KDM2B Promotes Cell Viability by Enhancing DNA Damage Response in Canine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Structural Basis for Selective Binding of Non-Methylated Cpg Islands by the CFP1 CXXC Domain
ARTICLE Received 13 Dec 2010 | Accepted 9 Feb 2011 | Published 8 Mar 2011 DOI: 10.1038/ncomms1237 The structural basis for selective binding of non-methylated CpG islands by the CFP1 CXXC domain Chao Xu1,*, Chuanbing Bian1,*, Robert Lam1, Aiping Dong1 & Jinrong Min1,2 CFP1 is a CXXC domain-containing protein and an essential component of the SETD1 histone H3K4 methyltransferase complex. CXXC domain proteins direct different chromatin-modifying activities to various chromatin regions. Here, we report crystal structures of the CFP1 CXXC domain in complex with six different CpG DNA sequences. The crescent-shaped CFP1 CXXC domain is wedged into the major groove of the CpG DNA, distorting the B-form DNA, and interacts extensively with the major groove of the DNA. The structures elucidate the molecular mechanism of the non-methylated CpG-binding specificity of the CFP1 CXXC domain. The CpG motif is confined by a tripeptide located in a rigid loop, which only allows the accommodation of the non-methylated CpG dinucleotide. Furthermore, we demonstrate that CFP1 has a preference for a guanosine nucleotide following the CpG motif. 1 Structural Genomics Consortium, University of Toronto, 101 College Street, Toronto, Ontario M5G 1L7, Canada. 2 Department of Physiology, University of Toronto, Toronto, Ontario M5S 1A8, Canada. *These authors contributed equally to this work. Correspondence and requests for materials should be addressed to J.M. (email: [email protected]). NATURE COMMUNICATIONS | 2:227 | DOI: 10.1038/ncomms1237 | www.nature.com/naturecommunications © 2011 Macmillan Publishers Limited. All rights reserved. ARTICLE NATURE COMMUNICATIONS | DOI: 10.1038/ncomms1237 pG islands contain a high density of CpG content and embrace the promoters of most genes in vertebrate genomes1. -

The Histone Demethylase KDM2B Regulates Human Primordial Germ
Int. J. Biol. Sci. 2021, Vol. 17 527 Ivyspring International Publisher International Journal of Biological Sciences 2021; 17(2): 527-538. doi: 10.7150/ijbs.55873 Research Paper The histone demethylase KDM2B regulates human primordial germ cell-like cells specification Weiyan Yuan1,#, Zhaokai Yao1,#, Veeramohan Veerapandian1,2,#, Xinyan Yang1, Xiaoman Wang1,3, Dingyao Chen1, Linzi Ma1, Chaohui Li1,2, Yi Zheng1, Fang Luo1, Xiao-yang Zhao1,4,5,6,7 1. State Key Laboratory of Organ Failure Research, Department of Developmental Biology, School of Basic Medical Sciences, Southern Medical University, Guangzhou, Guangdong, China 2. Shunde Hospital of Southern Medical University, Shunde, Guangdong, China 3. Shenzhen Hospital of Southern Medical University, Shenzhen, Guangdong, China 4. Bioland Laboratory (Guangzhou Regenerative Medicine and Health Guangdong Laboratory), Guangzhou, China 5. Sino-America Joint Research Center for Translational Medicine in Developmental Disabilities 6. Department of Gynecology, Zhujiang Hospital, Southern Medical University, Guangzhou, Guangdong, China 7. National Clinical Research Center for Kidney Disease, Guangzhou, China # These authors contributed equally to this study Corresponding authors: Fang Luo ([email protected]), Xiao-Yang Zhao ([email protected]) © The author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2020.11.13; Accepted: 2020.12.12; Published: 2021.01.01 Abstract Germline specification is a fundamental step for human reproduction and this biological phenomenon possesses technical challenges to study in vivo as it occurs immediately after blastocyst implantation. The establishment of in vitro human primordial germ cell-like cells (hPGCLCs) induction system allows sophisticated characterization of human primordial germ cells (hPGCs) development. -

