Mithramycin and Analogs for Overcoming Cisplatin Resistance in Ovarian Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Combination of Cabazitaxel and Plicamycin Induces Cell Death in Drug Resistant B-Cell Acute Lymphoblastic Leukemia
Clinical and Translational Science Institute Centers 9-1-2018 Combination of cabazitaxel and plicamycin induces cell death in drug resistant B-cell acute lymphoblastic leukemia Rajesh R. Nair West Virginia University Debbie Piktel West Virginia University Werner J. Geldenhuys West Virginia University Laura F. Gibson West Virginia University Follow this and additional works at: https://researchrepository.wvu.edu/ctsi Part of the Medicine and Health Sciences Commons Digital Commons Citation Nair, Rajesh R.; Piktel, Debbie; Geldenhuys, Werner J.; and Gibson, Laura F., "Combination of cabazitaxel and plicamycin induces cell death in drug resistant B-cell acute lymphoblastic leukemia" (2018). Clinical and Translational Science Institute. 34. https://researchrepository.wvu.edu/ctsi/34 This Article is brought to you for free and open access by the Centers at The Research Repository @ WVU. It has been accepted for inclusion in Clinical and Translational Science Institute by an authorized administrator of The Research Repository @ WVU. For more information, please contact [email protected]. HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Leuk Res Manuscript Author . Author manuscript; Manuscript Author available in PMC 2019 September 01. Published in final edited form as: Leuk Res. 2018 September ; 72: 59–66. doi:10.1016/j.leukres.2018.08.002. Combination of cabazitaxel and plicamycin induces cell death in drug resistant B-cell acute lymphoblastic leukemia Rajesh R. Naira, Debbie Piktelb, Werner J. Geldenhuysc, -

PEMD-91-12BR Off-Label Drugs: Initial Results of a National Survey
11 1; -- __...._-----. ^.-- ______ -..._._ _.__ - _........ - t Ji Jo United States General Accounting Office Washington, D.C. 20648 Program Evaluation and Methodology Division B-242851 February 25,199l The Honorable Edward M. Kennedy Chairman, Committee on Labor and Human Resources United States Senate Dear Mr. Chairman: In September 1989, you asked us to conduct a study on reimbursement denials by health insurers for off-label drug use. As you know, the Food and Drug Administration designates the specific clinical indications for which a drug has been proven effective on a label insert for each approved drug, “Off-label” drug use occurs when physicians prescribe a drug for clinical indications other than those listed on the label. In response to your request, we surveyed a nationally representative sample of oncologists to determine: . the prevalence of off-label use of anticancer drugs by oncologists and how use varies by clinical, demographic, and geographic factors; l the extent to which third-party payers (for example, Medicare intermediaries, private health insurers) are denying payment for such use; and l whether the policies of third-party payers are influencing the treatment of cancer patients. We randomly selected 1,470 members of the American Society of Clinical Oncologists and sent them our survey in March 1990. The sam- pling was structured to ensure that our results would be generalizable both to the nation and to the 11 states with the largest number of oncologists. Our response rate was 56 percent, and a comparison of respondents to nonrespondents shows no noteworthy differences between the two groups. -

