Lecture 6: Medical Imaging and Image-Guided Interventions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bio 219 Biomedical Imaging and Scientific Visualization
Bio 219 Biomedical Imaging and Scientific Visualization Ch. Zollikofer M. Ponce de León Organization • OLAT: – course scripts (pdf) • website: www.aim.uzh.ch/morpho/wiki/Teaching/SciVis – course scripts (pdf); passwd: scivisdocs – link collection (tutorials, applets, software/data downloads, ...) • book (background information): Zollikofer & Ponce de León, Virtual Reconstruction. A Primer in Computer-assisted Paleontology and Biomedicine (NY: Wiley, 2005) CHF 55 • final exam – Monday, 26. May 2014, 1015-1100 BioMedImg & SciVis • at the intersection between – theory/practice of image data acquisition – computer graphics – medical diagnostics – computer-assisted paleoanthropology Grotte Chauvet, France Biomedical Imaging • acquisition • processing • analysis • visualization ... of biomedical data Scientific Visualization visual... • representation (cf. data presentation) • exploration • analysis ...of scientific data aims of this course • provide theoretical (and practical) foundations of – image data acquisition, storage, retrieval – image data processing and analysis – image data visualization/rendering • establish links between – real-life vision and computer vision – computer science and biomedical sciences – theory and practice of handling biomedical data contents • real-life vision • computers and data representation • 2D image data acquisition • 3D image data acquisition • biomedical image processing in 2D and 3D • biomedical image data visualization and interaction biomedical data types of data data flow humans and computers facts and data • facts exist by definition (±independent of the observer): – females and males – humans and Neanderthals – dogs and wolves • data are generated through observation: – number of living human species: 1 – proportion of females to males at birth: 49/51 – nr. of wolves per square km biomedical data: general • physical/physiological data about the human body: – density – temperature – pressure – mass – chemical composition biomedical data: space and time • spatial – 1D – 2D – 3D • temporal • spatiotemporal (4D) .. -
Statement by the Association of Hoving Image Archivists (AXIA) To
Statement by the Association of Hoving Image Archivists (AXIA) to the National FTeservation Board, in reference to the Uational Pilm Preservation Act of 1992, submitted by Dr. Jan-Christopher Eorak , h-esident The Association of Moving Image Archivists was founded in November 1991 in New York by representatives of over eighty American and Canadian film and television archives. Previously grouped loosely together in an ad hoc organization, Pilm Archives Advisory Committee/Television Archives Advisory Committee (FAAC/TAAC), it was felt that the field had matured sufficiently to create a national organization to pursue the interests of its constituents. According to the recently drafted by-laws of the Association, AHIA is a non-profit corporation, chartered under the laws of California, to provide a means for cooperation among individuals concerned with the collection, preservation, exhibition and use of moving image materials, whether chemical or electronic. The objectives of the Association are: a.) To provide a regular means of exchanging information, ideas, and assistance in moving image preservation. b.) To take responsible positions on archival matters affecting moving images. c.) To encourage public awareness of and interest in the preservation, and use of film and video as an important educational, historical, and cultural resource. d.) To promote moving image archival activities, especially preservation, through such means as meetings, workshops, publications, and direct assistance. e. To promote professional standards and practices for moving image archival materials. f. To stimulate and facilitate research on archival matters affecting moving images. Given these objectives, the Association applauds the efforts of the National Film Preservation Board, Library of Congress, to hold public hearings on the current state of film prese~ationin 2 the United States, as a necessary step in implementing the National Film Preservation Act of 1992. -

Three-Dimensional Thematic Map Imaging of the Yacht Port on the Example of the Polish National Sailing Centre Marina in Gda ´Nsk
