2 March 2009
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Notification
Government of Jammu and Kashmir (UT) OFFICE OF THE CHIEF EDUCATION OFFICER KISHTWAR Ground Floor Mini Secretariat New DC Complex Kishtwar (E-mail: [email protected]/ Fax: 01995-261000) Sub:-Tentative Seniority list of Jr.Librarian / Junior Assistants/ In-Charge Junior Assistants / Laboratory Assistants/ In-Charge Laboratory Assistants / Library Assistants /In-Charge Library Assistants of District Kishtwar. NOTIFICATION The tentative seniority list of Jr. Librarian / Junior Assistants/ In-Charge Junior Assistants / Laboratory Assistants/ In-Charge Laboratory Assistant / Library Assistant /In- Charge Library Assistants has been framed on the basis of feedback received from the all the Drawing Disbursing Officer of Kishtwar District and is uploaded in the website (www.schedujammu.nic.in) for information of the concerned officials for verifying their particulars with reference to their original service records. Any variation in the particulars / dropout in the list shall be reported to this office, with documentary evidence duly recommended by the respective Drawing Disbursing Officers and such claim should reach this office within 05 days from the date of publication of this notification in the newspapers. After expiry of stipulated period of 05 days, the Drawing & Disbursing Officer (DDOs ) concerned will furnish the service particulars of the officials with the following certificate conspicuously recorded at the bottom of service particulars, so that final updated seniority list will be prepared by this office accordingly. 1. That the official listed in the tentative seniority list has genuine appointment on substantive basis. Any official having any criminal cases in VOJ/Crime, FIR, Court or departmental enquiry be conspicuously noted in the remarks Colum mention the FIR No. -

OFFICE of the CHIEF EDUCATION OFFICER DODA Tentative Seniority List of Junior Assistants in Respect of District Doda…
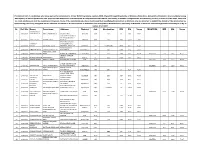
OFFICE OF THE CHIEF EDUCATION OFFICER DODA Tentative Seniority list of Junior Assistants in respect of District Doda… Date of First DATE FROM QUALI- WHICH WORKING S-NO Zone NAME OF OFFICIALS SEX PLACE OF POSTING D-O-B appointment RESEIDENCE CATEGORY REMAKRS FICATION IN THE as Jr- Asstt INSTITUTION 1 Thathri Nisar Ahmed Male HSS Jangalwar 12th 13-02-1974 23-05-2009 19-05-2016 Phagsoo RBA 2 Doda Shaishta Kouser Female DIET Doda BSc, DCA 26-05-1974 01-04-2010 24-04-2010 Doda Gen 3 Bhaderwah Abida Begum Female HSS Boys Bhaderwah 10+2 02-10-1966 20-03-2014 28-05-2018 Bhaderwah Gen 4 Doda Imtiaz Hussain Male ZEO Office Doda BA 24-10-1974 30-05-2014 30-05-2014 Shinal Doda Gen 5 Bhaderwah Archana Kotwal Female HSS Boys Bhaderwah MSc IT 20-04-1984 30-05-2014 30-05-2014 Udrana Gen 6 Doda Sajad Hussain Male DIET Doda B-A- 06-07-1985 30-05-2014 30-05-2014 Doda Gen 7 Bhagwah Vikram singh Male ZEO Office Bhagwah Matric 18-09-1971 20-06-2014 