09-17-12 Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Legislative Locator Legislative Locator
Legislative Locator Legislative Locator A Monthly Publication of The Pennsylvania Municipal League May 2019 TAKE ACTION! Attention Local Officials: Please reach out to your Senators and members of the Senate Transportation Committee where Senate Bill 607 awaits a vote - and express your support! Senate Bill 607 (PN 675) authorizes the use of radar and LIDAR for all municipal police. This proposal is supported by the Radar Coalition, which includes The League and PSATC. Please consider adopting a resolution supporting local use of radar in your municipality. We are providing a sample resolution on our website. If you have adopted a resolution in past sessions, it should be updated. In addition, we are providing a sample press release to use after adopting a resolution to let your residents know that municipal radar is a priority in your community and to encourage them to advocate for the passage of Senate Bill 607, too. Three other proposals have been introduced this session, which include provisions that authorize the restricted use of radar, they are: House Bill 74 (PN 78), introduced by Representative Greg Rothman; House Bill 352 (PN 328), introduced by Representative Bill Kortz; and House Bill 1275 (PN 1483), introduced by Representative Kurt Masser. The League and PSATC currently do not support these proposals as drafted due to their restrictive nature. All three of these bills are currently before the House Transportation Committee. (See SB 607 summary on next page) 1 Leisatie Locato Leisatie Locato Local Use of Radar and LIDAR Senate Bill 607 (PN 675), introduced by Senator Mario Scavello, amends Title 75 (Vehicles) authorizing the local use of both radar and LIDAR by any police officer. -

Representative Districts for the Susquehanna River Basin
April 30, 2021 Representative Districts for the Susquehanna River Basin Rom e !( 118 !( Utica Roche ste r HERKIMER !( !( !( One ida ONEIDA !( S yra cuse He rkim e r Aub urn ONONDAGA 127 Ca na joha rie Ca na nda ig ua !( !( !( !( Ge ne se o Ge ne va !( ONTARIO MADIS ON Coope rstown S CHOHARIE 131 121 !( !( 133 YATES CORTLAND !( 126 101 Cob le skill LIVINGS TON Pe nn Ya n OTS EGO !( Cortla nd !( 102 TOMPKINS Norwich One onta !( S CHUYLER !( 125 CHENANGO !( Itha ca Ba th !( Wa tkins Gle n 122 ALLEGANY S TEUBEN TIOGA Wa lton Corning !( We llsville 132 !( Bing ha m ton Ole a n !( CHEMUNG Owe g o 148 !( !( !( !( 124 123 DELAWARE Elm ira BROOME !( S a yre S US QUEHANNA Port Alle g a ny !( Ma nsfie ld !( Coude rsport !( Towa nda Montrose !( Ga le ton !( 111 McKEAN !( WAYNE 68 BRADFORD Montice llo TIOGA !( POTTER 110 114 Hone sda le Tunkha nnock LACKA- !( Em porium 67 !( !( !( WANNA Dushore WYOMING 112 S t. Ma rys !( CAMERON S cra nton S ULLIVAN 117 !( 139 84 LYCOMING ELK Re novo 113 !( 75 120 Willia m sport Wilke s-Ba rre !( JEFFERS ON CLINTON 83 !( 121 109 LUZERNE 118 DuBois !( 76 CLEARFIELD COLUMBIA 119 66 116 Ea st S troudsb urg !( MON- Bloom sb urg !( Punxsuta wne y Cle a rfie ld CENTRE Le wisb urg TOUR !( Ha zle ton 122 !( !( !( !( UNION CARBON Da nville 77 Le hig hton 73 85 !( S unb ury 107 S ta te Colle g e 171 !( S e linsg rove INDIANA !( !( NORTH- S NYDER 108 UMBERLAND 123 MIFFLIN !( Northe rn !( !( Ca m b ria S CHUYLKILL Pottsville Alle ntown Le wistown JUNIATA !( India na 72 !( 124 Altoona Port Roya l 125 !( Hunting don !( !( DAUPHIN -

House of Representatives
