Pediatric Epilepsy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 ILAE Classification & Definition of Epilepsy Syndromes in the Neonate
ILAE Classification & Definition of Epilepsy Syndromes in the Neonate and Infant: Position Statement by the ILAE Task Force on Nosology and Definitions Authors: Sameer M Zuberi1, Elaine Wirrell2, Elissa Yozawitz3, Jo M Wilmshurst4, Nicola Specchio5, Kate Riney6, Ronit Pressler7, Stephane Auvin8, Pauline Samia9, Edouard Hirsch10, O Carter Snead11, Samuel Wiebe12, J Helen Cross13, Paolo Tinuper14,15, Ingrid E Scheffer16, Rima Nabbout17 1. Paediatric Neurosciences Research Group, Royal Hospital for Children & Institute of Health & Wellbeing, University of Glasgow, Member of European Reference Network EpiCARE, Glasgow, UK. 2. Divisions of Child and Adolescent Neurology and Epilepsy, Department of Neurology, Mayo Clinic, Rochester MN, USA. 3. Isabelle Rapin Division of Child Neurology of the Saul R Korey Department of Neurology, Montefiore Medical Center, Bronx, NY USA. 4. Department of Paediatric Neurology, Red Cross War Memorial Children’s Hospital, Neuroscience Institute, University of Cape Town, South Africa. 5. Rare and Complex Epilepsy Unit, Department of Neuroscience, Bambino Gesu’ Children’s Hospital, IRCCS, Member of European Reference Network EpiCARE, Rome, Italy 6. Neurosciences Unit, Queensland Children's Hospital, South Brisbane, Queensland, Australia. Faculty of Medicine, University of Queensland, Queensland, Australia. 7. Clinical Neuroscience, UCL- Great Ormond Street Institute of Child Health, London, UK. Department of Clinical Neurophysiology, Great Ormond Street Hospital for Children NHS Foundation Trust, Member of European Reference Network EpiCARE London, UK 8. Université de Paris, AP-HP, Hôpital Robert-Debré, INSERM NeuroDiderot, DMU Innov-RDB, Neurologie Pédiatrique, Member of European Reference Network EpiCARE, Paris, France. 9. Department of Paediatrics and Child Health, Aga Khan University, East Africa. 1 10. Neurology Epilepsy Unit “Francis Rohmer”, INSERM 1258, FMTS, Strasbourg University, France. -

Pediatric Epilepsy Clips by Pediatric Elizabeth Medaugh, MSN, CPNP-PC , Pediatric Nurse Practitioner, Neurology
Nursing May 2016 Pediatric Clips Pediatric Nursing Pediatric Epilepsy Clips by Pediatric Elizabeth Medaugh, MSN, CPNP-PC , Pediatric Nurse Practitioner, Neurology Advanced Practice Sophia had been exceeding down to sleep, mother heard a Nurses at Dayton Case Study the expectations of school. thump and went to check on her. Her teachers report her being Sophia’s eyes were wide open Children’s provides Sophia is a 7 year old Caucasian focused the first two quarters, and deviated left, left arm was quick reviews of female who presented to her but have found her attention to stiffened with rhythmic shaking, be somewhat off over the last Sophia’s mouth was described common pediatric primary care physician with concerns of incontinence few weeks. Teachers have asked as “sort of twisted” and Sophia conditions. in sleep. Sophia is an parents if Sophia has been was drooling. The event lasted otherwise healthy child, with getting good rest as she has 90 seconds. Following, Sophia uncomplicated birth history, been falling asleep in class. was disoriented and very sleepy. Father reports his sister Dayton Children’s appropriate developmental Sophia’s mother and father had similar events as a child. progression with regards note that she has had is the region’s Sophia’s neurological exam to early milestones, and several episodes of urinary was normal, therefore her pediatric referral previously diurnal/nocturnally incontinence each week over pediatrician made a referral toilet trained. No report of the last 3-4 weeks. Parents center for a to pediatric neurology. Given recent illness, infection or ill have limited fluids prior to bed Sophia’s presentation, what 20-county area. -

Benign Rolandic Epilepsy