applied sciences Article Three-Dimensional Thematic Map Imaging of the Yacht Port on the Example of the Polish National Sailing Centre Marina in Gda ´nsk Pawel S. Dabrowski 1 , Cezary Specht 1,* , Mariusz Specht 2 and Artur Makar 3 1 Department of Geodesy and Oceanography, Gdynia Maritime University, 81-347 Gdynia, Poland; [email protected] 2 Department of Transport and Logistics, Gdynia Maritime University, 81-225 Gdynia, Poland; [email protected] 3 Department of Navigation and Hydrography, Polish Naval Academy, 81-127 Gdynia, Poland; [email protected] * Correspondence: [email protected] Abstract: The theory of cartographic projections is a tool which can present the convex surface of the Earth on the plane. Of the many types of maps, thematic maps perform an important function due to the wide possibilities of adapting their content to current needs. The limitation of classic maps is their two-dimensional nature. In the era of rapidly growing methods of mass acquisition of spatial data, the use of flat images is often not enough to reveal the level of complexity of certain objects. In this case, it is necessary to use visualization in three-dimensional space. The motivation to conduct the study was the use of cartographic projections methods, spatial transformations, and the possibilities offered by thematic maps to create thematic three-dimensional map imaging (T3DMI). The authors presented a practical verification of the adopted methodology to create a T3DMI visualization of Citation: Dabrowski, P.S.; Specht, C.; Specht, M.; Makar, A. the marina of the National Sailing Centre of the Gda´nskUniversity of Physical Education and Sport Three-Dimensional Thematic Map (Poland). -

MRC Review of Positron Emission Tomography (PET) Within the Medical Imaging Research Landscape
MRC Review of Positron Emission Tomography (PET) within The Medical Imaging Research Landscape August 2017 Content 1 Introduction 3 2 The medical imaging research landscape in the UK 4 2.1 Magnetic resonance imaging (MRI) 4 2.2 PET, including PET-MRI 6 2.3 Magnetoencephalography 7 3 Scientific uses and demand for PET imaging 8 3.1 Clinical practice 8 3.2 Research use of PET 8 3.3 Demand for PET 10 4 Bottlenecks 11 4.1 Cost 11 4.2 Radiochemistry requirements 12 4.3 Capacity 13 4.4 Analysis and modelling 13 5 Future Opportunities 14 5.1 Mitigating the high costs 14 5.2 Capacity building 14 5.3 Better Networking 15 6 Discussion and conclusions 16 Appendix 1 Experts consulted in the review 17 Appendix 2 Interests of other funders 18 Appendix 3 Usage and cost of PET in research 21 Appendix 4 Summary of facilities and capabilities across UK PET centres of excellence 23 2 1. Introduction This report aims to provide a review of Positron Emission Tomography (PET) within the medical imaging research landscape and a high level strategic review of the UK’s capabilities and needs in this area. The review was conducted by face-to-face and telephone interviews with 35 stakeholders from UK centres of excellence, international experts, industry and other funders (list at appendix 1). Data were also collected on facilities, resources and numbers of scans conducted across the centres of excellence using a questionnaire. The review has focused predominantly on PET imaging, but given MRC’s significant recent investment in other imaging modalities (7T Magnetic Resonance Imaging (MRI), hyperpolarised MRI) through the Clinical Research Infrastructure (CRI) Initiative, these are also considered more briefly. -

Members | Diagnostic Imaging Tests
Types of Diagnostic Imaging Tests There are several types of diagnostic imaging tests. Each type is used based on what the provider is looking for. Radiography: A quick, painless test that takes a picture of the inside of your body. These tests are also known as X-rays and mammograms. This test uses low doses of radiation. Fluoroscopy: Uses many X-ray images that are shown on a screen. It is like an X-ray “movie.” To make images clear, providers use a contrast agent (dye) that is put into your body. These tests can result in high doses of radiation. This often happens during procedures that take a long time (such as placing stents or other devices inside your body). Tests include: Barium X-rays and enemas Cardiac catheterization Upper GI endoscopy