COMMONWEALTH OF PENNSYLVANIA HOUSE OF REPRESENTATIVES APPROPRIATIONS COMMITTEE HEARING STATE CAPITOL MAIN BUILDING ROOM 140 HARRISBURG, PENNSYLVANIA WEDNESDAY , MARCH 11, 2015 PRESENTATION FROM DEPARTMENT OF COMMUNITY AND ECONOMIC DEVELOPMENT BEFORE: HONORABLE WILLIAM F. ADOLPH , JR., MAJORITY CHAIRMAN HONORABLE JOSEPH MARKOSEK , MINORITY CHAIRMAN HONORABLE KAREN BOBACK HONORABLE JIM CHRISTIANA HONORABLE GARY DAY HONORABLE GEORGE DUNBAR HONORABLE GARTH EVERETT HONORABLE KEITH GREINER HONORABLE GLEN GRELL HONORABLE SETH GROVE HONORABLE WARREN KAMPF HONORABLE FRED KELLER HONORABLE TOM KILLION HONORABLE JIM MARSHALL HONORABLE KURT MASSER HONORABLE DAVID R. MILLARD HONORABLE MARK T. MUSTIO HONORABLE MICHAEL PEIFER HONORABLE JEFFREY P. PYLE HONORABLE MARGUERITE QUINN HONORABLE CURTIS G. SONNEY HONORABLE MIKE VEREB ————————— JEAN DAVIS REPORTING 285 EAST MANSION ROAD • HERSHEY, PA 17033 Phone (717)503-6568 1 BEFORE (cont.'d): 2 HONORABLE MATTHEW D. BRADFORD HONORABLE TIM BRIGGS 3 HONORABLE MICHELLE F. BROWNLEE HONORABLE MIKE CARROLL 4 HONORABLE H. SCOTT CONKLIN HONORABLE MARY JO DALEY 5 HONORABLE MADELEINE DEAN HONORABLE MARIA DONATUCCI 6 HONORABLE EDWARD GAINEY HONORABLE JOHN GALLOWAY 7 HONORABLE STEPHEN KINSEY HONORABLE MICHAEL H. O'BRIEN 8 HONORABLE CHERELLE L. PARKER HONORABLE KEVIN SCHREIBER 9 10 ALSO IN ATTENDANCE : 11 DAVID DONLEY, REPUBLICAN EXECUTIVE DIRECTOR RITCHIE LaFAVER, REPUBLICAN EXECUTIVE DIRECTOR 12 CURT SCHRODER, REPUBLICAN CHIEF COUNSEL MIRIAM FOX, DEMOCRATIC EXECUTIVE DIRECTOR 13 ANNE BALOGA, DEMOCRATIC CHIEF COUNSEL HONORABLE VANESSA LOWERY BROWN 14 HONORABLE ELI EVANKOVICH HONORABLE ROBERT GODSHALL 15 HONORABLE BARRY JOZWIAK HONORABLE WILLIAM KORTZ 16 HONORABLE JOHN MAHER HONORABLE DAVID PARKER 17 HONORABLE THOMAS QUIGLEY HONORABLE MICHAEL SCHLOSSBERG 18 HONORABLE CRAIG STAATS HONORABLE GREG VITALI 19 HONORABLE JAKE WHEATLEY 20 21 JEAN M. -

LRI's Rev Up! Philadelphia 2018 Booklet
Register, Educate, Vote, Use Your Power Full political participation for Americans with disabilities is a right. AAPD works with state and national coalitions on effective, non- partisan campaigns to eliminate barriers to voting, promoting accessible voting technology and polling places; educate voters about issues and candidates; promote turnout of voters with disabilities across the country; protect eligible voters’ right to participate in elections; and engage candidates and elected officials to recognize the disability community. 1 Pennsylvania 2018 Midterm Election Dates 2018 Pennsylvania Midterm Election Registrations Date: Tuesday, October 9, 2018 – DEADLINE!! 2018 Pennsylvania Midterm Elections Date: Tuesday, November 6, 2018, 7 am – 8 pm Pennsylvania Voter Services https://www.pavoterservices.pa.gov • Register to Vote • Apply for An Absentee Ballot • Check Voter Registration Status • Check Voter Application Status • Find Your Polling Place 2 Table of Contents Pennsylvania 2018 Midterm Election Dates ............................ 2 2018 Pennsylvania Midterm Election Registrations ................. 2 2018 Pennsylvania Midterm Elections .................................. 2 Table of Contents ................................................................ 3 Voting Accommodations ....................................................... 7 Voter Registration ............................................................ 7 Language Access ................................................................ 8 Issues that Affect People with Disabilities -

November 7, 2018 Pennsylvania Was One of the Most Closely Watched
