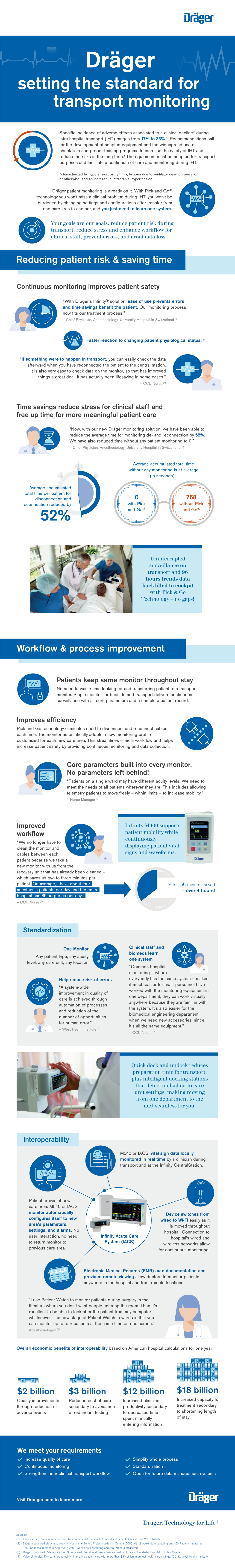
Dräger Setting the Standard for Transport Monitoring
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Origin of Bimaristans (Hospitals) in Islamic Medical History
The Origin of Bimaristans (Hospitals) in Islamic Medical History IMPORTANT NOTICE: Author: Dr. Sharif Kaf Al-Ghazal Chief Editor: Prof. Mohamed El-Gomati All rights, including copyright, in the content of this document are owned or controlled for these purposes by FSTC Limited. In Deputy Editor: Prof. Mohammed Abattouy accessing these web pages, you agree that you may only download the content for your own personal non-commercial Associate Editor: Dr. Salim Ayduz use. You are not permitted to copy, broadcast, download, store (in any medium), transmit, show or play in public, adapt or Release Date: April 2007 change in any way the content of this document for any other purpose whatsoever without the prior written permission of FSTC Publication ID: 682 Limited. Material may not be copied, reproduced, republished, Copyright: © FSTC Limited, 2007 downloaded, posted, broadcast or transmitted in any way except for your own personal non-commercial home use. Any other use requires the prior written permission of FSTC Limited. You agree not to adapt, alter or create a derivative work from any of the material contained in this document or use it for any other purpose other than for your personal non-commercial use. FSTC Limited has taken all reasonable care to ensure that pages published in this document and on the MuslimHeritage.com Web Site were accurate at the time of publication or last modification. Web sites are by nature experimental or constantly changing. Hence information published may be for test purposes only, may be out of date, or may be the personal opinion of the author. -

The Contemporary Physician Leader
White Paper The Contemporary Physician Leader By Miles Snowden, MD Optum www.optum.com/aco 800.765.6619 Page 1 The Contemporary Physician Leader White Paper The “Triple Aim”—a term coined by the Institute of Healthcare Improvement to embody the goals of better care, controlled costs and improved health—has become a rallying cry in the health care industry.1 As the health care market in the United States focuses on changing incentives to accomplish the Triple Aim, a new generation of better improved leaders is needed who can clinically and financially transform provider care health organizations. Chief medical officers (CMOs) and other physician leaders Triple in hospitals, group practices and integrated delivery systems have unique Aim qualifications that can allow them to take ownership of these important changes. However, their success in this new era will require that they controlled evolve away from the roles they have traditionally played. costs This paper will share the perspectives of five physician leaders who represent the contemporary physician leader. In doing so, it will discuss the skill set, experience and qualities physician executives need to lead their organizations’ conversion from volume to value. Physician executive roles continue to evolve The role of the physician executive has evolved over the years. The traditional physician leader in a hospital setting is a medical director. Medical directors were sometimes employed by facilities but often were independent, affiliated doctors. These providers served as liaisons between hospitals and the credentialed medical staff. They worked closely with hospital administrators but rarely had a seat at the executive table. -