20-06-2014 Gadi RBA Promoted through 8 Doda Taib Hussain Male HSS Sazan 12th 11-10-1991 16-08-2014 16-08-2014 Sazan RBA Hon'ble Court 9 Gundna Ved Perkash Male HS Barshalla 10th 01-07-1965 21-08-2014 10-08-2016 Thathri SC 10 Doda Farooq Ahmed Male HSS Boys Doda 12TH 07-02-1968 21-08-2014 04-06-2018 Doudhte Gen 11 Bhaderwah Zakir Hussain Male HS Manthala 12th 06-08-1971 22-08-2014 05-06-2017 Banoon Bonjwah Gen 12 Thathri Daya Krishan Male HSS Bhella B-A- 25-03-1972 21-08-2014 29-05-2018 Shaja RBA 13 Thathri Javeed Ahmed Male ZEO Office Thathri 10th 15-08-1972 22-08-2014 Aug-16 Thathri Gen 14 Assar Imtyaz Ahmed Male -

An Ethnobotanical Study of Medicinal Plants Used by the Locals in Kishtwar, Jammu and Kashmir, India
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by OpenSIUC Ethnobotanical Leaflets 13: 1240-56 , 2009. An Ethnobotanical Study of Medicinal Plants used by the Locals in Kishtwar, Jammu and Kashmir, India Mahesh Kumar, Yash Paul and V. K. Anand Department of Botany, University of Jammu, Jammu.-180006 e-mail. [email protected] Issued October 01, 2009 Abstract This study represents a systematic attempt to explore the knowledge of the native people about plants, which they use to cure diseases. And it is an attempt towards conserving the local knowledge of people to plants. This paper presents a list and uses of some medicinal plants distributed in the high altitude district Kishtwar in Jammu and Kashmir. The list was prepared during an ethno-botanical survey of the region from December 2007 to January, 2009. This paper provides information about 71 ethno-medicinally useful plants grown in this region. In this paper, family, botanical name, local name, ethnomedicinal uses are given for each plant. Introduction It is documented that 80% of the world population has faith in traditional medicines, particularly plant drugs for their primary healthcare (Kala et al., 2006). The use of plants for medicinal purposes and human sustenance has been in practice in India since the Vedic age. The earliest mention of the medicinal use of the plants is found in the Rigveda, 1500-400 BC, Athurveda 1500 BC, Upnishada 1000-600 BC (Chauhan, 1999). In India about 17000 species of higher plants out of which 7500 are known for medicinal uses (Shiva, 1996). -

Sr. Form No. Name Parentage Address District Cat. MM MO Acad.%Age 1 20600614 YASMEENA AHAD KH
General Merit list of candidates who have applied for admission to MA Education Progamme (Distance Mode) session-2020 Sr. Form No. Name Parentage Address District Cat. MM MO Acad.