Dear Students
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SLIAC Championships
TRXC Timing, LLC. - Contractor License HY-TEK's Meet Manager SLIAC Cross Country Championships - 10/29/2011 Entries and Results by TRXC Timing Highland, IL Last Completed Event Event 1 Women 6k Run CC ======================================================================= Name Year School Finals Points ======================================================================= 1 Powell, Casey FR Principia College 23:08 1 2 Koestner, Sarah FR Westminster College 23:32 2 3 Tonner, Alyssa SO Fontbonne College 24:09 3 4 Greenough, Julie SO Webster University 24:27 4 5 Litwiller, Sarah FR Principia College 24:33 5 6 Heisse, Heather SO Webster University 24:35 6 7 McKibben, Jane JR Webster University 24:36 7 8 Stackhouse, Eroica SO Webster University 24:38 8 9 Counts, Marielle SO Fontbonne College 24:41 9 10 Downey, Kaily SO Westminster College 24:46 10 11 West, Anna FR Westminster College 24:56 11 12 King, Janika FR Spalding University 25:04 13 Osborne, Emily FR Principia College 25:21 12 14 Cave, Samantha SO Spalding University 25:24 15 Morton, Haley FR Principia College 25:26 13 16 Suber, Julia FR Principia College 25:36 14 17 Ochoa, Kassandra FR Webster University 25:37 15 18 Ford, Suzanne FR Greenville College 25:42 16 19 Hamilton, Kelia SO Fontbonne College 25:46 17 20 Stiles, Sophia FR Greenville College 25:58 18 21 Przybylski, Jessica FR Greenville College 26:07 19 22 Schreck, Amanda FR Eureka College 26:21 20 23 Cheatham, Alyssa JR Principia College 26:33 21 24 Brock, Jessica SO Fontbonne College 26:44 22 25 Nelson, Rosie FR Greenville -

2008 Greater Louisville Cross Country Classic Hosted by the Greater Louisville Sports Commission E.P
2008 Greater Louisville Cross Country Classic (Men's Results) Page 1 of 14 2008 Greater Louisville Cross Country Classic Hosted by the Greater Louisville Sports Commission E.P. Tom Sawyer State Park — Louisville, KY (10/4/2008) Complete Men’s Results Gold Results | Blue Results --Gold Team Results | Gold Individual Results Event 1 Men’s 8k Gold Team Scores ================================================================================ Rank Team Total 1 2 3 4 5 *6 *7 *8 * ================================================================================ 1 Southern Illinois Univers 77 2 10 17 23 25 63 64 Total Time: 2:02:00.67 Average: 24:24.14 2 Eastern Kentucky Univ. 91 4 7 8 21 51 56 101 Total Time: 2:02:20.10 Average: 24:28.02 3 Rend Lake College 120 1 11 14 16 78 106 114 Total Time: 2:02:33.97 Average: 24:30.80 4 Univ. of Louisville 127 12 18 26 28 43 46 107 Total Time: 2:03:31.87 Average: 24:42.38 5 Univ. of Tennessee 218 24 32 34 40 88 98 110 Total Time: 2:05:06.44 Average: 25:01.29 6 Belmont University 224 22 38 45 54 65 71 104 Total Time: 2:05:25.39 Average: 25:05.08 7 Georgia State 233 6 36 60 61 70 100 137 Total Time: 2:05:20.36 Average: 25:04.08 8 Middle TN State Universit 251 13 39 57 67 75 Total Time: 2:05:36.45 Average: 25:07.29 9 East TN State Univ. 275 5 27 31 68 144 188 Total Time: 2:05:26.35 Average: 25:05.27 10 Univ. -
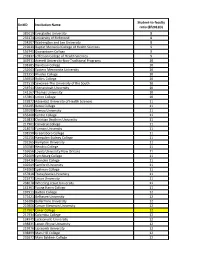
NCES Student Ratio Data
Student-to-faculty UnitID Institution Name ratio (EF2012D) 385619 Everglades University 8 233374 University of Richmond 8 234207 Washington and Lee University 8 219639 Baptist Memorial College of Health Sciences 9 156745 Georgetown College 9 231837 Jefferson College of Health Sciences 9 449931 Averett University-Non-Traditional Programs 10 198385 Davidson College 10 232043 Eastern Mennonite University 10 221351 Rhodes College 10 136950 Rollins College 10 221519 Sewanee-The University of the South 10 233541 Shenandoah University 10 141167 Thomas University 10 157863 Union College 10 133872 Adventist University of Health Sciences 11 156295 Berea College 11 139199 Brenau University 11 156408 Centre College 11 219833 Christian Brothers University 11 217961 Converse College 11 218070 Furman University 11 198598 Greensboro College 11 232256 Hampden-Sydney College 11 232265 Hampton University 11 107080 Hendrix College 11 159656 Loyola University-New Orleans 11 232609 Lynchburg College 11 233426 Roanoke College 11 102049 Samford University 11 141060 Spelman College 11 157818 Transylvania University 11 221971 Union University 11 238078 Wheeling Jesuit University 11 141361 Young Harris College 11 197911 Barton College 12 175421 Belhaven University 12 156286 Bellarmine University 12 219806 Carson-Newman University 12 217907 Coker College 12 217934 Columbia College 12 134945 Jacksonville University 12 198835 Lenoir-Rhyne University 12 219976 Lipscomb University 12 198899 Mars Hill College 12 232672 Mary Baldwin College 12 220710 Maryville College -