Keep up to date with our blog: Follow us on Twitter @BuchananGov knowingGovernmentRelations.com November 7, 2018 Pennsylvania was one of the most closely watched states in the country on Election Day. Redistricting of Congressional seats meant a shakeup was coming for the Commonwealth’s 18-member delegation. At the statewide level, the Governor and one of two U.S. Senators were on the ballot. In the state legislature, half of the 50 Senate seats (even- numbered districts) and the entire 203-seat House of Representatives were up for grabs. During the 2017-18 legislative session the Pennsylvania House of Representatives was comprised of 121 Republicans and 82 Democrats. After last night’s election, the 2018-19 legislative session will have 109 Republicans and 94 Democrats, after the Democrats picked up 11 seats. In the Pennsylvania Senate, Republicans had a majority during the 2017-18 by a margin of 34-16. Yesterday, Senate Democrats picked up 5 seats, narrowing the Republican’s majority. Next session will have 29 Republican members and 21 Democratic members. The 18-member Pennsylvania delegation had only 6 Democrats during the 115th Congress (2017-19). When new members are sworn into the 116th Congress next year, Pennsylvania’s delegation will be split, with 9 Republicans and 9 Democrats. Governor Governor Tom Wolf (D) and his running mate for Lieutenant Governor John Fetterman (D) defeated the ticket of Scott Wagner (R) and Jeff Bartos (R). Wolf received 2,799,1559 votes (57.66%), while Wagner got 1,981,027 votes (40.81%). U.S. Senate Senator Bob Casey (D) defeated Lou Barletta (R) by a margin of over half a million votes. -

Pennsylvania Issues Miscellaneous • Election Update: on November 8
November 22, 2016 Pennsylvania Issues Miscellaneous • Election Update: On November 8, 2016, Pennsylvania residents elected candidates for all 203 seats in the Pennsylvania House of Representatives and 25 seats in the Pennsylvania Senate. Senator David Argall (R-Berks, Schuylkill) and Representatives Gary Day (R-Lehigh, Berks), Robert Freeman (D- Northampton), Jerry Knowles (R-Schuylkill, Berks, Carbon), Ryan MacKenzie (R-Berks, Lehigh), Jack Rader (R-Monroe), Steve Samuelson (D-Northampton) and Peter Schweyer (D-Lehigh) were reelected without opposition. Representatives Rosemary Brown (R-Monroe, Pike), Joe Emrick (R-Northampton), Marcia Hahn (R-Northampton), Doyle Heffley (R-Carbon), Dan McNeill (D-Lehigh, Northampton), Michael Schlossberg (D-Lehigh), Justin Simmons (R-Lehigh, Montgomery, Northampton) and Craig Staats (R-Bucks) were reelected despite opposition. Representative David Parker (R-Monroe) was defeated by Democratic challenger Maureen Madden. After 11 terms in office, Representative Julie Harhart (R-Lehigh, Northampton) did not seek reelection and will be succeeded by Republican Zachary Mako, a helicopter pilot in the Pennsylvania Army National Guard. • Pennsylvania House and Senate Reorganization: House Republicans gained three seats and will maintain their majority for the fourth consecutive session with 122 Republicans and 81 Democrats. House Republicans renewed their leadership positions, except that Representative Stan Saylor (R-York) will serve as the Appropriations Chairman, Representative Marcy Toepel (R-Montgomery) will serve as Caucus Chairman and Representative Kurt Masser (R-Columbia, Montour, Northumberland) will serve as Caucus Administrator. House Democrats renewed all of their leadership positions. Senate Republicans gained four seats and now hold a 34 to 16 majority. Senate Republicans and Democrats renewed all of their leadership positions. -

Legislative Achievements
