of Exeter,Exeter, Cornwall Cornnwall Campus, U The JBS Haldane LectureLecture Tremough,Tremough, Penryn, TR10 0 9EZ UK.UK. The U Schools Evolutionn ConferenceConference Newsletter is published twicet a year,year, with copy dates of 1st June andand 26th November.November. U TaxiTaxi Drivers The British YeastYeaste Group Group descend on Oxford Oxford for their 2010 meeting: m see the reportreport on page 35. 3 Image © Georgina McLoughlin Issue 63.qxd:Genetic Society News 1/10/10 14:41 Page 2 A WORD FROM THE EDITOR A word from the editor Welcome to issue 63. In this issue we announce a UK is recognised with the award of a CBE in the new Genetics Society Prize to Queen’s Birthday Honours, tells us about one of Welcome to my last issue as join the medals and lectures we her favourite papers by Susan Lindquist, the 2010 editor of the Genetics Society award. The JBS Haldane Mendel Lecturer. Somewhat unusually we have a News, after 3 years in the hot Lecture will be awarded couple of Taxi Drivers in this issue – Brian and seat and a total of 8 years on annually to recognise Deborah Charlesworth are not so happy about the committee it is time to excellence in communicating the way that the print media deals with some move on before I really outstay aspects of genetics research to scientific issues and Chris Ponting bemoans the my welcome! It has been a the public. -

SCIENTIFIC REPORT 2013 Cruk.Org SCIENTIFIC Cover Image Graduate Student Loic Fort from Laura Machesky’S Group
SCIENTIFIC REPORT 2013 cruk.org SCIENTIFIC Cover image Graduate student Loic Fort from Laura Machesky’s group. REPORT 2013 BEATSON INSTITUTE CONTENTS SECTION 1 ADVANCED TECHNOLOGIES INTRODUCTION 04 Kurt Anderson 48 RESEARCH HIGHLIGHTS 06 Beatson Advanced Imaging Resource (BAIR) BACKGROUND 10 Gabriela Kalna 49 Bioinformatics and Computational Biology CANCER RESEARCH UK BEATSON INSTITUTE Gillian Mackay 50 Metabolomics REGULATION OF CANCER CELL GROWTH METABOLISM AND SURVIVAL Nick Morrice 51 Eyal Gottlieb 12 Proteomics and Mass Spectrometry Apoptosis and Tumour Metabolism Emma Shanks 52 Danny Huang 14 RNAi Screening Ubiquitin Signalling Karen Blyth 53 Hing Leung 16 Transgenic Models of Cancer Prostate Cancer Biology Douglas Strathdee 54 Kevin Ryan 18 Transgenic Technology Tumour Cell Death Karen Vousden 20 SECTION 2 Tumour Suppression BEATSON ASSOCIATES Peter D. Adams 56 REGULATION OF CANCER CELL INVASION Epigenetics of Cancer and Ageing AND METASTASIS Daniel J. Murphy 58 Kurt Anderson 24 Oncogene-Induced Vulnerabilities Tumour Cell Migration Stephen Tait 60 Jeff Evans 26 Mitochondria and Cell Death Translational Cancer Therapeutics Robert Insall 28 UNIVERSITY OF GLASGOW Cell Migration and Chemotaxis Jeff Evans 64 Laura Machesky 30 Institute of Cancer Sciences Migration, Invasion and Metastasis Jim Norman 32 SECTION 3 Integrin Cell Biology RESEARCH FACILITIES 72 The Beatson Institute for Cancer Michael Olson 34 PUBLICATIONS 76 Research building Molecular Cell Biology CONFERENCES AND WORKSHOPS 90 Owen Sansom 36 SEMINARS 92 Colorectal Cancer -