Benign Rolandic Epilepsy What is Benign Rolandic Epilepsy (BRE)? Benign Rolandic Epilepsy is a common, mild form of childhood epilepsy characterized by brief simple partial seizures involving the face and mouth, usually occuring at night or during the early morning hours. Seizures are the result of brief disruptions in the brain’s normal neuronal activity. Who gets this form of epilepsy? Children between the ages of three and 13 years, who have no neurological or intellectual deficit.The peak age of onset is from 9-10 years of age. BRE is more common in boys than girls. What kind of seizures occur? Typically, the child experiences a sensation then a twitching at the corner of their mouth. The jerking spreads to in- volve the tongue, cheeks and face on one side, resulting in speech arrest, problems with pronunciation and drooling. Or one side of the child’s face may feel paralyzed. Consciousness is retained. On occasion, the seizure may spread and cause the arms and legs on that side to stiffen and or jerk, or it may become a generalized tonic-clonic seizure that involves the whole body and a loss of consciousness. When do the seizures occur? Seizures tend to happen when the child is waking up or during certain stages of sleep. Seizures may be infrequent, or can happen many times a day. How is Benign Rolandic Epilepsy diagnosed? A child having such seizures is given an EEG test to confirm the diagnosis, a test that graphs the pattern of electrical activity in the brain. BRE has a typical EEG spike pattern—repetitive spike activity firing predominantly from the mid-temporal or parietal areas of the brain near the rolandic (motor) strip. -

A Small Number of People Have What Is Known As Reflex Epilepsy, In
A small number of people have what is known What are the features of reflex epilepsy? as reflex epilepsy, in which seizures are set off There are many different types of reflex by specific stimuli. These can include flashing epilepsy, depending on the area of the brain that lights, a flickering computer “monitor”, sudden is affected. Seizure stimuli may be very specific, noises, a particular piece of music, or the phone or they may be broad categories. They can ringing. Some people even have seizures when include: they think about a particular subject or see their own hand! flashing or flickering lights, including computer monitors or video games. This is What are other terms for reflex epilepsy? called photosensitive epilepsy. It is the most Other terms for reflex epilepsy that you may common childhood form of reflex epilepsy, come across include: and the child may eventually outgrow it. the sight of a particular pattern; this is called epilepsy with reflex seizures visual pattern reflex epilepsy sensory precipitation epilepsy thinking about certain things stimulus sensitive epilepsy performing a certain task, such as typing; this is called praxis-induced epilepsy There are also many terms for specific types of reading reflex epilepsy. language-related stimuli such as writing, listening to speech, singing, or reciting What causes reflex epilepsy? certain passages of music; this is called The seizure stimulus is not the underlying cause musicogenic epilepsy of the epilepsy. Rather, it sends a particular certain sounds; this is called audiogenic message to a sensitive, seizure-prone area of the epilepsy brain, excites the neurons there, and causes a surprises or startles seizure. -
EEG in the Diagnosis, Classification, and Management of Patients With
EEG IN THE DIAGNOSIS, J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2005.069245 on 16 June 2005. Downloaded from CLASSIFICATION, AND MANAGEMENT ii2 OF PATIENTS WITH EPILEPSY SJMSmith J Neurol Neurosurg Psychiatry 2005;76(Suppl II):ii2–ii7. doi: 10.1136/jnnp.2005.069245 he human electroencephalogram (EEG) was discovered by the German psychiatrist, Hans Berger, in 1929. Its potential applications in epilepsy rapidly became clear, when Gibbs and Tcolleagues in Boston demonstrated 3 per second spike wave discharge in what was then termed petit mal epilepsy. EEG continues to play a central role in diagnosis and management of patients with seizure disorders—in conjunction with the now remarkable variety of other diagnostic techniques developed over the last 30 or so years—because it is a convenient and relatively inexpensive way to demonstrate the physiological manifestations of abnormal cortical excitability that underlie epilepsy. However, the EEG has a number of limitations. Electrical activity recorded by electrodes placed on the scalp or surface of the brain mostly reflects summation of excitatory and inhibitory postsynaptic potentials in apical dendrites of pyramidal neurons in the more superficial layers of the cortex. Quite large areas of cortex—in the order of a few square centimetres—have to be activated synchronously to generate enough potential for changes to be registered at electrodes placed on the scalp. Propagation of electrical activity along physiological pathways or through volume conduction in extracellular spaces may give a misleading impression as to location of the source of the electrical activity. Cortical generators of the many normal and abnormal cortical activities recorded in the EEG are still largely unknown. -