LEGISLATIVE ACHIEVEMENTS P E N N S Y L V A N I A HOUSE REPUBLICAN CAUCUS 2019-2020 Legislative Session September 2020 1 | 2019/20 Legislative Accomplishments Pennsylvania’s House Republican Caucus is committed to our state’s residents and taxpayers. Constantly striving to strengthen economic opportunities for all, enact commonsense public policy, and provide a government that is both efficient and effective, the Pennsylvania House Republican Caucus is out front, fighting to make Pennsylvania the best place to live, work and raise a family – equally, for every Pennsylvanian. By working together, we have accomplished much and have shown we stand by our commitments to our constituents. 2 | 2019/20 Legislative Accomplishments ACHIEVEMENTS Pennsylvania House of Representatives 2019-2020 Legislative Session Budget Highlights 2020-2021 Budget 7 2019-2020 Budget 9 COVID-19 Pandemic COVID Response 12 Economic Enhancers #GOODJOBS4PA 21 Promoting Confidence Among Consumers and Businesses 24 Preserving PA’s Agricultural Heritage 26 Protecting Pennsylvanians Protecting Victims 30 Addiction and Substance Use Disorder 34 Emergency Responders 35 Justice Reform 37 Strengthening Communities & Supporting Families 40 Senior Citizens 42 Health Care that Makes Sense 43 Conservation Efforts to Achieve Results 47 Standing up for Taxpayer Government Done Right 49 Fiscal Responsibility 58 Relaxing the State’s Hold on Alcohol 60 Advancing Local Government 62 Insurance Related Concerns 66 Education Accomplishments 3 | 2019/20 Legislative Accomplishments Education: Equipping Students for Success 68 Safeguarding Citizens’ Rights to Safely Hunt and Fish 71 Supporting and Honoring Our Veterans 73 Transportation 75 Miscellaneous 77 4 | 2019/20 Legislative Accomplishments 5 | 2019/20 Legislative Accomplishments Budget Highlights 6 | 2019/20 Legislative Accomplishments 2020-2021 Budget Faced with the economic uncertainty created Signed in Law: by the COVID-19 epidemic, the delaying of • Act 1A of 2020 (formerly HB 2387, filing taxes and a potential $5 billion Rep. -
FOAC Voters Guides
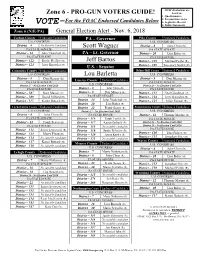
FOAC Evaluations are Zone 6 - PRO-GUN VOTERS GUIDE! based on: 1. Questionnaires For the FOAC Endorsed Candidates Below 2. Personal Interviews VOTE- 3. Legislative Record 4. Public Statements Zone 6 (N/E-PA) General Election Alert - Nov. 6, 2018 Carbon County Endorsed Candidates PA – Governor Pike County Endorsed Candidates U.S. CONGRESS U.S. CONGRESS District – 6 No Suitable Candidate Scott Wagner District – 8 John Chrin (R) PA STATE SENATE PA STATE SENATE District – 14 John Yudichak (D) PA – Lt. Governor District – 20 Lisa Baker (R) PA STATE HOUSE PA STATE HOUSE District – 122 Doyle Heffley (R) Jeff Bartos District – 139 Michael Peifer (R) District – 124 Jerry Knowles (R) District – 189 Rosemary Brown (R) U.S. - Senator Columbia County Endorsed Candidates Schuylkill County Endorsed Candidates U.S. CONGRESS Lou Barletta U.S. CONGRESS District – 9 Dan Meuser (R) District – 9 Dan Meuser (R) Luzerne County Endorsed Candidates PA STATE SENATE PA STATE SENATE District 27 - No Election Until 2020 U.S. CONGRESS District 29 - No Election Until 2016 PA STATE HOUSE District – 8 John Chrin (R) PA STATE HOUSE District – 107 Kurt Masser (R) District – 9 Dan Meuser (R) District – 123 Neal Goodman (D) District – 109 David Millard (R) PA STATE SENATE District – 124 Jerry Knowles (R) District - 117 Karen Boback (R) District – 14 John Yudichak (D) District – 125 Mike Tobash (R) District – 20 Lisa Baker (R) Lackawanna County Endorsed Candidates District – 22 Frank Scavo (R) Susquehanna County Endorsed Candidates U.S. CONGRESS District 27 - No Election Until -

House Republican Caucus Elects Leadership For