Women's D III 25% Schedule Rule
Women's NCAA Division III Percentages 06-06-2021 SCHOOL Reg Conf TOT PCT. SCHOOL Reg Conf TOT PCT. SCHOOL Reg Conf TOT PCT. Adrian College (MH)............ 74 0 79 94% Colby College ....................... 0 0 0 0% Gustavus Adolphus C. (MN) 25 0 26 96% Albion College (MH)............ 54 0 54 100% Concordia College-MN 11 0 12 92% Hamilton College (NS) ......... 16 0 17 94% Albright College (M3) .......... 0 0 0 0% (MN)...................................... Hanover College (H3)........... 33 0 34 97% Allegheny College (NC) ....... 12 0 19 63% Concordia University (TX) 21 0 23 91% Hardin-Simmons University 21 0 24 88% Alma College (MH) .............. 54 0 54 100% (AS)....................................... (AS)....................................... Alvernia University (M3)...... 32 0 43 74% Concordia University WI 58 0 70 83% Hastings College ................... 0 0 0 0% (NO) ...................................... Alverno College (NO)........... 0 0 0 0% Heidelberg University (OA).. 0 0 0 0% Cornell College ..................... 0 0 0 0% Amherst College (NS)........... 17 0 17 100% Hendrix College (S2) ............ 0 0 0 0% Cortland State (N3) ............... 14 0 17 82% Anderson University (IN) 0 0 0 0% Hiram College (NC).............. 0 0 0 0% (H3) ....................................... Covenant College.................. 0 0 0 0% Hollins University................. 0 0 0 0% Arcadia University (M3)....... 32 0 38 84% Crown College (UM) ............ 0 0 0 0% Hood College (M3) ............... 1 0 1 100% Augsburg College ................. 0 0 0 0% Dallas, University of ............. 0 0 0 0% Hope College (MH) .............. 40 0 40 100% Augsburg University (MN)... 0 0 0 0% Defiance College (H3) .......... 22 0 27 81% Houghton College ................. 0 0 0 0% Augustana College (IW) ...... -