A Clinical Guide to Epileptic Syndromes and Their Treatment
Published August 13, 2008 as 10.3174/ajnr.A1231 dures and principles of treatment. These chapters are particu- BOOK REVIEW larly important for readers unfamiliar with the overall clinical presentation of the epilepsies and their diagnostic evaluation. A Clinical Guide to Epileptic Omitting these topics was a certain pitfall that has been Syndromes and Their Treatment, avoided. Basic techniques used in the evaluation of patients with of epilepsy, including anatomic and functional neuroim- 2nd ed. aging, are also included. The discussion of the relative value of C.P. Panayiotopoulos, ed. London, UK: Springer-Verlag; 2007, 578 EEG and its problems is particularly valuable. pages, 100 illustrations, $99.00. Subsequent chapters are devoted to the meat of the book, the epilepsy syndromes. These are presented in age-based he syndromic classification of epileptic seizures has been chronologic order, beginning with syndromes in the neonate evolving for more than a quarter century. Piggy-backed T and infant and continuing through syndromes in adults. onto major advances in neurophysiology and neuroimaging, Complete coverage of reflex seizures and reflex epilepsies in the current nomenclature of specific clinical epilepsy syn- chapter 16 is particularly welcome. Chapter 17 covers a group dromes now supersedes earlier seizure classifications based of disorders that are associated with epileptic seizures. The exclusively on seizure types. The practice of epilepsy has thus chapter gives excellent coverage of these disorders but makes joined mainstream medicine through its newfound ability to no pretenses at being comprehensive. For example, coverage link the signs and symptoms of epilepsy with specific under- of important disorders with epilepsy such as the Wolf- lying disorders. -
Epilepsy in Childhood
Psychogenic Non-epileptic Seizures Dr Katharina Junejo Consultant Child and Adolescent Psychiatrist Aim Overview of basic principles in childhood epilepsy PNES Diagnosis of epilepsy Every child’s brain is capable of generating seizures with certain pro-convulsive drugs, acute metabolic disturbance, CNS infection, acute head trauma Risk of epilepsy after acute and provoked seizure is 3-5% Emotional stress is not considered provoking factor Henri Gastaut and colleagues proposed a classification of seizures: “all attempts at classification of seizures are hampered by our limited knowledge of the underlying pathological processes within the brain and that any classification must of necessity be a tentative one and will be subject to change with every advance in scientific understanding of epilepsy” (Gastaut et al 1964). Epilepsy has variable clinical presentations Convulsions (tonic- Staring spells clonic seizures) (absences) Period with confusion with or without Variants of automatism (complex paroxysmal events partial seizures) during sleep (common frontal lobe seizures) Limb or body jerk movements (myoclonus) Loss of speech/decline in Spasms (infantile or social, cognitive function Falls or drops epileptic spasms) (Landau-Kleffner (atonic but also syndrome) tonic seizures) ILAE Revised Terminology for Organization of Seizures and Epilepsies 2011 ‐ 2013 Classification of seizures: generalised and focal seizures Electroclinical syndromes and other epilepsies grouped by specificity of diagnosis (arranged by typical age of onset) Major conceptual changes: using aetiological classification of epilepsy-genetic, metabolic, immune, infectious and unknown causes Changes in terminology Operational diagnosis of epilepsy: occurrence of 2 or more unprovoked seizures, irrespective of seizure type (as recurrence risk is 80-90%) Careful history is only diagnostic test as many paroxysmal disorders that mimic epileptic seizures (most common vasovagal syncope or reflex anoxic seizure) Limitations of EEG: approx. -

Photosensitive Epilepsy