November 16, 2020 – Issue 134 our nation forward by always answering the call of House Republican Caucus our constituents to face ever-evolving challenges. I Elects Leadership for 2021- am honored and inspired to join with these proven, principled and selfless public servants to continue to 22 Session answer the call to improve the lives of Pennsylvanians and stand humbled and ready to he Pennsylvania House Republican Caucus oversee another successful session." Tuesday elected its legislative leaders for the T 2021-22 Legislative Session. House Majority Leader Kerry Benninghoff (R-Centre/Mifflin): "Led by our message of fiscal The leadership team consists of: responsibility, adding common sense to our COVID-19 response, and ensuring government is Speaker-designee Bryan Cutler (R-Lancaster). responsible to the people, the voters of Majority Leader Kerry Benninghoff (R- Pennsylvania have returned a significant Centre/Mifflin). Republican majority back to the Pennsylvania Majority Whip Donna Oberlander (R- General Assembly. I am proud to lead our caucus in Clarion/Armstrong/Forest). our ongoing mission to be the true voice of the Majority Appropriations Committee people and work to improve the lives of Chairman Stan Saylor (R-York). Pennsylvanians everywhere." Majority Policy Committee Chairman Marty Causer (R-Cameron/McKean/Potter). Majority Whip Donna Oberlander (R- Majority Caucus Chairman Mike Reese (R- Clarion/Armstrong/Forest): "Today's leadership Westmoreland/Somerset). election sends a strong message that we, as a caucus, are poised to use our growing strength in Majority Caucus Secretary Martina White (R- order to confront the challenges facing our Philadelphia). Commonwealth in the next two years," said Majority Caucus Administrator Kurt Masser Oberlander. -

Commonwealth of Pennsylvania Legislative
COMMONWEALTH OF PENNSYLVANIA LEGISLATIVE JOURNAL TUESDAY, JUNE 6, 2017 SESSION OF 2017 201ST OF THE GENERAL ASSEMBLY No. 28 HOUSE OF REPRESENTATIVES COMMUNICATION FROM The House convened at 11 a.m., e.d.t. INDEPENDENT FISCAL OFFICE The SPEAKER. The Speaker acknowledges receipt of a THE SPEAKER (MIKE TURZAI) letter from the Independent Fiscal Office regarding an actuarial PRESIDING note for HB 922, PN 1910. PRAYER (Copy of communication is on file with the Journal clerk.) HON. HAROLD A. ENGLISH, member of the House of BILLS REPORTED FROM COMMITTEES, Representatives, offered the following prayer: CONSIDERED FIRST TIME, AND Heavenly Father, thank You for this beautiful day and RECOMMITTED TO COMMITTEE ON RULES bringing us here safely to work in this House with so many HB 302, PN 302 By Rep. BARRAR wonderful people with different backgrounds, thoughts, and beliefs. We ask for Your help and guidance so that we may hear An Act amending Title 51 (Military Affairs) of the Pennsylvania all voices, ideas, and opinions. Consolidated Statutes, in professional and occupational licenses, God, Your story is so beautiful. Allow us to hear the further providing for retention of licenses and certifications of persons symmetry of that first Passover that launched the Jewish people entering military service. into freedom from Egyptian slavery, but also into a wilderness VETERANS AFFAIRS AND EMERGENCY identity crisis that was resolved with the giving of the Ten PREPAREDNESS. Commandments and the last Passover with Christ's death and resurrection that launched Christian disciples and believers into HB 353, PN 1911 (Amended) By Rep. BAKER freedom from fear of death and also into a wilderness identity crisis that was resolved with the giving of the Holy Spirit on An Act amending the act of April 14, 1972 (P.L.233, No.64), Pentecost. -