Chief Physician and Surgeon
OPEN SPOT CONTINUOUS EXAMINATION FOR DEPARTMENT OF STATE HOSPITALS- ATASCADERO, COALINGA, METROPOLITAN, NAPA, AND PATTON CHIEF PHYSICIAN AND SURGEON www.dsh.ca.gov The State of California is an equal opportunity employer to all, regardless of age, ancestry, color, disability (mental and physical), exercising the right to family care and medical leave, gender, gender expression, gender identity, genetic information, marital status, medical condition, military or veteran status, national origin, political affiliation, race, religious creed, sex (includes pregnancy, childbirth, breastfeeding and related medical conditions), and sexual orientation. It is the objective of the State of California to achieve a drug-free state workplace. Any applicant for State employment will be expected to behave in accordance with this objective because the use of illegal drugs is inconsistent with the law of the State, the rules governing civil service, and the special trust placed in public servants. EXAMINATION TYPE This is an open examination for the Department of State Hospitals. Examination and/or Employment Applications will not be accepted on a promotional basis. Career credits do not apply. HOW TO APPLY Please submit an Examination and/or Employment Application (STD. 678) form to the address indicated below. DO NOT SUBMIT EXAMINATION AND/OR EMPLOYMENT APPLICATION FORMS TO THE CALIFORNIA DEPARTMENT OF HUMAN RESOURCES. NOTE: All Examination and/or Employment Application forms must include: “to” and “from” dates (month/day/year); time base; and civil service class titles. Examination and/or Employment Application forms received without this information will be rejected. Resumes will not be accepted in lieu of a completed Examination and/or Employment Application (STD. -

Credentials Policy
CREDENTIALS POLICY Deer Valley Medical Center John C. Lincoln Medical Center Scottsdale Osborn Medical Center Scottsdale Shea Medical Center Scottsdale Thompson Peak Medical Center Proposed April 11, 2018 Horty, Springer & Mattern, P.C. 259050.19 CREDENTIALS POLICY TABLE OF CONTENTS PAGE 1. GENERAL ..........................................................................................................................1 1.A. TIME LIMITS .........................................................................................................1 1.B. DELEGATION OF FUNCTIONS ..........................................................................1 1.C. CONFIDENTIALITY AND PEER REVIEW PROTECTION ...............................1 1.C.1. Confidentiality .............................................................................................1 1.C.2. Peer Review Protection ................................................................................2 1.D. INDEMNIFICATION..............................................................................................2 1.E. DEFINITIONS .........................................................................................................2 2. QUALIFICATIONS, CONDITIONS, AND RESPONSIBILITIES .............................7 2.A. QUALIFICATIONS ................................................................................................7 2.A.1. Threshold Eligibility Criteria .......................................................................7 2.A.2. Extension of Time Frame to Satisfy Board -

Uk Healthcare Medical Staff Bylaws
UNIVERSITY OF KENTUCKY UK HEALTHCARE MEDICAL STAFF BYLAWS ADOPTED AND APPROVED OCTOBER 11, 2010 AMENDED AND RESTATED DECEMBER 9, 2019 TABLE OF CONTENTS ARTICLE 1 DEFINITIONS ........................................................................................................... 1 ACGME ............................................................................................................................................. 1 Administration ................................................................................................................................... 1 Board of Trustees or Board ................................................................................................................ 1 Chair .................................................................................................................................................. 1 Chandler Hospital .............................................................................................................................. 1 Children’s Hospital ............................................................................................................................ 2 Chief Clinical Officer ........................................................................................................................ 2 Chief Medical Officer(s) .................................................................................................................... 2 Chief Nurse Executive ...................................................................................................................... -