Smutty Alchemy
University of Calgary PRISM: University of Calgary's Digital Repository Graduate Studies The Vault: Electronic Theses and Dissertations 2021-01-18 Smutty Alchemy Smith, Mallory E. Land Smith, M. E. L. (2021). Smutty Alchemy (Unpublished doctoral thesis). University of Calgary, Calgary, AB. http://hdl.handle.net/1880/113019 doctoral thesis University of Calgary graduate students retain copyright ownership and moral rights for their thesis. You may use this material in any way that is permitted by the Copyright Act or through licensing that has been assigned to the document. For uses that are not allowable under copyright legislation or licensing, you are required to seek permission. Downloaded from PRISM: https://prism.ucalgary.ca UNIVERSITY OF CALGARY Smutty Alchemy by Mallory E. Land Smith A THESIS SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY GRADUATE PROGRAM IN ENGLISH CALGARY, ALBERTA JANUARY, 2021 © Mallory E. Land Smith 2021 MELS ii Abstract Sina Queyras, in the essay “Lyric Conceptualism: A Manifesto in Progress,” describes the Lyric Conceptualist as a poet capable of recognizing the effects of disparate movements and employing a variety of lyric, conceptual, and language poetry techniques to continue to innovate in poetry without dismissing the work of other schools of poetic thought. Queyras sees the lyric conceptualist as an artistic curator who collects, modifies, selects, synthesizes, and adapts, to create verse that is both conceptual and accessible, using relevant materials and techniques from the past and present. This dissertation responds to Queyras’s idea with a collection of original poems in the lyric conceptualist mode, supported by a critical exegesis of that work. -

The ST Cross College Magazine 2015 Ad Quattuor Cardines Mundi
CROSSWORD THE ST CROSS COLLEGE MAGAZINE 2015 AD QUAttUOR CARDINES MUNDI Contents ST Cross COLLEGE West Quad Campaign UNIVERSITY OF OXFORD 04 An update on the progress towards achieving this landmark project COVER STORY – The 161st Boat Race 05 St Cross students making history on the Tideway The Body in the Garden 06 Recent investigations undertaken by Oxford Archaeology ahead of the construction of the West Quad revealed a body in the garden The St Cross 50th Anniversary Lecture Series 08 This series of termly lectures brought three eminent speakers to Oxford to celebrate the th Crossword – Issue 23 College’s 50 Anniversary Editor: Susan Berrington St Cross Merchandise 09 A selection of gifts, books and momentos Managing Editor: Ella Bedrock Design: Broccoli Creative Design AI Risk 10 Stuart Armstrong looks at the risks associated with Contact details: Artificial Intelligence The Development & Alumni Relations Office St Cross College Students’ News 61 St Giles 12 Oxford ‘Four Corners’ - The St Cross International Poetry OX1 3LZ 13 Competition 2015 Tel: +44 (0)1865 278480 Kate Venables talks of the success of the ‘Four Corners’ Email: [email protected] International Poetry Competition www.stx.ox.ac.uk St Cross College Photography Competition 2015 Cover Image: 14 Students Jamie Cook (MSc Engineering Science) and Shelley Pearson (MSc Child Development Sports News and Education), who were in the winning Dark 16 Blue boats in this year’s Oxford and Cambridge Members’ News Boat Race, with Olympic gold medallist rower 18 Tim Foster (Dip Social Studies, 1996). Matriculation and College Photographs Photo credit: Phil Sills 20 The 2015 Telethon This edition of Crossword is printed using an 22 A conversation from the call room environmentally friendly, waterless printing process, on Forest Stewardship Council (FSC) certified paper and to Eco Management Audit The Four Corners of the World Scheme (EMAS) standards. -