1 Commonwealth of Pennsylvania House of Representatives
1 COMMONWEALTH OF PENNSYLVANIA HOUSE OF REPRESENTATIVES APPROPRIATIONS COMMITTEE BUDGET HEARING GAMING CONTROL BOARD STATE CAPITOL HARRISBURG, PENNSYLVANIA ROOM 140, MAJORITY CAUCUS ROOM THURSDAY, MARCH 12, 2015 9:30 A.M. BEFORE: HONORABLE WILLIAM ADOLPH, MAJORITY CHAIRMAN HONORABLE JOSEPH MARKOSEK, MINORITY CHAIRMAN HONORABLE KAREN BOBACK HONORABLE GARY DAY HONORABLE GEORGE DUNBAR HONORABLE KEITH GREINER HONORABLE GLEN GRELL HONORABLE SETH GROVE HONORABLE WARREN KAMPF HONORABLE FRED KELLER HONORABLE TOM KILLION HONORABLE JIM MARSHALL HONORABLE KURT MASSER HONORABLE DAVID MILLARD HONORABLE DUANE MILNE HONORABLE MIKE PEIFER HONORABLE JEFFREY PYLE HONORABLE MARGUERITE QUINN HONORABLE CURT SONNEY HONORABLE MIKE VEREB HONORABLE MATTHEW BRADFORD HONORABLE TIM BRIGGS HONORABLE MICHELLE BROWNLEE HONORABLE MIKE CARROLL HONORABLE SCOTT CONKLIN 2 1 HONORABLE MARY JO DALEY HONORABLE MADELEINE DEAN 2 HONORABLE MARIA DONATUCCI HONORABLE EDWARD GAINEY 3 HONORABLE JOHN GALLOWAY HONORABLE STEPHEN KINSEY 4 HONORABLE MICHAEL O'BRIEN 5 NON-COMMITTEE MEMBERS: 6 REPRESENTATIVE DARYL METCALFE REPRESENTATIVE MARK COHEN 7 REPRESENTATIVE PAM DELISSIO REPRESENTATIVE VANESSA LOWERY BROWN 8 9 COMMITTEE STAFF: 10 DAVID DONLEY, EXECUTIVE DIRECTOR (R) RITCHIE LAFAVER, DEPUTY EXECUTIVE DIRECTOR (R) 11 CURT SCHRODER, CHIEF COUNSEL MIRIAM FOX, EXECUTIVE DIRECTOR (D) 12 ANNE BALOGA, CHIEF COUNSEL (D) 13 14 TRACY L. MARKLE, COURT REPORTER/NOTARY PUBLIC 15 16 17 18 19 20 21 22 23 24 25 3 1 INDEX TO TESTIFIERS NAME PAGE 2 WILLIAM H. RYAN, JR, CHAIRMAN 5 3 GAMING CONTROL BOARD 4 KEVIN O'TOOLE, EXECUTIVE DIRECTOR 22 GAMING CONTROL BOARD 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 4 1 ---oOo--- 2 MAJORITY CHAIRMAN ADOLPH: Thank you, and 3 good morning. -

Legislative Accomplishments
LEGISLATIVE ACHIEVEMENTS P E N N S Y L V A N I A HOUSE REPUBLICAN CAUCUS 2019-2020 Legislative Session Fall 2019 Pennsylvania’s House Republican Caucus is committed to our state’s residents and taxpayers. Constantly striving to strengthen the economy, enact commonsense public policy, and provide a government that is both efficient and effective, the Pennsylvania House Republican Caucus is out front, fighting to make Pennsylvania the best place to live, work and raise a family. By working together, we have accomplished much and have shown we stand by our commitments. 2 | Page ACHIEVEMENTS Pennsylvania House of Representatives 2019-2020 Legislative Session Budget 5 Economic Enhancers #GOODJOBS4PA 8 Promoting Confidence Among Consumers and Businesses 11 Preserving PA’s Agricultural Heritage 12 Protecting Pennsylvanians Protecting Victims 16 Addiction and Substance Use Disorder 19 Emergency Responders 20 Justice Reform 22 Strengthening Communities & Supporting Families 23 Senior Citizens 25 Health Care that Makes Sense 26 Conservation Efforts to Achieve Results 28 Standing up for Taxpayers Government Done Right 30 Fiscal Responsibility 37 Relaxing the State’s Hold on Alcohol 38 Advancing Local Government 39 Insurance Related Concerns 41 Education Accomplishments Education: Equipping Students for Success 43 Safeguarding Citizens’ Rights to Safely Hunt and Fish 45 Supporting and Honoring Our Veterans 46 Transportation 48 Miscellaneous 49 3 | Page 4 | Page Budget Thanks to Republican-led budgets, our ways. School funding is revenues are up, and we are on a path to increased, but so is better protect taxpayers now and in the funding to support future. opportunities for students to thrive in private, • This budget puts $317 million charter and online into the Rainy Day Fund.