Brescia University Vs. IU Southeast
INDIANA UNIVERSITY SOUTHEAST GRENADIERS - VOLLEYBALL GAME PROGRAM - Brescia University vs. IU Southeast Tuesday, October 6, 2009 Match Time: 7:00 PM ET PROBABLE STARTERS - IU Southeast Grenadier Volleyball 2009 Grenadier Volleyball Schedule Date Opponent Time (EDT)/Results IU Southeast (10-7) Ht. Yr. Pos. Hometown 1 Lindsey MAYMON 5’6” FR OH Sellersburg, Ind. AUGUST 3 Lindsey RUMPH 5’5” SO OH Brownstown, Ind. Fri. 21 Cedarville University W 3-1 4 Pamela COCKERELL 6’0” FR MB Corydon, Ind. Fri. 21 IU East L 3-1 Sat. 22 Grace (Ind.) College W 3-0 5 Kara DRAPER 5’6” SR OS La Grange, Ky. Sat. 22 Huntington University L 3-1 6 Vanessa STAUBLE 6’0” SR MB Louisville, Ky. Wed. 26 ASBURY COLLEGE* W 3-1 8 Stacey FLATT 5’4” SR SET Louisville, Ky. 10 Lauren McCARTIN 5’6” SO LIB Floyds Knobs, Ind. SEPTEMBER Tues. 1 LINDSEY WILSON W 3-1 GRENADIER VOLLEYBALL QUICK FACTS VOLLEYBALL COACHING STAFF Thurs. 3 CAMPBELLSVILLE L 3-1 Location……………………………..New Albany, IN 47150 Wed. 9 Spalding University W 3-1 Founded (Indiana University)…………………………1820 Volleyball Head Coach: Lesley Drury Prather Fri. 11 St. Francis L 3-0 Enrollment……………………………………………...6,840 (University of Louisville, ’05) Fri. 11 IU East L 3-2 Nickname………………………………………….Grenadiers Colors……………………………………Crimson and Cream Sat. 12 Saint Xavier University L 3-1 Record at IU Southeast: 10-7 (1st Year) Sat. 12 Cedarville University W 3-2 Conference……….Kentucky Intercollegiate Athletic (KIAC) Overall Record: 10-7 (1st Year) Home Court………………………………Activities Building Thurs. 17 Oakland City University L 3-1 President………………………….Dr. -

Sept. 12 Virtualcollegefairs.Org
Find the college for you! Sept. 12 virtualcollegefairs.org Sign up now at virtualcollegefairs.org and start tagging the colleges you’re interested in! Then, log in on September 12 for the chance to connect with hundreds of colleges. College advisers will be available that day to share information about majors, scholarships, and more. Attend Zoom sessions, text your questions, and demonstrate interest… all without leaving home. See you on September 12! Alabama Fresno Pacific University-Pueblo Rollins College DePaul University University of Alabama State University Fort Lewis College The University of Dominican University Massachusetts University Amherst Humboldt State University of Colorado Tampa Northwestern University Auburn University University Boulder University of Central Wentworth Institute of Quincy University Technology Samford University Laguna College of Art University of Northern Florida and Design Roosevelt University Wheaton College The University of Colorado University of Florida Saint Xavier University Alabama Los Angeles College of Western Colorado University of Miami Worcester Polytechnic Music Southern Illinois Institute University of Alabama University University of North University at Birmingham Loyola Marymount Florida University Carbondale Maine Connecticut University of South University of Illinois at University of New Alaska Saint Mary’s College of Central Connecticut Florida Chicago England University of Alaska California State University Anchorage Santa Clara University Sacred Heart University University of Southern -

A Stronger Bottom Line
A Stronger Bottom Line Association of Independent Kentucky Colleges and Universities Comparing Costs, Growth Potential of Kentucky’s Independent Colleges & Universities AIKCU member colleges and universities are complex, nonprofit organizations that are in the business of changing lives and communities. And like the leaders of any business, college leaders need access to accurate, organized, and insight-producing data to make good strategic decisions in an increasingly complex environment. This need is what led AIKCU leaders to partner with The Higher Education Practice LLC, led by Kenneth L. Hoyt, Ph.D., to conduct the Optimizing Academic Balance (OAB) comparative study. This is the first time that a group of similar institutions has gone through this process together, providing a critical but previously unavailable opportunity for benchmarking academic program costs and productivity. We are pleased that 13 of 18 AIKCU member institutions were able to complete the process. The participating campus leaders now have access to rich data that helps them understand the true economics of their academic programs and, importantly, how they stack up to similar institutions across the state. Having this information will aid their decision-making as they strive to maximize their limited resources to better serve students and their communities. We are extremely grateful to the James Graham Brown Foundation for its financial support of this project and its long history of supporting educational initiatives in the Commonwealth. We also want to thank the staff on our participating campuses for the time and energy they dedicated to mining their data systems and cleaning data in preparation for the OAB analysis. -