An Atypical 12Q24.31 Microdeletion Implicates Six Genes Including A
Hum Genet DOI 10.1007/s00439-016-1668-4 ORIGINAL INVESTIGATION An atypical 12q24.31 microdeletion implicates six genes including a histone demethylase KDM2B and a histone methyltransferase SETD1B in syndromic intellectual disability Jonathan D. J. Labonne1,2 · Kang‑Han Lee3 · Shigeki Iwase4 · Il‑Keun Kong5 · Michael P. Diamond1 · Lawrence C. Layman1,2,6 · Cheol‑Hee Kim3 · Hyung‑Goo Kim1,2 Received: 13 November 2015 / Accepted: 31 March 2016 © Springer-Verlag Berlin Heidelberg 2016 Abstract Microdeletion syndromes are frequent causes by synteny analysis revealing the conservation of the order of neuropsychiatric disorders leading to intellectual dis- of these six candidate genes between humans and zebrafish. ability as well as autistic features accompanied by epilepsy Among them, we propose histone demethylase KDM2B and craniofacial anomalies. From comparative deletion and histone methyltransferase SETD1B as the two most mapping of the smallest microdeletion to date at 12q24.31, plausible candidate genes involved in intellectual disabil- found in a patient with overlapping clinical features of ity, autism, epilepsy, and craniofacial anomalies. These two 12q24.31 microdeletion syndrome, we narrowed the puta- chromatin modifiers located approximately 224 kb apart tive critical region to 445 kb containing seven genes, one were both commonly deleted in six patients, while two microRNA, and one non-coding RNA. Zebrafish in situ additional patients had either KDM2B or SETD1B deleted. hybridization and comprehensive transcript analysis of The four additional candidate genes (ORAI1, MORN3, annotated genes in the panels of human organ and brain TMEM120B, RHOF), a microRNA MIR548AQ, and a non- suggest that these are all candidates for neurological phe- coding RNA LINC01089 are localized between KDM2B notypes excluding the gene HPD. -

Intrinsic Disorder of the BAF Complex: Roles in Chromatin Remodeling and Disease Development
International Journal of Molecular Sciences Article Intrinsic Disorder of the BAF Complex: Roles in Chromatin Remodeling and Disease Development Nashwa El Hadidy 1 and Vladimir N. Uversky 1,2,* 1 Department of Molecular Medicine, Morsani College of Medicine, University of South Florida, 12901 Bruce B. Downs Blvd. MDC07, Tampa, FL 33612, USA; [email protected] 2 Laboratory of New Methods in Biology, Institute for Biological Instrumentation of the Russian Academy of Sciences, Federal Research Center “Pushchino Scientific Center for Biological Research of the Russian Academy of Sciences”, Pushchino, 142290 Moscow Region, Russia * Correspondence: [email protected]; Tel.: +1-813-974-5816; Fax: +1-813-974-7357 Received: 20 September 2019; Accepted: 21 October 2019; Published: 23 October 2019 Abstract: The two-meter-long DNA is compressed into chromatin in the nucleus of every cell, which serves as a significant barrier to transcription. Therefore, for processes such as replication and transcription to occur, the highly compacted chromatin must be relaxed, and the processes required for chromatin reorganization for the aim of replication or transcription are controlled by ATP-dependent nucleosome remodelers. One of the most highly studied remodelers of this kind is the BRG1- or BRM-associated factor complex (BAF complex, also known as SWItch/sucrose non-fermentable (SWI/SNF) complex), which is crucial for the regulation of gene expression and differentiation in eukaryotes. Chromatin remodeling complex BAF is characterized by a highly polymorphic structure, containing from four to 17 subunits encoded by 29 genes. The aim of this paper is to provide an overview of the role of BAF complex in chromatin remodeling and also to use literature mining and a set of computational and bioinformatics tools to analyze structural properties, intrinsic disorder predisposition, and functionalities of its subunits, along with the description of the relations of different BAF complex subunits to the pathogenesis of various human diseases. -