Angiogram Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA): Use magnets and radio waves to create pictures of your body. An MRA is a type of MRI that looks at blood vessels. Neither an MRI nor an MRA uses radiation, so there is no exposure. Ultrasound: Uses sound waves to make pictures of the inside of your body. This test does not use radiation, so there is no exposure. Computed Tomography (CT) Scan: Uses a detector that moves around your body and records many X- ray images. A computer then builds pictures or “slices” of organs and tissues. A CT scan uses more radiation than other imaging tests. A CT scan is often used to answer, “What does it look like?” Nuclear Medicine Imaging: Uses a radioactive tracer to produce pictures of your body. -

Lab 11: the Compound Microscope
OPTI 202L - Geometrical and Instrumental Optics Lab 9-1 LAB 9: THE COMPOUND MICROSCOPE The microscope is a widely used optical instrument. In its simplest form, it consists of two lenses Fig. 9.1. An objective forms a real inverted image of an object, which is a finite distance in front of the lens. This image in turn becomes the object for the ocular, or eyepiece. The eyepiece forms the final image which is virtual, and magnified. The overall magnification is the product of the individual magnifications of the objective and the eyepiece. Figure 9.1. Images in a compound microscope. To illustrate the concept, use a 38 mm focal length lens (KPX079) as the objective, and a 50 mm focal length lens (KBX052) as the eyepiece. Set them up on the optical rail and adjust them until you see an inverted and magnified image of an illuminated object. Note the intermediate real image by inserting a piece of paper between the lenses. Q1 ● Can you demonstrate the final image by holding a piece of paper behind the eyepiece? Why or why not? The eyepiece functions as a magnifying glass, or simple magnifier. In effect, your eye looks into the eyepiece, and in turn the eyepiece looks into the optical system--be it a compound microscope, a spotting scope, telescope, or binocular. In all cases, the eyepiece doesn't view an actual object, but rather some intermediate image formed by the "front" part of the optical system. With telescopes, this intermediate image may be real or virtual. With the compound microscope, this intermediate image is real, formed by the objective lens. -
Image Compression Using Discrete Cosine Transform Method
Qusay Kanaan Kadhim, International Journal of Computer Science and Mobile Computing, Vol.5 Issue.9, September- 2016, pg. 186-192 Available Online at www.ijcsmc.com International Journal of Computer Science and Mobile Computing A Monthly Journal of Computer Science and Information Technology ISSN 2320–088X IMPACT FACTOR: 5.258 IJCSMC, Vol. 5, Issue. 9, September 2016, pg.186 – 192 Image Compression Using Discrete Cosine Transform Method Qusay Kanaan Kadhim Al-Yarmook University College / Computer Science Department, Iraq [email protected] ABSTRACT: The processing of digital images took a wide importance in the knowledge field in the last decades ago due to the rapid development in the communication techniques and the need to find and develop methods assist in enhancing and exploiting the image information. The field of digital images compression becomes an important field of digital images processing fields due to the need to exploit the available storage space as much as possible and reduce the time required to transmit the image. Baseline JPEG Standard technique is used in compression of images with 8-bit color depth. Basically, this scheme consists of seven operations which are the sampling, the partitioning, the transform, the quantization, the entropy coding and Huffman coding. First, the sampling process is used to reduce the size of the image and the number bits required to represent it. Next, the partitioning process is applied to the image to get (8×8) image block. Then, the discrete cosine transform is used to transform the image block data from spatial domain to frequency domain to make the data easy to process. -

Ground-Based Photographic Monitoring