%age 1 20600614 YASMEENA AHAD KH. ABDUL AHAD WANI NAMBLABAL PAMPORE PULWAMA OM 10 8.4 84.00 2 20601519 MEHFOOZA ASHIQ ASHIQ HUSSAIN MIR CHADOORA BUDGAM OM 1000 835 83.50 3 20600464 IQRA GULAM MOHD QASBA NUND RESHI COLONY A BEMINA SRINAGAR OM 100 82 82.00 4 20600013 RASIK AHMAD RESHI GUL MOHD RESHI GUNDINOWROZE ANANTNAG OM 945 770 81.48 5 20601399 MUDASIR AHMAD HAJAM BASHIR AHMAD HAJAM BAKUR ALASTENG GANDERBAL GANDERBAL WUP 1000 811 81.10 BABAPORA, BABADEMB ROAD, 6 20602361 SOHAN CHOUDHARY BHOLA RAM CHOUDHARY SRINAGAR SRINAGAR OM 1000 809 80.90 7 20602039 MUSTAFA MAJEED AB MAJEED SHAH HAJI BAGH HMT BUDGAM BUDGAM OM 1000 808 80.80 8 20600861 ABID HUSSAIN HAJI MOHD AMIN HAJI SEDOW SHOPIAN SHOPIAN RBA 1000 806 80.60 9 20600983 ASIMA MANZOOR GANIE MANZOOR AHMAD GANIE CHANDHARA PAMPORE PULWAMA PULWAMA OM 100 80.4 80.40 PHASE-II, ALAMDAR BASTI, CHARAR-- 10 20601853 UMAR YOUSEF MOHD YOUSEF KHIRKA SHARIEF BUDGAM OM 10 8 80.00 11 20600127 ARSHID AHMAD MIR GHULAM MOHAMMAD MIR KANITAR SEDRABAL SRINAGAR SRINAGAR OM 10 7.98 79.80 12 20601369 INSHA GUL GULAM MOHAMMAD BHAT SHAH HAMDAN COLONY NAIK BAGH SRINAGAR OM 10 7.93 79.30 13 20600164 RUKHSANA MOHAMMAD HAFIZ DAR ZADIBAL HAWAL SRINAGAR OM 10 7.91 79.10 14 20601935 AASHAQ HUSSAIN WANI MOHD ABDULLAH WANI GUNDI SHAMASH BUDGAM RBA 1000 789 78.90 15 20600062 MASARAT NABI BADANA GH NABI BADANA ZAKURA HAZRATBAL SRINAGAR CGB 1000 782 78.20 NUNDRESHI COLONY BEMINA 16 20601409 SADAF ZAHOOR ZAHOOR AHMAD KHAN SRINAGAR SRINAGAR OM 330 258 78.18 17 20601556 NIDA BASHIR BASHIR AHMAD ZADOO HOUSE NO 141 BEMINA BYPASS SRINAGAR OM 10 7.79 77.90 H.NO. -

Directory Establishment
DIRECTORY ESTABLISHMENT SECTOR :URBAN STATE : JAMMU & KASHMIR DISTRICT : Anantnag Year of start of Employment Sl No Name of Establishment Address / Telephone / Fax / E-mail Operation Class (1) (2) (3) (4) (5) NIC 2004 : 0121-Farming of cattle, sheep, goats, horses, asses, mules and hinnies; dairy farming [includes stud farming and the provision of feed lot services for such animals] 1 DEPARTMENT OF ANIMAL HUSBANDRY NAZ BASTI ANTNTNAG OPPOSITE TO SADDAR POLICE STATION ANANTNAG PIN CODE: 2000 10 - 50 192102, STD CODE: NA , TEL NO: NA , FAX NO: NA, E-MAIL : N.A. NIC 2004 : 0122-Other animal farming; production of animal products n.e.c. 2 ASSTSTANT SERICULTURE OFFICER NAGDANDY , PIN CODE: 192201, STD CODE: NA , TEL NO: NA , FAX NO: NA, E-MAIL : N.A. 1985 10 - 50 3 INTENSIVE POULTRY PROJECT MATTAN DTSTT. ANANTNAG , PIN CODE: 192125, STD CODE: NA , TEL NO: NA , FAX NO: 1988 10 - 50 NA, E-MAIL : N.A. NIC 2004 : 0140-Agricultural and animal husbandry service activities, except veterinary activities. 4 DEPTT, OF HORTICULTURE KULGAM TEH KULGAM DISTT. ANANTNAG KASHMIR , PIN CODE: 192231, STD CODE: NA , 1969 10 - 50 TEL NO: NA , FAX NO: NA, E-MAIL : N.A. 5 DEPTT, OF AGRICULTURE KULGAM ANANTNAG NEAR AND BUS STAND KULGAM , PIN CODE: 192231, STD CODE: NA , 1970 10 - 50 TEL NO: NA , FAX NO: NA, E-MAIL : N.A. NIC 2004 : 0200-Forestry, logging and related service activities 6 SADU NAGDANDI PIJNAN , PIN CODE: 192201, STD CODE: NA , TEL NO: NA , FAX NO: NA, E-MAIL : 1960 10 - 50 N.A. 7 CONSERVATOR LIDDER FOREST CONSERVATOR LIDDER FOREST DIVISION GORIWAN BIJEHARA PIN CODE: 192124, STD CODE: 1970 10 - 50 DIVISION NA , TEL NO: NA , FAX NO: NA, E-MAIL : N.A. -
Provisional List of Candidates Who Have Applied for Admission to 2