X- and Y-Linked Chromatin-Modifying Genes As Regulators of Sex-Specific Cancer Incidence and Prognosis
Author Manuscript Published OnlineFirst on July 30, 2020; DOI: 10.1158/1078-0432.CCR-20-1741 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. X- and Y-linked chromatin-modifying genes as regulators of sex- specific cancer incidence and prognosis Rossella Tricarico1,2,*, Emmanuelle Nicolas1, Michael J. Hall 3, and Erica A. Golemis1,* 1Molecular Therapeutics Program, Fox Chase Cancer Center, Philadelphia, PA, 19111, USA; 2Department of Biology and Biotechnology, University of Pavia, 27100 Pavia, Italy; 3Cancer Prevention and Control Program, Department of Clinical Genetics, Fox Chase Cancer Center, Philadelphia, PA, 19111, USA Running title: Allosomally linked epigenetic regulators in cancer Conflict Statement: The authors declare no conflict of interest. Funding: The authors are supported by NIH DK108195 and CA228187 (to EAG), by NCI Core Grant CA006927 (to Fox Chase Cancer Center), and by a Marie Curie Individual Fellowship from the Horizon 2020 EU Program (to RT). * Correspondence should be directed to: Erica A. Golemis Fox Chase Cancer Center 333 Cottman Ave. Philadelphia, PA 19111 USA [email protected] (215) 728-2860 or Rossella Tricarico Department of Biology and Biotechnology University of Pavia Via Ferrata 9, 27100 Pavia, Italy [email protected] +39 340-2429631 1 Downloaded from clincancerres.aacrjournals.org on September 25, 2021. © 2020 American Association for Cancer Research. Author Manuscript Published OnlineFirst on July 30, 2020; DOI: 10.1158/1078-0432.CCR-20-1741 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract Biological sex profoundly conditions organismal development and physiology, imposing wide-ranging effects on cell signaling, metabolism, and immune response. -
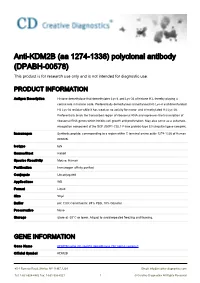
Anti-KDM2B (Aa 1274-1336) Polyclonal Antibody (DPABH-00578) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-KDM2B (aa 1274-1336) polyclonal antibody (DPABH-00578) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description Histone demethylase that demethylates Lys-4 and Lys-36 of histone H3, thereby playing a central role in histone code. Preferentially demethylates trimethylated H3 Lys-4 and dimethylated H3 Lys-36 residue while it has weak or no activity for mono- and tri-methylated H3 Lys-36. Preferentially binds the transcribed region of ribosomal RNA and represses the transcription of ribosomal RNA genes which inhibits cell growth and proliferation. May also serve as a substrate- recognition component of the SCF (SKP1-CUL1-F-box protein)-type E3 ubiquitin ligase complex. Immunogen Synthetic peptide, corresponding to a region within C terminal amino acids 1274-1336 of Human KDM2B. Isotype IgG Source/Host Rabbit Species Reactivity Mouse, Human Purification Immunogen affinity purified Conjugate Unconjugated Applications WB Format Liquid Size 50 μl Buffer pH: 7.00; Constituents: 89% PBS, 10% Glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name KDM2B lysine (K)-specific demethylase 2B [ Homo sapiens ] Official Symbol KDM2B 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Synonyms KDM2B; lysine (K)-specific demethylase 2B; F box and leucine rich repeat protein 10; FBXL10; lysine-specific demethylase -

The Emerging Role of Histone Lysine Demethylases in Prostate Cancer
Crea et al. Molecular Cancer 2012, 11:52 http://www.molecular-cancer.com/content/11/1/52 REVIEW Open Access The emerging role of histone lysine demethylases in prostate cancer Francesco Crea1*, Lei Sun3, Antonello Mai4, Yan Ting Chiang1, William L Farrar3, Romano Danesi2 and Cheryl D Helgason1,5* Abstract Early prostate cancer (PCa) is generally treatable and associated with good prognosis. After a variable time, PCa evolves into a highly metastatic and treatment-refractory disease: castration-resistant PCa (CRPC). Currently, few prognostic factors are available to predict the emergence of CRPC, and no curative option is available. Epigenetic gene regulation has been shown to trigger PCa metastasis and androgen-independence. Most epigenetic studies have focused on DNA and histone methyltransferases. While DNA methylation leads to gene silencing, histone methylation can trigger gene activation or inactivation, depending on the target amino acid residues and the extent of methylation (me1, me2, or me3). Interestingly, some histone modifiers are essential for PCa tumor- initiating cell (TIC) self-renewal. TICs are considered the seeds responsible for metastatic spreading and androgen- independence. Histone Lysine Demethylases (KDMs) are a novel class of epigenetic enzymes which can remove both repressive and activating histone marks. KDMs are currently grouped into 7 major classes, each one targeting a specific methylation site. Since their discovery, KDM expression has been found to be deregulated in several neoplasms. In PCa, KDMs may act as either tumor suppressors or oncogenes, depending on their gene regulatory function. For example, KDM1A and KDM4C are essential for PCa androgen-dependent proliferation, while PHF8 is involved in PCa migration and invasion. -