Men's NCAA Division III Percentages 06-04-2021
Men's NCAA Division III Percentages 06-04-2021 SCHOOL Reg Conf TOT PCT. SCHOOL Reg Conf TOT PCT. SCHOOL Reg Conf TOT PCT. Adrian College (MH)............ 61 0 64 95% Cazenovia College ................ 0 0 0 0% Emory and Henry College 14 0 28 50% Albertus Magnus College 11 0 40 28% Centenary College (U5) ........ 18 0 30 60% (OD) ...................................... (GN) ...................................... Centenary College NJ (CS)... 0 0 0 0% Emory University (UN) ........ 60 0 92 65% Albion College (MH)............ 54 0 54 100% Central College (IA) (II) ....... 47 0 93 51% Endicott College (C1) ........... 12 0 12 100% Albright College (CW).......... 47 0 47 100% Centre College (S2)............... 34 0 41 83% Eureka College (ST).............. 11 0 11 100% Allegheny College (NC) ....... 24 0 25 96% Chapman University (S1)...... 10 0 10 100% Farmingdale State (SY)......... 34 0 57 60% Alma College (MH) .............. 54 0 54 100% Christopher Newport (CP) .... 72 0 90 80% FDU-Florham (FC) ............... 33 0 33 100% Alvernia University (CW)..... 52 0 52 100% Claremont Mudd Scripps 0 0 0 0% Ferrum College (OD)............ 65 0 68 96% Amherst College (NS)........... 21 0 21 100% (S1)........................................ Finlandia University.............. 0 0 0 0% Anderson University (H3)..... 0 0 0 0% Clarks Summit University 3 0 3 100% Fontbonne University (ST) ... 26 0 43 60% Anna Maria College.............. 0 0 0 0% (CS) ....................................... Franklin & Marshall (CC)..... 34 0 58 59% Arcadia University (CW)...... 46 0 46 100% Clarkson University (LL)...... 17 0 17 100% Franklin College (H3) ........... 50 0 54 93% Augsburg University (MN)... 33 0 33 100% Coe College (II) ................... -

Faculty Faculty
Faculty Faculty • Lopez, Luis M., BA, University Arkansas Little Rock, 2015; MPA, University Arkansas Little Rock, 2017 Adjunct faculty are assigned the title of adjunct professor. • Metzger, James E., BA, University Notre Dame, 1971; MA, University Chicago, 1975 Adjunct faculty can be characterized as follows: • Perkins, Veronica D., BS, University Arkansas Pine Bluff, 1994; MS, University Arkansas Pine Bluff, 1998; EdD, • They teach for Webster University on a continuing basis. Arkansas State University, 2009 • They attend faculty meetings. • Rhodes, Deaundra M., BA, University Arkansas Pine • They attend institutes and workshops for adjunct faculty. Bluff, 1997; MA, Webster University, 2000; EdD, Walden • They are evaluated by students at the end of each course University, 2012 taught. • Sample, Gary L., BS, University Arkansas Little Rock, 1995; • They submit course syllabi prior to the beginning of classes. MS, University Arkansas Fayetteville, 1996 • They participate in curriculum design through workshops and • Smith, Gary W., BS, University Southern Mississippi, 1970; faculty meetings. MHA, Washington University, 1974 Part-time faculty are persons who are not fully employed by • Sweeden, Joseph P., BA, University Arkansas Little Rock, Webster University but teach courses for Webster University. 1989; MA, University Arkansas Little Rock, 1993 • Villines, Justin J., BS, University Phoenix, 2009; MBA, U.S. Campuses University Phoenix, 2010 • Volpe, Joseph J., BS, U.S. Military Academy, 1988; JD, Arizona University Arkansas Little -