Provisional List of candidates who have applied for admission to 2-Year B.Ed.Programme session-2020 offered through Directorate of Distance Education, University of Kashmir. Any candidate having discrepancy in his/her particulars can approach the Directorate of Admissions & Competitive Examinations, University of Kashmir alongwith the documentary proof by or before 31-07-2021, after that no claim whatsoever shall be considered. However, those of the candidates who have mentioned their Qualifying Examination as Masters only are directed to submit the details of the Graduation by approaching personally alongwith all the relevant documnts to the Directorate of Admission and Competitive Examinaitons, University of Kashmir or email to [email protected] by or before 31-07-2021 Sr. Roll No. Name Parentage Address District Cat. Graduation MM MO %age MASTERS MM MO %age SHARIQ RAUOF 1 20610004 AHMAD MALIK ABDUL AHAD MALIK QASBA KHULL KULGAM RBA BSC 10 6.08 60.80 VPO HOTTAR TEHSILE BILLAWAR DISTRICT 2 20610005 SAHIL SINGH BISHAN SINGH KATHUA KATHUA RBA BSC 3600 2119 58.86 BAGHDAD COLONY, TANZEELA DAWOOD BRIDGE, 3 20610006 RASSOL GH RASSOL LONE KHANYAR, SRINAGAR SRINAGAR OM BCOMHONS 2400 1567 65.29 KHAWAJA BAGH 4 20610008 ISHRAT FAROOQ FAROOQ AHMAD DAR BARAMULLA BARAMULLA OM BSC 1800 912 50.67 MOHAMMAD SHAFI 5 20610009 ARJUMAND JOHN WANI PANDACH GANDERBAL GANDERBAL OM BSC 1800 899 49.94 MASTERS 700 581 83.00 SHAKAR CHINTAN 6 20610010 KHADIM HUSSAIN MOHD MUSSA KARGIL KARGIL ST BSC 1650 939 56.91 7 20610011 TSERING DISKIT TSERING MORUP -
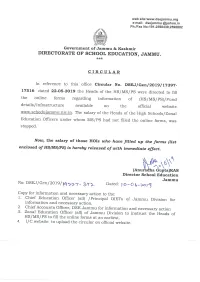
Circular on Drawal of Salary
LIST OF SCHOOLS WHO HAVE FILLED THE FORM TILL 10-6-19 S.NO DISTRICT NAME OF SCHOOL TYPE NAME OF INCHARGE 1 DODA BHALESSA HS THALORAN HS DEYAL SINGH PARIHAR 2 DODA ASSAR HS KALHOTA HS MOHD IQBAL 3 DODA ASSAR HS BAGAR HS RUKHSANA KOUSAR 4 DODA ASSAR HS BULANDPUR HS SURESH KUMAR 5 DODA ASSAR HS HAMBAL HS ROMESH CHANDER 6 DODA ASSAR LOWERHS JATHI HS NAZIR HUSSAIN 7 DODA ASSAR HS BARRI HS MOHD SAFDER 8 DODA ASSAR HS MANGOTA HS MOHD SAFDER 9 DODA ASSAR HS MALHORI HS YOG RAJ 10 DODA ASSAR HS THANDA PANI HS KULDEEP RAJ 11 DODA ASSAR HS ROAT HS MOHD ASSDULLAH 12 DODA ASSAR HS MOOTHI HS JAVED HUSSAIN 13 DODA BHADARWAH LHS NAGAR HS NUSRAT JAHAN 14 DODA BHADARWAH HS MATHOLA HS SHAHEEN BEGUM 15 DODA BHADARWAH GHS MANTHLA HS SAYEDA BEGUM 16 DODA BHADARWAH HS THANALLA HS AJIT SINGH MANHAS 17 DODA BHADARWAH HS BHEJA BHADERWAH HS MUMTAZ BEGUM 18 DODA BHAGWAH HS SOOLI HS GHULAM MOHD 19 DODA BHALESSA GHS KILHOTRAN HS(G) MOHD ABASS 20 DODA BHALESSA HS BATARA HS ABDUL RASHID 21 DODA BHALESSA HS DHAREWRI HS MOHD SHAFI KHAN 22 DODA BHALESSA HS BHARGI HS KHATAM HUSSAIN 23 DODA BHALESSA HS BHARTHI HS TALKING HUSSAIN 24 DODA BHALESSA HS ALNI HS TALIB HUSSAIN 25 DODA BHALESSA HS GANGOTA HS JAVID IQBALL MASTER 26 DODA BHALLA HS SERI HS SHAHEENA AKHTER 27 DODA BHALLA GHS CHATTRA HS HEADMASTER 28 DODA BHALLA HS BHAGRATHA HS KULBIR SINGH 29 DODA BHATYAD HS HADDAL HS MOHD ASLAM INCHARGE 30 DODA BHATYAS GHS CHILLY BALLA HS(G) RAM LAL 31 DODA BHATYAS HS TILOGRA HS ROMESH CHANDER 32 DODA BHATYAS HS CHAMPAL HS OM PARKASH 33 DODA BHATYAS HS KAHARA HS PIAR SINGH 34 DODA BHATYAS -