Medical Books in the Byzantine World
EIKASMOS Quaderni Bolognesi di Filologia Classica Studi Online, 2 MEDICAL BOOKS IN THE BYZANTINE WORLD EDITED BY BARBARA ZIPSER BOLOGNA 2013 Medical books in the Byzantine world edited by BarbaraZipser Bologna 2013 o Eikasmós Online II ISSN 2282-2178 In memoriam David Bennett y Table of Contents Acknowledgments . vii List of figures. .xi List of abbreviations . xii 1. Prefatory note: the uses of medical manuscripts Peregrine Horden (RHUL and Oxford). .1 2. Byzantine medicine, genres, and the ravages of time Vivian Nutton (UCL) . 7 3. Disease and where to treat it: a Byzantine vade mecum Dionysios Stathakopoulos (KCL) . 19 4. Two Latin Pre-Salernitan medical manuals, the Liber passionalis and the Tereoperica (Ps. Petroncellus) Klaus-Dietrich Fischer (Mainz) . 35 5. The fate of a Greek medical handbook in the Medieval West: the Intro- duction, or the Physician ascribed to Galen Caroline Petit (ICS) . 57 6. Aristotle and the Caliph's Dream. Aspects of medical translations David Bennett (formerly NHS and RHUL) . 79 7. `Syriac' plant names in a fifteenth century Greek glossary (From the Wellcome Library Books and Manuscripts) Nikolaj Serikoff (Wellcome Library). .97 8. The Reception of Galen's Art of medicine in the Syriac Book of medicines Siam Bhayro (Exeter) . 123 9. Medieval hospital formularies: Byzantium and Islam compared Peregrine Horden (RHUL and Oxford) . 145 10. Cancerous cells, Neanderthal DNA and the tradition of Byzantine me- dicine. Textual criticism in philology and genomics Florian Markowetz (Cancer Research UK Cambridge and University of Cambridge) and Barbara Zipser (RHUL) . 165 Acknowledgements This volume originates from a conference on Byzantine Medical Manuals in Context, held in central London on the 19th of September 2009. -

JOURNAL of REHABILITATION the International JRM MEDICINE Non-Profit Journal VOL
JOURNAL OF REHABILITATION The International JRM MEDICINE Non-profit Journal VOL. 51. OCTOBER 2019 6th Baltic and North Sea Conference on Physical and Rehabilitation Medicine Rehabilitation towards future health and participa- tion - an evidence-based strategy Oslo, Norway, October 9–10, 2019 ABSTRACT BOOK Immediate Open Access Official journal of the – UEMS European Board and Section of Physical and Rehabilitation Medicine (EBPRM) – European Academy of Rehabilitation Medicine (EARM) – Baltic and North Sea Forum for Physical and Rehabilitation Medicine (BNFPRM) Published in association with the – European Society of Physical and Rehabilitation Medicine (ESPRM) – Canadian Association of Physical Medicine and Rehabilitation (CAPM&R) – Asia Oceania Society of Physical and Rehabilitation Medicine (AOSPRM) – Baltic and North Sea Forum for Physical and Rehabilitation Medicine (BNFPRM) Journal of Rehabilitation Medicine VOL. 51. OCTOBER 2019 Journal of Rehabilitation Medicine Journal of Rehabilitation Medicine is an international peer-review journal published in English with ten regular issues per year. It is owned by a Swedish nonprofit organi- zation: Foundation for Rehabilitation Information. Journal of Rehabilitation Medicine was former called Scandinavian Journal of Rehabilitation Medicine, which was founded by Olle Höök in 1968. The name was changed to Journal of Rehabilitation Medicine in 2001. Journal of Rehabilitation Medicine aims to be a leading worldwide forum for research in physical and rehabilitation medicine, aiming to increase -