Interplay Between Cofactors and Transcription Factors in Hematopoiesis and Hematological Malignancies
Signal Transduction and Targeted Therapy www.nature.com/sigtrans REVIEW ARTICLE OPEN Interplay between cofactors and transcription factors in hematopoiesis and hematological malignancies Zi Wang 1,2, Pan Wang2, Yanan Li2, Hongling Peng1, Yu Zhu2, Narla Mohandas3 and Jing Liu2 Hematopoiesis requires finely tuned regulation of gene expression at each stage of development. The regulation of gene transcription involves not only individual transcription factors (TFs) but also transcription complexes (TCs) composed of transcription factor(s) and multisubunit cofactors. In their normal compositions, TCs orchestrate lineage-specific patterns of gene expression and ensure the production of the correct proportions of individual cell lineages during hematopoiesis. The integration of posttranslational and conformational modifications in the chromatin landscape, nucleosomes, histones and interacting components via the cofactor–TF interplay is critical to optimal TF activity. Mutations or translocations of cofactor genes are expected to alter cofactor–TF interactions, which may be causative for the pathogenesis of various hematologic disorders. Blocking TF oncogenic activity in hematologic disorders through targeting cofactors in aberrant complexes has been an exciting therapeutic strategy. In this review, we summarize the current knowledge regarding the models and functions of cofactor–TF interplay in physiological hematopoiesis and highlight their implications in the etiology of hematological malignancies. This review presents a deep insight into the physiological and pathological implications of transcription machinery in the blood system. Signal Transduction and Targeted Therapy (2021) ;6:24 https://doi.org/10.1038/s41392-020-00422-1 1234567890();,: INTRODUCTION by their ATPase subunits into four major families, including the Hematopoiesisisacomplexhierarchicaldifferentiationprocessthat SWI/SNF, ISWI, Mi-2/NuRD, and INO80/SWR1 families. -

KDM2B Is a Histone H3K79 Demethylase and Induces
bioRxiv preprint doi: https://doi.org/10.1101/228379; this version posted December 4, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 KDM2B is a histone H3K79 demethylase and induces 2 transcriptional repression via SIRT1-mediated chromatin silencing 3 4 Joo-Young Kang1, Ji-Young Kim1, Kee-Beom Kim1, Jin Woo Park1, Hana Cho1, Ja Young Hahm1, 5 Yun-Cheol Chae1, Daehwan Kim1, Hyun Kook2, Sangmyung Rhee1, Nam-Chul Ha3, Sang-Beom Seo1* 6 7 1Department of Life Science, College of Natural Sciences, Chung-Ang University, Seoul 156-756, 8 Republic of Korea 9 2Medical Research Center for Gene Regulation and Department of Pharmacology, Chonnam National 10 University, Gwangju 501-746, Republic of Korea 11 3Department of Food and Animal Biotechnology, Department of Agricultural Biotechnology, Seoul 12 National University, Seoul 151-921, Republic of Korea 13 *For correspondence: [email protected] 14 15 Abstract 16 The methylation of histone H3 lysine 79 (H3K79) is an active chromatin marker and is prominant in 17 actively transcribed regions of the genome. However, demethylase of H3K79 remains unknown 18 despite intensive research. Here, we show that KDM2B (also known as FBXL10), a member of the 19 Jumonji C family of proteins and known for its histone H3K36 demethylase activity, is a di- and tri- 20 methyl H3K79 demethylase. We demonstrate that KDM2B induces transcriptional repression of 21 HOXA7 and MEIS1 via occupancy of promoters and demethylation of H3K79. -

Human Transcription Factors Responsive to Initial Reprogramming Predominantly Undergo Legitimate Reprogramming During Fbroblast Conversion to Ipscs Ricardo R
www.nature.com/scientificreports OPEN Human transcription factors responsive to initial reprogramming predominantly undergo legitimate reprogramming during fbroblast conversion to iPSCs Ricardo R. Cevallos1, Yvonne J. K. Edwards1,2, John M. Parant3, Bradley K. Yoder2 & Kejin Hu1* The four transcription factors OCT4, SOX2, KLF4, and MYC (OSKM) together can convert human fbroblasts to induced pluripotent stem cells (iPSCs). It is, however, perplexing that they can do so only for a rare population of the starting cells with a long latency. Transcription factors (TFs) defne identities of both the starting fbroblasts and the end product, iPSCs, and are also of paramount importance for the reprogramming process. It is critical to upregulate or activate the iPSC-enriched TFs while downregulate or silence the fbroblast-enriched TFs. This report explores the initial TF responses to OSKM as the molecular underpinnings for both the potency aspects and the limitation sides of the OSKM reprogramming. The authors frst defned the TF reprogramome, i.e., the full complement of TFs to be reprogrammed. Most TFs were resistant to OSKM reprogramming at the initial stages, an observation consistent with the inefciency and long latency of iPSC reprogramming. Surprisingly, the current analyses also revealed that most of the TFs (at least 83 genes) that did respond to OSKM induction underwent legitimate reprogramming. The initial legitimate transcriptional responses of TFs to OSKM reprogramming were also observed in the reprogramming fbroblasts from a diferent individual. Such early biased legitimate reprogramming of the responsive TFs aligns well with the robustness aspect of the otherwise inefcient and stochastic OSKM reprogramming. OCT4, SOX2, KLF4, and MYC (collectively OSKM) can convert human fbroblasts into induced pluripotent stem cells (iPSCs), which are the man-made version of embryonic stem cells (ESCs)1–3. -