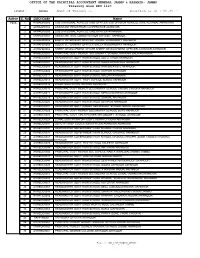
Treasury Wise DDO List Position As on : Name of Tresury
OFFICE OF THE PRINCIPAL ACCOUNTANT GENERAL JAMMU & KASHMIR- JAMMU Treasury wise DDO list Location : Jammu Name of Tresury :- Position as on : 09-JAN-17 Active S. No DDO-Code Name YES 1 AHBAGR0003 SUB DIVISIONAL AGRICULTURE OFFICER SUB DIVISION AGRICULTURE ACHABAL ANANTNAG 2 AKHAGR0002 ASSISTANT REGISTRAR COOPERATIVE AKHNOOR 3 AKHAGR0006 SUB DIVISIONAL AGRICULTURE OFFICER AKHNOOR . 4 AKHAGR0007 ASSISTANT SOIL CONSERVATION OFFICER AKHNOOR . 5 AKHAHD0002 BLOCK VETERINARY OFFICER ANIMAL HUSBANDRY AKHNOOR 6 AKHAHD0003 BLOCK VETERINARY OFFICER SHEEP HUSBANDARY AKHNOOR . 7 AKHAHD0004 SHEEP DEVELOPMENT OFICER SHEEP DEVELOPMENT OFFICER AKHNOOR AKHNOOR 8 AKHEDU0001 PRINCIPAL GOVT HIGHER SECONDARY SCHOOL NARRARI BALA AKHNOOR 9 AKHEDU0003 HEADMASTER GOVT HIGH SCHOOL KOTLI TANDA AKHNOOR 10 AKHEDU0004 HEADMASTER GOVT HIGH SCHOOL MAWA BRAHMANA AKHNOOR 11 AKHEDU0007 HEADMASTER GOVT HIGH SCHOOL RAH SALAYOTE AKHNOOR 12 AKHEDU0009 HEADMASTER GOVT HIGH SCHOOL KATHAR AKHNOOR 13 AKHEDU0011 HEADMASTER GOVT HIGH SCHOOL MALLAH AKHNOOR 14 AKHEDU0013 HEADMASTER GOVT HIGH SCHOOL SUNAIL AKHNOOR 15 AKHEDU0015 ZONAL EDUCATION OFFICER AKHNOOR . 16 AKHEDU0016 PRINCIPAL GOVT HIGHER SECONDARY SCHOOL CHOUKI CHOURA AKHNOOR 17 AKHEDU0017 HEADMASTER GOVT HIGH SCHOOL MERA MANDRIAN AKHNOOR 18 AKHEDU0018 HEADMASTER GOVT HIGH SCHOOL SUNGAL AKHNOOR 19 AKHEDU0020 HEADMASTER GOVT HIGH SCHOOL DEVIPUR AKHNOOR 20 AKHEDU0021 HEADMASTER GOVT HIGHER SECONDARY SCHOOL SOHAL AKHNOOR 21 AKHEDU0025 PRINCIPAL GOVT HIGHER SECONDARY SCHOOL BOYS AKHNOOR 22 AKHEDU0026 PRINCIPAL GOVT GIRLS HIGHER SECONDARY SCHOOL AKHNOOR 23 AKHEDU0028 ZONAL EDUCATION OFFICER CHOWKI CHOURA AKHNOOR 24 AKHEDU0031 DEPUTY CHIEF EDUCATION OFFICER AKHNOOR AKHNOOR 25 AKHEDU0034 HEADMASTER GOVERNMENT HIGH SCHOOL CHANG AKHNOOR . 26 AKHEDU0037 HEADMASTER GOVERNMENT HIGH SCHOOL GARKHAL AKHNOOR 27 AKHEDU0038 HEADMASTER GOVERNMENT HIGH SCHOOL DHANNA CHHAPRI (ZONE CHOWKI CHOURA) AKHNOOR 28 AKHEDU0039 HEADMASTER GOVT. -

December, 2019)
IMPLEMENTATION AND ALLOCATION OF BAR CODES TO HEALTH CARE FACILITIES IN JAMMU & KASHMIR PCB (December, 2019) Jammu & Kashmir Pollution Control Board Parivesh Bhawan, Gladni, Transport Nagar, Narwal, Jammu-180 006 Sheikh-ul -Alam Complex, Behind Govt. Silk Factory, Rajbagh,Srinagar -190 0008 https://jkspcb.nic.in E.mail: [email protected] Government of Jammu & Kashmir JAMMU & KASHMIR POLLUTION CONTROL BOARD IMPLEMENTATION OF BAR CODE SYSTEM IN HEALTH CARE FACILITIES AND COMMON BIO-MEDICAL WASTE TREATMENT FACILITES OF JAMMU & KASHMIR The Bio-medical Waste Management Rules, 2016 notified on 28.03.2016 and amended thereof on 16/3/2018, 19/2/2019 and 10/5/2019, respectively, under the Environment (Protection) Act, 1986, stipulates that it is the duty of every Health Care Facility (HCF) to establish a Bar Code system for bags or containers containing biomedical waste (BMW) to be sent out of the premises for further treatment and disposal in accordance with the guidelines issued by the Central Pollution Control Board, by 27.03.2019 [Rule-4 (i)]. Also, Rule 5 of the BMWM Rules, 2016 stipulates that it is the duty of every Operator of a Common Bio-medical Waste Treatment Facility (CBMWTF) to establish bar code system for handling of bio-medical waste in accordance with the guidelines issued by the Central Pollution Control Board, by 27.03.2019. “Guidelines for Bar Code System for Effective Management of Bio-medical Waste” prepared by Central Pollution Control Board, Delhi in April, 2018, is to facilitate and provide guidance to both the Occupier as well as Operator of CBMWTF to establish bar code system and also to have uniformity in adoption of the bar code system throughout the country, thereby ensuring effective enforcement of the BMWM Rules, 2016. -

IGP Says Slain Were Involved in Militancy, Will Convince Families with Concrete Evidence Abid Bashir Ed with Pistols and Grenades
10thyear of publication SRINAGAR OBSERVER Farooq urges LG to take steps for promotion NC Deputation, BDC Members Meet LG in Srinagar DDC Srinagar Convenes DLAC Meet On Food Safety of Surinsar as tourist destination Several deputations from political parties and members of the Block District Development Commissioner (DDC) Srinagar, Dr. Shahid Iqbal Development Council today called on Lieutenant Governor Manoj Sinha Chowdhary today convened a meeting of District Level Advisory Committee Emphasizing huge potential of the Surinsar Lake as a tourism destination, here for the redressal of grievances and other issues. A deputation of National Conference President and MP, Dr Farooq Abdullah today urged Lt. (DLAC) on Food Safety at Banquet Hall here. On the occasion, Assistant National Conference led by Member of Parliament, Hasnain Masoodi Commissioner, Food Safety Srinagar Hilal Ahmad Mir who is also the Governor Mr Manoj Sinha to have a plan in place in the larger interest of the and comprising former legislators, Altaf Ahmad Kaloo, | Page 05 local economy and promotion of tourism in the Jammu region. “We will Member Secretary of the committee, gave a detailed presentation. The take up the issue in Parliament, as also with the | Page 03 meeting was informed that from the date | Page 07 TUESDAY, 19 JANUARY 2021 05, Jamada-ul-Thani 1442 Hijri Published from Srinagar RNI No:JKENG/2012/43267 Vol:10 Issue No: 16 Pages:8 Rs.5.00 epaper: www.srinagarobserver.com LAWAYPORA ENCOUNTER Bodies Won’t Be Handed Over To Families Due To Pandemic: IGP Says slain were involved in militancy, will convince families with concrete evidence Abid Bashir ed with pistols and grenades. -

Aadhaar Enrolment Enabled Business Units