The Journal of America's Physician Groups – Spring 2021 Edition
The Journal of Volume 15 • No. 1 • Spring 2021 COVER STORY: Member Spotlight Clive Fields, MD, p.18 Health Equity and Social Justice, p.24 The Latest on Alternative Payment Models, p.34 Serving those who provide care. IT’S IN OUR DNA. TDC Group is proud to be the exclusive sponsor of the podcast APG on American Healthcare. 7864_Journal_APG_Sponsor_Spr2021_0221_v4.indd 1 2/19/21 1:48 PM ON THE COVER 18 Clive Fields, MD The VillageMD Co-Founder explains how we can eliminate the barriers to advanced primary care. TABLE OF CONTENTS TABLE The Journal of DEPARTMENTS FEATURES 6 12 Publisher From the President New APG Manual Offers an Valerie Okunami Essential Guide to Risk Editor-in-Chief Contracting Don Crane 8 Editorial Advisory Board Lura Hawkins, MBA News and Events Dianne Glover, MPH Gregory Phillips 22 Managing Editor Improving Medication Adherence Lura Hawkins, MBA 10 During a Pandemic Contributing Writers From the BOD Chair Bill Barcellona Don Crane Lessons Learned From Sanjay Doddamani, MD the Pandemic Garrett Eberhardt 24 Clive Fields, MD New APG Collaborative Addresses Russ Foster Lura Hawkins, MBA Health Equity and Social Justice Jennifer Jackman 14 Dorothy Lockhart, MBA, MSN, RN Federal Policy Update Steve Neorr Gregory Phillips As COVID-19 Continues, 30 Valinda Rutledge Faith Saporsantos, MSN, MHA, RN, Physicians Still Need Relief Connecting Key Strategies CRRN to Promote Talent Management Sheila Stephens Bill Wulf, MD 16 Journal of America’s Physician Groups is published by Policy Briefing 34 Valerie Okunami Media California Bill Targets Health Is Wealth: The Latest PO Box 674, Sloughhouse, CA 95683 Healthcare Affordabilty on Alternative Payment Models Phone 916.761.1853 apg.org Please send press releases and editorial inquiries to [email protected] or 27 c/o Journal of America’s Physician Groups, APG Member List 915 Wilshire Blvd., Suite 1620, Los Angeles, CA 90017 For advertising, please send email to [email protected] Subscription rates: $32 per year; $58 two years; $3 single copy. -

STEMI ACCELERATOR-2: Regional Coordination Improves Outcomes
WEDNESDAY, NOVEMBER 15 DailyNewsNovember 11-15 | Anaheim, California Today’s highlights from 3 the program chair STEMI ACCELERATOR-2: Regional Queen Latifah honored for her 4 work promoting heart failure awareness coordination improves outcomes, Small case series challenges 6 thinking about fluoropyrimidine- FMC-to-device times in STEMI patients related cardiac toxicity egional training and coor- patients having a cath lab activated within 20 dination interventions that minutes of paramedic arrival. GEMINI-ACS-1: provide timely reperfusion “For the overall project, we increased from for ST-elevation myocardial 67 percent to 74 percent of patients reaching Switching P2Y12 infarction patients improve the national standard of first medical contact inhibitor in ACS outcomes and the interval of to device within 90 minutes. This coordina- patients based on first-medical-contact-to- tion of training was associated with signif- Rdevice time, according to a study present- icant reductions in heart failure and death, pharmacogenomic ed at Scientific Sessions on Tuesday. and demonstrated a marked and statistically testing results uncommon In the study, investigators worked with significant decline in mortality,” Jollis said. leaders, healthcare professionals, paramed- The study is a collaboration of Duke An update of the GEMINI-ACS-1 ics, nurses, emergency medicine physicians and the AHA’s Mission: Lifeline program. James G. Jollis, MD, FACC trial found that switching of P2Y12 in- and cardiologists in 12 major U.S. metropol- hibitors based on the results of pharma- itan regions to develop centralized STEMI ICARE-ACS cogenomics testing and reporting for plans for EMS catheterization lab activation Results of a New Zealand study suggest Patients with Possible Acute Coronary reduced or enhanced function alleles of and rapid transfer from non-PCI hospitals. -