Bearcat Hoinke Classic January 12, 2014 TEAM STANDINGS | VARSITY - Women
Bearcat Hoinke Classic January 12, 2014 TEAM STANDINGS | VARSITY - Women NO TEAM NAME TEAM BKR TOTAL GM AVG DIFF 1. Lindenwood University 5848 3999 9847 10.0 984.700 2. Martin Methodist College 5734 4036 9770 10.0 977.000 -77 3. Wright State University 5985 3730 9715 10.0 971.500 -132 4. Huntington University 5860 3731 9591 10.0 959.100 -256 5. Bowling Green State Univ. 5936 3620 9556 10.0 955.600 -291 6. Campbellsville University 5582 3866 9448 10.0 944.800 -399 7. Ursuline College 5707 3716 9423 10.0 942.300 -424 8. Urbana University 5728 3688 9416 10.0 941.600 -431 9. Bellarmine University 5652 3600 9252 10.0 925.200 -595 10. Lindenwood University-Belleville 5235 3775 9010 10.0 901.000 -837 11. Morehead State University 5084 3526 8610 10.0 861.000 -1237 12. Youngstown State University 5136 3426 8562 10.0 856.200 -1285 13. Northern Kentucky University 5085 3312 8397 10.0 839.700 -1450 14. Spalding University 4792 3290 8082 10.0 808.200 -1765 15. Louisville /University of 4704 3141 7845 10.0 784.500 -2002 16. Lindsey Wilson College 4612 3107 7719 10.0 771.900 -2128 Event Field Average = 901.519 Games Bowled - 6 Team / 20 Baker NO NAME SCHOOL TM TOTAL GM AVG 1. Laglia, Regina Martin Methodist Var 1358 6 226.3333 2. Meadows, Kayla Bowling Green State Var 1323 6 220.5000 3. Griffith, Casandra Huntington Var 1307 6 217.8333 4. Johnson, Samantha Lindenwood Var 1298 6 216.3333 5. -

The Association for Student Affairs at Catholic Colleges and Universities 1996– 2009: Building a Community of Practice
The Association for Student Affairs at Catholic Colleges and Universities 1996– 2009: Building a Community of Practice Sandra M. Estanek, Ph.D. Abstract This article provides a history of the founding and maturation of the Associa- tion for Student Affairs at Catholic Colleges and Universities (ASACCU). It is the story of a group of lay and ordained student affairs professionals from Catholic colleges and universities who were inspired by the vision of Gaudium et spes1 and Ex corde Ecclesiae2 to take the initiative to create a community of practice among their peers. In 2014, ASACCU celebrated its fi fteenth anniver- sary as a national organization. Utilizing archival material and interviews with the founders, this article provides a history of ASACCU’s founding and fi rst ten years. Student affairs professionals at universities and colleges work with students as individuals and in groups in many educational envi- ronments outside the classroom. These professionals supervise resi- dence halls; they advise student organizations and work with student identity groups; they organize leadership development activities; they provide programming on campus on a variety of topics; they provide career counseling and academic advising. At Catholic colleges and uni- versities, these varied responsibilities often put student affairs profes- sionals in the midst of some of the most diffi cult and controversial issues: How should issues of sexual behavior be addressed? What rules should be in place in residence halls? Who should be permitted to speak on campus? Should an LGBT student organization be offi cially Sandra M. Estanek, Ph.D., is Professor of Graduate Education and Leadership at Canisius College, Buffalo, New York. -

2019-20 Ncaa Division Iii Women's Volleyball Pools
2019-20 NCAA DIVISION III WOMEN’S VOLLEYBALL POOLS CENTRAL REGION (Rank 8) Pool A Conferences (5) InstItutIons In AQ Conferences (41) Pool B Independents (0) AmerIcan Rivers Conference (9) Buena Vista University Central College (Iowa) Coe College University of Dubuque Loras College Luther College Nebraska Wesleyan University Simpson College AQ – Conference Championship Wartburg College Minnesota IntercollegIate AthletIc Augsburg University Conference (12) Bethel University (Minnesota) Carleton College Concordia College, Moorhead Gustavus Adolphus College Hamline University Macalester College College of Saint Benedict St. Catherine University Saint Mary’s University of Minnesota St. Olaf College AQ – Conference Championship University of St. Thomas (Minnesota) St. Louis Intercollegiate AthletIc Blackburn College Conference (10) Eureka College Fontbonne University Greenville University Iowa Wesleyan University MacMurray College Principia College Spalding University Webster University AQ – Conference Championship Westminster College (Missouri) UnIversIty AthletIc AssocIatIon (1^) Washington University in St. Louis AQ – Conference Championship Upper MIdwest AthletIc Conference (9) Bethany Lutheran College Crown College (Minnesota) Martin Luther College University of Minnesota, Morris North Central University Northland College University of Northwestern – St. Paul The College of St. Scholastica AQ – Conference Championship University of Wisconsin-Superior ^University Athletic Association is listed in Pool A in seven regions. GREAT LAKES REGION