C-JUN and ITS TARGETS in FIBROSARCOMA and MELANOMA CELLS
c-JUN AND ITS TARGETS IN FIBROSARCOMA AND MELANOMA CELLS Mari Kielosto Medicum Department of Pathology Faculty of Medicine Doctoral Programme in Integrative Life Science and Faculty of Biological and Environmental Sciences University of Helsinki Finland Academic Dissertation To be presented for public examination, with permission of the Faculty of Biological and Environmental Sciences of the University of Helsinki, in Lecture Hall 2 of Metsätalo building (Unioninkatu 40, Helsinki), on 06.11.2020 at 12 noon. Helsinki 2020 Supervisor Docent Erkki Hölttä, MD, PhD Abnormal MAPK signaling has been implicated in human malignancies. Thus, the MAPK pathways Faculty of Medicine need to be tightly regulated. The MAPK phosphatases (MKPs), also known as dual specificity University of Helsinki phosphatases (DUSPs), are a family of proteins functioning as major negative regulators of MAPKs. Dephosphorylation of threonine and/or tyrosine residues within the Thr-X-Tyr motif located in the Thesis committee Professor Antti Vaheri, MD, PhD Faculty of Medicine MAPK activation loop inactivates MAPKs. Further, the MKPs/DUSPs have also been implicated in University of Helsinki the development of cancers (reviewed in Low and Zhang, 2016; Kidger and Keyse, 2016). Professor Jim Schröder, PhD Faculty of Biological and Environmental Sciences University of Helsinki Reviewers Docent Jarmo Käpylä, PhD Department of Biochemistry University of Turku Docent Päivi Koskinen, PhD Department of Biology University of Turku Opponent Docent Liisa Nissinen, PhD Department of Dermatology and Venereology University of Turku Custos Professor Juha Partanen, PhD Faculty of Biological and Environmental Sciences University of Helsinki The Faculty of Biological and Environmental Sciences uses the Urkund system (plagiarism recognition) to examine all doctoral dissertations. -

The H3K4 Methyltransferase Setd1b Is Essential for Hematopoietic Stem and Progenitor Cell Homeostasis in Mice
RESEARCH ARTICLE The H3K4 methyltransferase Setd1b is essential for hematopoietic stem and progenitor cell homeostasis in mice Kerstin Schmidt1, Qinyu Zhang2, Alpaslan Tasdogan3,4, Andreas Petzold5, Andreas Dahl5, Borros M Arneth6, Robert Slany7, Hans Jo¨ rg Fehling3, Andrea Kranz2*, Adrian Francis Stewart2*, Konstantinos Anastassiadis1* 1Stem Cell Engineering, Biotechnology Center, Technische Universita¨ t Dresden, Dresden, Germany; 2Genomics, Biotechnology Center, Technische Universita¨ t Dresden, Dresden, Germany; 3Institute of Immunology, University Hospital Ulm, Ulm, Germany; 4Department of Dermatology, University Hospital Ulm, Ulm, Germany; 5Deep Sequencing Group, DFG - Center for Regenerative Therapies Dresden, Dresden, Germany; 6Institute of Laboratory Medicine and Pathobiochemistry, Molecular Diagnostics, Hospital of the Universities Giessen and Marburg, Giessen, Germany; 7Department of Genetics, Friedrich Alexander Universita¨ t Erlangen, Erlangen, Germany Abstract Hematopoietic stem cells require MLL1, which is one of six Set1/Trithorax-type histone 3 lysine 4 (H3K4) methyltransferases in mammals and clinically the most important leukemia gene. Here, we add to emerging evidence that all six H3K4 methyltransferases play essential roles in the hematopoietic system by showing that conditional mutagenesis of Setd1b in adult mice provoked *For correspondence: aberrant homeostasis of hematopoietic stem and progenitor cells (HSPCs). Using both ubiquitous [email protected] (AK); and hematopoietic-specific deletion strategies, the loss of Setd1b resulted in peripheral thrombo- [email protected] and lymphocytopenia, multilineage dysplasia, myeloid-biased extramedullary hematopoiesis in the (AFS); spleen, and lethality. By transplantation experiments and expression profiling, we determined that konstantinos.anastassiadis@tu- Setd1b is autonomously required in the hematopoietic lineages where it regulates key lineage dresden.de (KA) specification components, including Cebpa, Gata1, and Klf1.