United States Department of Agriculture Ground-Based Forest Service Pacific Northwest Research Station Photographic General Technical Report PNW-GTR-503 Monitoring May 2001 Frederick C. Hall Author Frederick C. Hall is senior plant ecologist, U.S. Department of Agriculture, Forest Service, Pacific Northwest Region, Natural Resources, P.O. Box 3623, Portland, Oregon 97208-3623. Paper prepared in cooperation with the Pacific Northwest Region. Abstract Hall, Frederick C. 2001 Ground-based photographic monitoring. Gen. Tech. Rep. PNW-GTR-503. Portland, OR: U.S. Department of Agriculture, Forest Service, Pacific Northwest Research Station. 340 p. Land management professionals (foresters, wildlife biologists, range managers, and land managers such as ranchers and forest land owners) often have need to evaluate their management activities. Photographic monitoring is a fast, simple, and effective way to determine if changes made to an area have been successful. Ground-based photo monitoring means using photographs taken at a specific site to monitor conditions or change. It may be divided into two systems: (1) comparison photos, whereby a photograph is used to compare a known condition with field conditions to estimate some parameter of the field condition; and (2) repeat photo- graphs, whereby several pictures are taken of the same tract of ground over time to detect change. Comparison systems deal with fuel loading, herbage utilization, and public reaction to scenery. Repeat photography is discussed in relation to land- scape, remote, and site-specific systems. Critical attributes of repeat photography are (1) maps to find the sampling location and of the photo monitoring layout; (2) documentation of the monitoring system to include purpose, camera and film, w e a t h e r, season, sampling technique, and equipment; and (3) precise replication of photographs. -

(NSPM) Content Outline and Exam Blueprint Effective Through 2020
Nonsurgical Pain Management (NSPM) Content Outline and Exam Blueprint Effective through 2020 The NSPM subspecialty examination will assess a nurse anesthetist’s competence of needle placement in three anatomical approaches (i.e., midline, lateral, peripheral) and four anatomical regions (i.e., cervical, thoracic, lumbar, and sacral), as well as assess knowledge related to the NSPM certification examination content outline as listed below: Domain I. Physiology and Pathophysiology of Pain (13%) I.A. Applicable anatomy and physiology of pain I.B. Nociception: transduction, transmission, perception and modulation of pain I.C. Factors influencing pain I.D. Cellular response to pain and treatment I.E. Pain classifications I.F. Evidence based principles I.G. Pathophysiology I.G.1. Neurotransmitters I.G.2. Inflammatory mediators I.G.3. Pain pathways Domain II. Imaging Safety (8%) II.A. Evaluation of equipment II.B. Equipment safety II.C. Radiation safety II.D. Safe practices with imaging equipment II.E. Provider and Staff safety II.F. Patient safety Domain III. Assessment/Diagnosis/Integration/Referral (24%) III.A. Physical examination III.B. Pain generators III.C. Health history III.D. Diagnostic studies III.D.1. MRI III.D.2. CT III.D.3. EMG III.D.4. X-ray III.D.5. Discogram III.E. Documentation III.F. Data interpretation III.G. Treatment plan III.H. Imaging strategies III.I. Clinical judgment III.J. Multidisciplinary collaboration 1 Nonsurgical Pain Management (NSPM) Content Outline and Exam Blueprint Effective through 2020 Domain IV. Pharmacological Treatment (15%) IV.A. Pharmacology and pain IV.A.1. NSAIDS IV.A.2. Opioids IV.A.3. -

Diagnostic Radiography Is the Production of High Quality Images for the Purpose of Diagnosis of Injury Or Disease
A Career in Medical Imaging What is Diagnostic Radiography / Medical Imaging? Diagnostic Radiography is the production of high quality images for the purpose of diagnosis of injury or disease. It is a pivotal aspect of medicine and a patient's diagnosis and ultimate treatment is often dependent on the images produced. Diagnostic Radiography uses both ionising and non-ionising radiation in the imaging process. The equipment used is at the high end of technology and computerisation within medicine. What does a Diagnostic Radiographer / Medical Imaging Technologist do? A Diagnostic Radiographer/Medical Imaging Technologist is a key member of the health care team. They are responsible for producing high quality medical images that assist medical specialists and practitioners to describe, diagnose, monitor and treat a patient’s injury or illness. Much of the medical equipment used to gain the images is highly technical and involves