Mapping Oesophageal Cancer Genes Leads to New Drug Targets 4 February 2019
Mapping oesophageal cancer genes leads to new drug targets 4 February 2019 sensitive to drugs (CDK4/6 inhibitors) already in clinical trials for breast cancer. This means phase II/III clinical trials to treat oesophageal cancer could be feasible in one to two years. Interestingly, women were found to have more KRAS mutations than men. These mutations are often seen in other cancer types, but are rarely found in oesophageal cancer. This could indicate a different sub-type of the disease in women and suggest they may have a different prognosis or be eligible for other treatments. Professor Rebecca Fitzgerald, Cancer Research UK funded scientist and lead researcher at the MRC Cancer Unit, said: "This research could completely shift the paradigm from giving A depiction of the double helical structure of DNA. Its oesophageal cancer patients the same four coding units (A, T, C, G) are color-coded in pink, chemotherapy that we know doesn't always work, orange, purple and yellow. Credit: NHGRI to more targeted treatments based on individual characteristics of a patient's cancer. "We are now designing clinical trials that provide Mutations that cause oesophageal real-time analysis of patients' genes to offer adenocarcinoma (OAC) have been mapped in patients the best treatment based on their own unprecedented detail—unveiling that more than half genome. could be targeted by drugs currently in trials for other cancer types. "This research could also provide better options for older patients, who are more likely to develop This research, published today in Nature Genetics, oesophageal cancer, and who are often not fit could help stratify oesophageal cancer patients to enough for current treatment options." give them more personalised therapies. -
Detailed Program
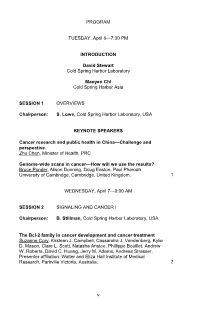
PROGRAM TUESDAY, April 6—7:30 PM INTRODUCTION David Stewart Cold Spring Harbor Laboratory Maoyen Chi Cold Spring Harbor Asia SESSION 1 OVERVIEWS Chairperson: S. Lowe, Cold Spring Harbor Laboratory, USA KEYNOTE SPEAKERS Cancer research and public health in China—Challenge and perspective. Zhu Chen, Minister of Health, PRC Genome-wide scans in cancer—How will we use the results? Bruce Ponder, Alison Dunning, Doug Easton, Paul Pharoah. University of Cambridge, Cambridge, United Kingdom. 1 WEDNESDAY, April 7—9:00 AM SESSION 2 SIGNALING AND CANCER I Chairperson: B. Stillman, Cold Spring Harbor Laboratory, USA The Bcl-2 family in cancer development and cancer treatment Suzanne Cory, Kirsteen J. Campbell, Cassandra J. Vandenberg, Kylie D. Mason, Clare L. Scott, Natasha Anstee, Phillippe Bouillet, Andrew W. Roberts, David C. Huang, Jerry M. Adams, Andreas Strasser. Presenter affiliation: Walter and Eliza Hall Institute of Medical Research, Parkville Victoria, Australia. 2 v Regulators of Invadopodia formation and cancer cell invasion Barbara Blouw, Matt Buschman, Pilar Cejudo-Martin, Begoña Diaz, Christine Gould, Danielle Murphy, Manuela Quintavalle, Susanne Heynen, Behrad Azimi, Jeff Price, Sara A. Courtneidge. Presenter affiliation: The Burnham Institute for Medical Research, La Jolla, California. 3 Axes of aging—Telomeres, checkpoints and mitochondria Ergun Sahin, Ronald A. DePinho. Presenter affiliation: Belfer Institute for Applied Cancer Science, Boston, Massachusetts; Dana-Farber Cancer Institute and Harvard Medical School, Boston, Massachusetts. 4 TGF-β signaling for regulation of cancer Kohei Miyazono, Hiroaki Ikushima, Yoko Katsuno, Shogo Ehata. Presenter affiliation: University of Tokyo, Tokyo, Japan. 5 ALK fusion genes, a new target in lung cancer Hiroyuki Mano. -