Consumer Medicine Information
DBL™ Docetaxel Concentrated Injection docetaxel Consumer Medicine Information What is in this leaflet It works by stopping cells from • wheezing or difficulty breathing growing and multiplying. or a tight feeling in your chest This leaflet answers some common Ask your doctor if you have any • swelling of the face, lips, tongue questions about DBL Docetaxel, questions about why this medicine or other parts of the body Concentrated Injection. has been prescribed for you. • rash, itching, hives or flushed, red It does not contain all the available Your doctor may have prescribed it skin information. It does not take the for another reason. • dizziness or light-headedness place of talking to your doctor or This medicine is not addictive. • back pain pharmacist. This medicine is available only with Do not use DBL Docetaxel, All medicines have risks and a doctor’s prescription. benefits. Your doctor has weighed Concentrated Injection if you have, You may have taken another the risks of you taking DBL or have had, any of the following Docetaxel, Concentrated Injection medicine to treat your breast, non medical conditions: small cell lung cancer, ovarian, against the benefits they expect it • severe liver problems prostate or head and neck cancer. will have for you. • blood disorder with a reduced However, your doctor has now number of white blood cells If you have any concerns about decided to treat you with docetaxel. taking this medicine, ask your There is not enough information to Do not use this medicine if you are doctor or pharmacist. recommend the use of this medicine pregnant or intend to become Keep this leaflet with the medicine. -
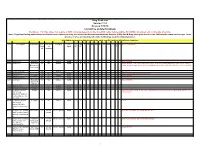
Drug Code List Version 11.4 Revised 5/18/18 List Will Be Updated Routinely
Drug Code List Version 11.4 Revised 5/18/18 List will be updated routinely Disclaimer: For drug codes that require an NDC, coverage depends on the drug NDC status (rebate eligible, Non-DESI, non-termed, etc) on the date of service. Note: Physician/Facility-administered medications are reimbursed using the Centers for Medicare and Medicaid Services (CMS) Part B Drug pricing file found on the CMS website--www.cms.hhs.gov. In the absence of a fee, pricing may reflect the methodolgy used for retail pharmacies. Highlights represent updated material for each specific revision of the Drug Code List. Code Description Brand Name NDC NDC unit Category Service AC CAH P NP MW MH HS PO OPH HI IDT DC Special Instructions Requir of Limits OP OP F ed measure 90281 human ig, im Gamastan Yes ML Antisera NONE X X X X Closed 3/31/13. 90283 human ig, iv Gamimune, Yes ML Antisera NONE X X X X Closed 3/31/13. Cost invoice required with claim. Restricted to ICD-9 diagnoses codes 204.10 - 204.12, Flebogamma, 279.02, 279.04, 279.06, 279.12, 287.31, and 446.1, and must be included on claim form, effective 10/1/09. Gammagard 90287 botulinum antitoxin N/A Antisera Not Covered 90288 botulism ig, iv No ML NONE X X X X Requires documentation and medical review 90291 cmv ig, iv Cytogam Yes ML Antisera NONE X X X X Closed 3/31/13. 90296 diphtheria antitoxin No ML NONE X X X X 90371 hep b ig, im Bayhep B, Yes ML Antisera NONE X X X X Closed 3/31/13. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM LIDADRONICUM 63132-38-7 ABAFUNGIN 129639-79-8 ACIDUM SALCAPROZICUM 183990-46-7 ABAMECTIN 65195-55-3 ACIDUM SALCLOBUZICUM 387825-03-8 ABANOQUIL 90402-40-7 ACIFRAN 72420-38-3 ABAPERIDONUM 183849-43-6 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABATACEPTUM 332348-12-6 ACITEMATE 101197-99-3 ABCIXIMAB 143653-53-6 ACITRETIN 55079-83-9 ABECARNIL 111841-85-1 ACIVICIN 42228-92-2 ABETIMUSUM 167362-48-3 ACLANTATE 39633-62-0 ABIRATERONE 154229-19-3 ACLARUBICIN 57576-44-0 ABITESARTAN 137882-98-5 ACLATONIUM NAPADISILATE 55077-30-0 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURINUM 178535-93-8 ACOLBIFENUM 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDUM 185106-16-5 ACAMPROSATE 77337-76-9 -

Identification of Inhibitors of Ovarian Cancer Stem-Like Cells by High-Throughput Screening Roman Mezencev, Lijuan Wang and John F Mcdonald*
Mezencev et al. Journal of Ovarian Research 2012, 5:30 http://www.ovarianresearch.com/content/5/1/30 RESEARCH Open Access Identification of inhibitors of ovarian cancer stem-like cells by high-throughput screening Roman Mezencev, Lijuan Wang and John F McDonald* Abstract Background: Ovarian cancer stem cells are characterized by self-renewal capacity, ability to differentiate into distinct lineages, as well as higher invasiveness and resistance to many anticancer agents. Since they may be responsible for the recurrence of ovarian cancer after initial response to chemotherapy, development of new therapies targeting this special cellular subpopulation embedded within bulk ovarian cancers is warranted. Methods: A high-throughput screening (HTS) campaign was performed with 825 compounds from the Mechanistic Set chemical library [Developmental Therapeutics Program (DTP)/National Cancer Institute (NCI)] against ovarian cancer stem-like cells (CSC) using a resazurin-based cell cytotoxicity assay. Identified sets of active compounds were projected onto self-organizing maps to identify their putative cellular response groups. Results: From 793 screening compounds with evaluable data, 158 were found to have significant inhibitory effects on ovarian CSC. Computational analysis indicates that the majority of these compounds are associated with mitotic cellular responses. Conclusions: Our HTS has uncovered a number of candidate compounds that may, after further testing, prove effective in targeting both ovarian CSC and their more differentiated progeny. Keywords: High-throughput screening, Ovarian cancer, Cancer stem cells Background alternative strategies. One approach has been to evaluate Ovarian cancer is the most lethal of gynecological can- molecules known to be inhibitory against pathways cers [1] despite its typically high initial response rate to believed to be deregulated in CSC (e.g., the Hedgehog, chemotherapy [2]. -