FINAL-CMO-CNO-Letter-Masking
November 19, 2020 Dear Tennessee residents: The past several months have taken a toll on all of us, as we cope with the stress of quarantines, social distancing and other public health measures related to the COVID-19 pandemic. We miss our friends and family, we miss concerts and other events, we miss seeing smiles that are hidden by masks when we are at the grocery store, and we are heartbroken to have lost so many to this horrible disease. As clinicians in Tennessee hospitals, we feel it too. However, we are also impacted for other reasons. We are worried for our patients who were perfectly healthy just a week ago and are now dependent on a ventilator to breathe, saddened as we hold the phone while family members say their final goodbyes on FaceTime, and frustrated that simple steps that could greatly reduce the loss of life are not being embraced by all Tennesseans. We, the Chief Medical Officers and Chief Nursing Officers across the state of Tennessee, are banding together in one unified voice to say masking makes a difference. While nothing short of total isolation completely eliminates the risk of contracting or spreading COVID-19, we, as medical professionals, know that wearing a mask and maintaining social distancing does greatly reduce the risk. A cloth or surgical mask traps droplets that are released when the wearer talks, coughs or sneezes. These droplets are what spreads the virus between people. Containing the droplets helps stop the spread of COVID-19. More recent evidence further indicates that wearing a mask also protects the wearer by reducing the number of infectious droplets inhaled by the wearer. -

MEDICINE Buspring 2020 • Volume 104Et • Number 4 In
MEDICINE BuSpring 2020 • Volume 104et • Number 4 in THE GREATEST GOOD Maryland’s Center for Vaccine Development Innovations in Renal Transplantation Advancing the Field of Transplantation University of Maryland Medical Center Division of Transplantation recently concluded an eight-year study on the benefits of combining living donor kidney transplantation and panniculectomy. Guidelines suggest those with body mass index (BMI) >40 are less likely to benefit from transplantation. While nearly a quarter of those on the waiting list are categorized as obese, only 15% of renal transplants occur in obese patients. Obese and post-obese patients often have a large abdominal pannus, which may be prohibitive to transplantation. By using a multidisciplinary team to combine living donor renal transplant and panniculectomy, UMMC was able to greatly improve access to transplantation for the obese and post-obese population. This combined approach, unique to UMMC, yielded shorter- than-expected hospital stays and patients experienced excellent postoperative outcomes, and thus should be considered for patients in whom transplantation might otherwise be withheld on the basis of obesity. Transplant surgeons at UMMC prepare a living kidney donation for transplantation. Improving access to To refer a patient or consult with one of our physicians call 410-328-5408 transplantation Superior surgical Learn more at umm.edu/transplant expertise Visit our Physician Video Channel at physicians.umm.edu MEDICINE Bulletin Editorial Board Harry C. Knipp, ’76 Chairman Gary D. Plotnick, ’66 Vice Chairman John Allen, ’14 Frank M. Calia, MD, MACP Bu etin Triesta Fowler-Lee, ’99 Nidhi Goel, ’10 Christopher Hardwick Sachin D. Kalyani, ’03 8 Cover story George C. -
Healthcare Changes and New C-Suite Roles
HEALTHCARE CHANGES AND NEW C-SUITE ROLES BY BRIAN JUSTICE 30 Healthcare Executive MAY/JUNE 2009 The healthcare industry is officer, chief strategy officer, chief informatics officer and chief population health management officer. The predicted to represent 20 percent of GDP nascent state of these roles is recognized by many in the in the United States by 2025. Given the healthcare industry, including Kimberly A. Smith, man- aging partner in Academic Medicine and Health economic and societal import Sciences Practice, Witt/Kieffer, Oakbrook, Ill., and an of that fact, and the role healthcare ACHE Member. executives play in the well-being of the “These roles are emerging rapidly, and they are much, much more prevalent than they were just a year or two population, the successful navigation of a ago,” she says. “What continues to be less clear is the defi- landscape beset by disruptors is more nition of what each of these roles is. There is variability across them, but certainly what is happening in health- crucial than ever. care is what is driving these roles.” In 2015, ACHE conducted a survey of executive search A wide range of forces are buffeting our industry, firms that are members of the ACHE/Executive Search including changing delivery models, the rise of value- Firm Exchange on trends in recruiting healthcare leaders. based care and the omnipresence of data. Private The survey was the first of its kind developed by ACHE. industry is stepping in and causing jitters, too. Forty-three executive search firms were surveyed, with Amazon, Berkshire Hathaway and JPMorgan announced 35 responding.