S.No Center Location 1 J&K Bank BU:Shalamar Road Block:Jammu ,district:Jammu 2 J&K Bank BU:Gandhi Nagar Block:Jammu ,district:Jammu 3 J&K Bank BU:Patel Nagar Block:Jammu ,district:Jammu 4 J&K Bank BU:Channi Himmat Block:Jammu ,district:Jammu 5 J&K Bank BU:Akhnoor Block:Akhnoor,district:Jammu 6 J&K Bank BU:Durga Nagar Block:jammu,district:Jammu 7 J&K Bank BU:Sidhra Block:Dansal ,district:Jammu 8 J&K Bank BU:Nagrota Block:Dansal ,district:Jammu 9 J&K Bank BU:Arnia Block:Bishnah,district:Jammu 10 J&K Bank BU:Khour Block:Khour,district:Jammu 11 J&K Bank BU:Bari brahamna Block:Bari Brahmna ,district:Samba 12 J&K Bank BU:Samba main Block:Samba ,district:Samba 13 J&K Bank BU:Dayalachak Block:Hiranagar,district:KATHUA 14 J&K Bank BU:Phinter Block:Bilawar,district:KATHUA 15 J&K Bank BU:Basoli Block:Basholi,district:KATHUA 16 J&K Bank BU:Kalibari Block:Hiranagar,district:KATHUA 17 J&K Bank BU:Doda Main Block:Doda ,district:Doda 18 J&K Bank BU: Seri Block:Thatri ,district:Doda 19 J&K Bank BU:Hidyal Block:Kishtwar ,district:Doda 20 J&K Bank BU:Kuleed Block:Kishtwar ,district:Doda 21 J&K Bank BU: Tethar Block:Banihal ,district:Doda 22 J&K Bank BU: Maitra Ramban Block:Ramban ,district:Ramban 23 J&K Bank BU: Cama Housing Colony Udhampur, Block:Udhampur ,district:Udhampur 24 J&K Bank BU:SMM Ramnagar,Udhampur Block:Udhampur ,district:Udhampur 25 J&K Bank BU: Rehambal, Udhampur Block:Udhampur,district:Udhampur 26 J&K Bank BU: Arli Katra, Reasi Block:Katra ,district:Reasi 27 J&K Bank BU: DC Office Reasi Block:Reasi ,district:Reasi 28 J&K Bank BU: Kheora -

Public Works Deptt
AADHAR BASED BIOMETRIC IDENTIFICATION AND SKILL PROFILING Reports Select Department :- PUBLIC WORKS DEPA Select District :- All Sno. District Name Parentage Address Present Office DOB Category MOHD NAZIR AHMAD CASUAL 1 ANANTNAG MUNAWAR RAKH CHANDIPORA PHG SUB DIVISION KULGAM 01-01-1987 SHEIKH LABOURERS SHEIKH HILAL AHMAD CASUAL 2 ANANTNAG GH NABI BHAT ZAWOORA BADARHAMA SHOPIAN SUB DIVISION PULWAMA 01-01-1985 DAR LABOURERS RAYEES AHMAD GH HASSAN CASUAL 3 ANANTNAG SOUF SHALI KOKERNAG SUB DIV KHANABAL 15-02-1991 MAKTOO MAKTOO LABOURERS MOHD ASLAM ABDUL RAZAQ CASUAL 4 ANANTNAG ARHAMA SUB DIV PULWAMA 02-03-1985 ITOO ITOO LABOURERS JAVAID AHMAD CASUAL 5 ANANTNAG AB RAZAK ARHAMA SHOPIAN SUB DIVISION PULWAMA 02-02-1986 ITOO LABOURERS FAYAZ AHMAD GH MOHI UD CASUAL 6 ANANTNAG AURBAGH PULWAMA SUB DIV PULWAMA 03-01-1986 BHAT BHAT LABOURERS ISHTIYAQ AHMAD FAROQQ WORK SHOP SUB DIVISION CASUAL 7 ANANTNAG S K COLONY ANG 15-08-1988 NANWAI AHMAD KHANBAL LABOURERS MOHD YOUSUF CASUAL 8 ANANTNAG GH HASSAN DOONIPAWA ANG SUB DIVISION KULGAM 01-04-1985 MALIK LABOURERS MUSHTAQ CASUAL http://10.149.2.27/abbisp/AdminReport/District_Wise.aspx[1/17/2018 2:32:43 PM] 9 ANANTNAG AHMAD AB GANI DANEW BOGUND SUB DIVISION KULGAM 01-04-1968 LABOURERS KHANDAY SHOWKAT GH HASSAN CASUAL 10 ANANTNAG PRICHOO PULWAMA PRICHOO PULWAMA 19-06-1989 AHMAD SHEIKH SHEIKH LABOURERS AB KHALIQ CASUAL 11 ANANTNAG ALI MOHD SHAH NEW COLONEY BIJBIHARA SUB DIV KHANABAL 25-03-1977 SHAH LABOURERS MOHD SHAFI NOOR MOHD CASUAL 12 ANANTNAG SEER HAMDAN PWD KHANABAL 22-11-1990 SHEIKH SHEIKH LABOURERS