photosensitive epilepsy factsheet If you have epilepsy you may be able to identify triggers – situations that set off your seizures. Common triggers include stress or tiredness. If seizures are triggered by flashing lights 1 or certain patterns, this is called photosensitive epilepsy. how common is photosensitive epilepsy? how is photosensitive epilepsy treated? Around 1 in 100 people has epilepsy, and of these Photosensitive epilepsy usually responds well to people, around 3% have photosensitive epilepsy. anti-epileptic drugs (AEDs) that treat generalised Photosensitive epilepsy is more common in children seizures (seizures that affect both sides of the brain and young people (up to 5%) and is less commonly at once). diagnosed after the age of 20. See our booklet and chart medication for epilepsy for more information. how can I tell if I am photosensitive? Many people know this if they have a seizure Triggers are individual, but the following sources when they are exposed to flashing lights or patterns in themselves are not generally likely to trigger as a photosensitive trigger will usually cause photosensitive seizures. See over the page for a seizure straightaway. possible triggers and what increases the risk. An electroencephalogram (EEG) may include testing • UK TV programme content. Ofcom regulates for photosensitive epilepsy. This involves looking at a material shown on TV in the UK. The regulations light which will flash at different speeds. If this causes restrict the flash rate to three hertz or less, and any changes in brain activity the technician can stop they also restrict the area of screen allowed for the flashing light before a seizure develops. -

Prognostic Utility of Hypsarrhythmia Scoring in Children with West
Clinical Neurology and Neurosurgery 184 (2019) 105402 Contents lists available at ScienceDirect Clinical Neurology and Neurosurgery journal homepage: www.elsevier.com/locate/clineuro Prognostic utility of hypsarrhythmia scoring in children with West syndrome T after ketogenic diet ⁎ Yunjian Zhang1, Lifei Yu1, Yuanfeng Zhou, Linmei Zhang, Yi Wang, Shuizhen Zhou Department of Pediatric Neurology, Children’s Hospital of Fudan University, China ARTICLE INFO ABSTRACT Keywords: Objective: The aim of this study was to evaluate the clinical efficacy and electroencephalographic (EEG) changes West syndrome of West syndrome after ketogenic diet (KD) therapy and to explore the correlation of EEG features and clinical Ketogenic diet efficacy. EEG Patients and methods: We retrospectively studied 39 patients with West syndrome who accepted KD therapy from Hypsarrhythmia May 2011 to October 2017. Outcomes including clinical efficacy and EEG features with hypsarrhythmia severity scores were analyzed. Results: After 3 months of treatment, 20 patients (51.3%) had ≥50% seizure reduction, including 4 patients (10.3%) who became seizure-free. After 6 months of treatment, 4 patients remained seizure free, 12 (30.8%) had 90–99% seizure reduction, 8 (20.5%) had a reduction of 50–89%, and 15 (38.5%) had < 50% reduction. Hypsarrhythmia scores were significantly decreased at 3 months of KD. They were associated with seizure outcomes at 6 months independent of gender, the course of disease and etiologies. Patients with a hypsar- rhythmia score ≥8 at 3 months of therapy may not be benefited from KD. Conclusion: Our findings suggest a potential benefit of KD for patients with drug-resistant West syndrome. Early change of EEG after KD may be a predictor of a patient’s response to the therapy. -

Title in All Caps
Epilepsy Syndromes: Where does Dravet Syndrome fit in? Scott Demarest MD Assistant Professor, Departments of Pediatrics and Neurology University of Colorado School of Medicine Children's Hospital Colorado Disclosures Scott Demarest has consulted for Upsher-Smith on an unrelated subject matter. No conflicts of interest Objectives • What is an Epilepsy Syndrome? • How do we define epilepsy syndromes? • Genetic vs Phenotype (Features) • So what? Why do we care about Epilepsy Syndromes? • How do we organize and categorize Epilepsy Syndromes? • What epilepsy syndromes are similar to Dravet Syndrome and what is different about them? Good Resource International League Against Epilepsy Epilepsydiagnosis.org https://www.epilepsydiagnosis.org/syndrome/epilepsy- syndrome-groupoverview.html What is an Epilepsy Syndrome? A syndrome is a collection of common clinical traits. For Epilepsy this