state of the art computerisation. A Diagnostic Radiographer/Medical Imaging Technologist needs to have the scientific and technological background to understand and use the equipment within a modern Radiology department as well as compassion and strong interpersonal skills. They need to be able to demonstrate care and understanding and have a genuine interest in a patient's welfare. The Diagnostic Radiographer/Medical Imaging Technologist will also need to be able to explain to the patient the need for the preparation and post examination care as well as the procedure to be undertaken. The Diagnostic Radiographer/Medical Imaging Technologist is able to work in a highly advanced technical profession that requires excellent people skills. It is an exciting and rewarding profession to embark on and great opportunities await the graduate. -

Imaging Services Order Guide Medicare Guidelines Require Explicit Written and Signed Provider Orders
Imaging Services 2021 Imaging Services Order Guide Medicare guidelines require explicit written and signed provider orders. This guide was created to assist you in ordering and authorizing exams accurately. Please obtain insurance authorizations before scheduling imaging studies. Call one of our licensed/certified technologists if you have questions or comments. NOTE: Please DO NOT call the department to schedule an appointment. CENTRALIZED SCHEDULING . 509-248-9592 GENERAL X-RAY . 509-895-0509 COMPUTED TOMOGRAPHY (CT) . 509-895-0507 MAGNETIC RESONANCE IMAGING (MRI) . 509-895-0505 NUCLEAR MEDICINE . 509-575-8099 `OHANA MAMMOGRAPHY . 509-574-3863 ULTRASOUND . 509-249-5154 VASCULAR ULTRASOUND–Memorial Heart & Vascular . 509-574-0243 VASCULAR STAT REFERRALS–Memorial Heart & Vascular . .509-494-0551 CARDIOVASCULAR SERVICES–Memorial Heart & Vascular . 509-574-0243 BONE DENSITY–Lakeview Campus . 509-972-1170 PROVIDER EMERGENCY . 509-248-7380 Option 0 Consultation of a Clinical Decision Support Mechanism is required to determine if advanced diagnostic imaging services (CT, MRI, Nuclear Medicine, PET) adheres to Appropriate Use Criteria. Order must include Decision Support Number (DSN), G-Code, and Modifier. PHONE | 509-895-0507 PHONE | 509-895-0507 2 3 CT/CAT Scan/Computed Tomography FAX | 509-576-6982 CT/CAT Scan/Computed Tomography FAX | 509-576-6982 *If patient is over 400 lbs., please call the CT department at 509-895-0507. *If patient is over 400 lbs., please call the CT department at 509-895-0507. Consultation of a Clinical Decision Support Mechanism is required. Order must include DSN, G-Code, and Modifier. Consultation of a Clinical Decision Support Mechanism is required. Order must include DSN, G-Code, and Modifier. -
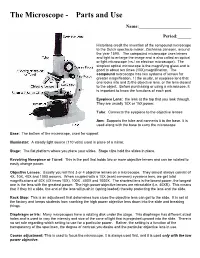
The Microscope Parts And
The Microscope Parts and Use Name:_______________________ Period:______ Historians credit the invention of the compound microscope to the Dutch spectacle maker, Zacharias Janssen, around the year 1590. The compound microscope uses lenses and light to enlarge the image and is also called an optical or light microscope (vs./ an electron microscope). The simplest optical microscope is the magnifying glass and is good to about ten times (10X) magnification. The compound microscope has two systems of lenses for greater magnification, 1) the ocular, or eyepiece lens that one looks into and 2) the objective lens, or the lens closest to the object. Before purchasing or using a microscope, it is important to know the functions of each part. Eyepiece Lens: the lens at the top that you look through. They are usually 10X or 15X power. Tube: Connects the eyepiece to the objective lenses Arm: Supports the tube and connects it to the base. It is used along with the base to carry the microscope Base: The bottom of the microscope, used for support Illuminator: A steady light source (110 volts) used in place of a mirror. Stage: The flat platform where you place your slides. Stage clips hold the slides in place. Revolving Nosepiece or Turret: This is the part that holds two or more objective lenses and can be rotated to easily change power. Objective Lenses: Usually you will find 3 or 4 objective lenses on a microscope. They almost always consist of 4X, 10X, 40X and 100X powers. When coupled with a 10X (most common) eyepiece lens, we get total magnifications of 40X (4X times 10X), 100X , 400X and 1000X.