Genes and Cancer Meeting
Monday 8th April 10.00 - 12.00 Early Career Workshop Chair: Kevin Ryan, Beatson Institute for Cancer Research 10.05 - 10.25 Demystifying career pathways in large pharma Susan Critchlow, AstraZeneca, United Kingdom 10.25 - 10.45 Title TBC Tracy Weightman, Translation Executive, Cancer Research UK Commercial Partnership, United Kingdom 10.45 - 11.05 Inside the black box of Nature; Who Nature editors are and how we make decisions Barbara Marte, Senior Editor, Nature, United Kingdom 11.05 - 11.25 From bench to desk: working in science outside the lab Áine McCarthy, Senior Communications and Marketing Manager, Children’s Cancers, Cancer Research UK, United Kingdom 11.25 - 12.00 Discussion The early career workshop is sponsored by: 12.00 - 13.30 Lunch (Early Career Workshop attendees only) 13.50 - 14.00 Opening remarks & welcome Kevin Ryan, Cancer Research UK Beatson Institute, United Kingdom and Chair, Organising Committee 14.00 - 15.30 Session 1: Gene expression in cancer Chair: Jason Carroll, Cancer Research UK Cambridge Institute 14.00 - 14.30 O1.1 Modifications of RNA: their function and role in cancer Tony Kouzarides, University of Cambridge, United Kingdom 14.30 - 15.00 O1.2 The role of post-transcriptional control in cancer development Anne Willis, University of Cambridge, United Kingdom Short talks selected from abstracts: 15.00 - 15.20 SO1.3 The Myb-MuvB complex is required for YAP-dependent transcription of mitotic genes Stefan Gaubatz, University of Wuerzburg, Germany 15.20 - 15.35 SO1.4 NF-κB regulation of the CHK1 adaptor protein -

Communicating Biochemistry: Meetings and Events
© The Authors. Volume compilation © 2011 Portland Press Limited Chapter 3 Communicating Biochemistry: Meetings and Events Ian Dransfield and Brian Beechey Scientific conferences organized by the Biochemical Society represent a key facet of activity throughout the Society’s history and remain central to the present mission of promoting the advancement of molecular biosciences. Importantly, scientific conferences are an important means of communicating research findings, establishing collaborations and, critically, a means of cementing the community of biochemical scientists together. However, in the past 25 years, we have seen major changes to the way in which science is communicated and also in the way that scientists interact and establish collabo- rations. For example, the ability to show videos, “fly through” molecular structures or show time-lapse or real-time movies of molecular events within cells has had a very positive impact on conveying difficult concepts in presentations. However, increased pressures on researchers to obtain/maintain funding can mean that there is a general reluctance to present novel, unpublished data. In addition, the development of email and electronic access to scientific journals has dramatically altered the potential for communi- cation and accessibility of information, perhaps reducing the necessity of attending meetings to make new contacts and to hear exciting new science. The Biochemical Society has responded to these challenges by progressive development of the meetings format to better match the -

REPORTER S P E C I a L No 6 T U E S D Ay 24 a P R I L 2018 Vol Cxlviii
CAMBRIDGE UNIVERSITY REPORTER S PECIAL NO 6 T UE S D AY 24 A PRIL 2018 VOL CXLVIII MEMBERS OF UNIVERSITY BODIES REPRESENTATIVES OF THE UNIVERSITY (‘OFFICERS NUMBER’, PARTS II AND III) PUBLISHED BY AUTHORITY [SPECIAL NO. 6 MEMBERS OF UNIVERSITY BODIES REPRESENTATIVES OF THE UNIVERSITY P ART II: M E mb ER S OF U N I V ER S I T Y B ODIE S Nominating and appointing bodies: abbreviations 1 Faculty Boards and Degree Committees 18 Septemviri, Discipline Committee, University Tribunal 1 Committees 26 Discipline Board 2 Trustees, Managers, Awarders, of Funds, Council, Audit Committee, Finance Committee 2 Scholarships, Studentships, Prizes, etc. 32 General Board of the Faculties 2 Representatives of the Colleges for Election of Other Committees of the Central Bodies 2 Members of the Finance Committee 51 Boards of Electors to Professorships 6 P ART III: R EPRE S E ntAT I V E S OF th E U N I V ER S I T Y Advisory Committees for Elections to Professorships 7 Boards of Electors to offices other than Professorships 7 1. Representative Governors, etc. 52 Syndicates 8 2. Representative Trustees Associated with the Boards 9 University 53 Councils of the Schools 11 3. Cambridge Enterprise Ltd: Board of Directors 53 Appointments Committees 12 NOTICE BY thE EDITOR Following the publication of Part I of the Officers Number in February 2018, this issue of Part II (Members of University Bodies) and Part III (Representatives of the University) includes data received up to 13 April 2018. The next update of Part I (University Officers) will be published in Lent Term 2019 and an update to Parts II and III will follow shortly thereafter.