is usually about: • What type of seizures occur? • Age seizure start? Electroclinical • Development? Features or • What does the EEG look like? Phenotype • Other Co-morbidities… Course of an Epilepsy Syndrome Developmental Trajectories - Theoretical Model Normal Previously Normal with Epileptic Encephalopathy Development Never Normal Gray represents Epilepsy Onset the intensity of Age Epilepsy How distinct are Epilepsy Syndromes? A B C Many features might overlap, but the hope is that the cluster of symptoms are “specific” to that epilepsy syndrome…this is often better in theory than practice. How does the individual patient fit? A B C Is this patient at type A,B or C? What about Syndromes Defined by Genes? Is SCN1A the same as Dravet Syndrome? …I don’t have a perfect answer for this… many diseases are being defined by the gene (CDKL5, SCN8A, CHD2). -
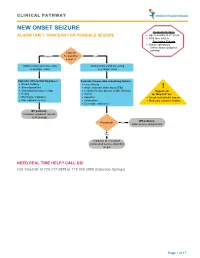
Seizure, New Onset
CLINICAL PATHWAY NEW ONSET SEIZURE Inclusion Criteria ALGORITHM 1. CONCERN FOR POSSIBLE SEIZURE • Age 6 months to 21 years • First-time seizure Exclusion Criteria • Status epilepticus (refer to status epilepticus pathway) Concern Unsure for possible Yes seizure? Obtain history and screening Obtain history and screening neurologic exam neurologic exam Consider differential diagnoses: Evaluate for possible provoking factors: • Breath holding • Fever/illness • Stereotypies/tics • Acute traumatic brain injury (TBI) ! • Vasovagal/syncope/vertigo • Central nervous system (CNS) infection Urgent call • Reflux • Tumor to ‘OneCall’ for: • Electrolyte imbalance • Ingestion • Suspected infantile spasm • Non epileptic seizure • Intoxication • Medically complex children • Electrolyte imbalance Off pathway: Consider outpatient referral to Neurology Off pathway: Provoked? Yes Address provoking factors No Continue to new onset unprovoked seizure algorithm on p.2 NEED REAL TIME HELP? CALL US! Call ‘OneCall’ at 720-777-3999 or 719-305-3999 (Colorado Springs) Page 1 of 17 CLINICAL PATHWAY ALGORITHM 2. NEW ONSET UNPROVOKED SEIZURE Inclusion Criteria • Age 6 months to 21 years New onset unprovoked • First-time unprovoked seizure seizure • Newly recognized seizure or epilepsy syndrome Exclusion Criteria • Provoked seizure: any seizure as a symptom of fever/illness, acute traumatic brain injury (TBI), Has central nervous system (CNS) infection, tumor, patient returned ingestion, intoxication, or electrolyte imbalance Consult inpatient • to baseline within No -

The Relationship Between the Components of Idiopathic Focal Epilepsy
Journal of Pediatrics and Neonatal Care Review Article Open Access The relationship between the components of idiopathic focal epilepsy Abstract Volume 8 Issue 3 - 2018 The classification of epileptic syndromes in children is not a simple duty, it requires Cesar Ramon Romero Leguizamon a great clinical ability as well as some degree of experience. Until today there is no Department of Drug Design and Pharmacology, University of international consensus regarding the different diseases that are part of the Idiopathic Copenhagen, Denmark Focal Epilepsies However, these diseases are the most prevalent in children suffering from some type of epilepsy, for this reason it is important to know more about these, Correspondence: Cesar Ramon Romero Leguizamon their clinical characteristics, pathological findings in studies such as encephalogram, M.D., Department of Drug Design and Pharmacology Faculty resonance, polysomnography and others. In the same way, to explore the possible of Health and Medical Science, University of Copenhagen, genetic origins of many of these pathologies, that have been little explored and Denmark, Jagtev 160, 2100 Copenhagen, Denmark, become an important therapeutic goal. A description of the most relevant aspects of Email [email protected] atypical benign partial epilepsy, Landau-Kleffner syndrome, benign epilepsy with centrotemporal spikes, electrical status epilepticus during sleep and Panayiotopoulos Received: February 17, 2018 | Published: May 14, 2018 syndrome is presented in this review, Allowing physicians and family members of children suffering from these diseases to have a better understanding and establish in this way a better diagnosis and treatment in patients, as well as promote in the scientific community the interest to investigate more about these relevant pathologies in childhood.