Prevalence and Safety of Off-Label Use of Chemotherapeutic Agents in Older Patients with Breast Cancer: Estimates from SEER-Medicare Data
Supplemental online content for: Prevalence and Safety of Off-Label Use of Chemotherapeutic Agents in Older Patients With Breast Cancer: Estimates From SEER-Medicare Data Anne A. Eaton, MS; Camelia S. Sima, MD, MS; and Katherine S. Panageas, DrPH J Natl Compr Canc Netw 2016;14(1):57–65 • eAppendix 1: J-Codes Representing Intravenous Chemotherapy • eAppendix 2: Established Sequential Adjuvant Chemotherapy Regimens for Breast Cancer • eTable 1: Patient Characteristics © JNCCN—Journal of the National Comprehensive Cancer Network | Volume 14 Number 1 | January 2016 Eaton et al - 1 eAppendix 1: J-Codes Representing Intravenous Chemotherapy J-Code Agent J-Code Agent J9000 Injection, doxorubicin HCl, 10 mg J9165 Injection, diethylstilbestrol diphosphate, 250 J9001 Injection, doxorubicin HCl, all lipid mg formulations, 10 mg J9170 Injection, docetaxel, 20 mg J9010 Injection, alemtuzumab, 10 mg J9171 Injection, docetaxel, 1 mg J9015 Injection, aldesleukin, per single use vial J9175 Injection, Elliotts’ B solution, 1 ml J9017 Injection, arsenic trioxide, 1 mg J9178 Injection, epirubicin HCl, 2 mg J9020 Injection, asparaginase, 10,000 units J9179 Injection, eribulin mesylate, 0.1 mg J9025 Injection, azacitidine, 1 mg J9180 Epirubicin HCl, 50 mg J9027 Injection, clofarabine, 1 mg J9181 Injection, etoposide, 10 mg J9031 BCG (intravesical) per instillation J9182 Etoposide, 100 mg J9033 Injection, bendamustine HCl, 1 mg J9185 Injection, fludarabine phosphate, 50 mg J9035 Injection, bevacizumab, 10 mg J9190 Injection, fluorouracil, 500 mg J9040 Injection, -

Chemotherapy and Polyneuropathies Grisold W, Oberndorfer S Windebank AJ European Association of Neurooncology Magazine 2012; 2 (1) 25-36
Volume 2 (2012) // Issue 1 // e-ISSN 2224-3453 Neurology · Neurosurgery · Medical Oncology · Radiotherapy · Paediatric Neuro- oncology · Neuropathology · Neuroradiology · Neuroimaging · Nursing · Patient Issues Chemotherapy and Polyneuropathies Grisold W, Oberndorfer S Windebank AJ European Association of NeuroOncology Magazine 2012; 2 (1) 25-36 Homepage: www.kup.at/ journals/eano/index.html OnlineOnline DatabaseDatabase FeaturingFeaturing Author,Author, KeyKey WordWord andand Full-TextFull-Text SearchSearch THE EUROPEAN ASSOCIATION OF NEUROONCOLOGY Member of the Chemotherapy and Polyneuropathies Chemotherapy and Polyneuropathies Wolfgang Grisold1, Stefan Oberndorfer2, Anthony J Windebank3 Abstract: Peripheral neuropathies induced by taxanes) immediate effects can appear, caused to be caused by chemotherapy or other mecha- chemotherapy (CIPN) are an increasingly frequent by different mechanisms. The substances that nisms, whether treatment needs to be modified problem. Contrary to haematologic side effects, most frequently cause CIPN are vinca alkaloids, or stopped due to CIPN, and what symptomatic which can be treated with haematopoetic taxanes, platin derivates, bortezomib, and tha- treatment should be recommended. growth factors, neither prophylaxis nor specific lidomide. Little is known about synergistic neu- Possible new approaches for the management treatment is available, and only symptomatic rotoxicity caused by previously given chemo- of CIPN could be genetic susceptibility, as there treatment can be offered. therapies, or concomitant chemotherapies. The are some promising advances with vinca alka- CIPN are predominantly sensory, duration-of- role of pre-existent neuropathies on the develop- loids and taxanes. Eur Assoc Neurooncol Mag treatment-dependent neuropathies, which de- ment of a CIPN is generally assumed, but not 2012; 2 (1): 25–36. velop after a typical cumulative dose. Rarely mo- clear. -

Multistage Delivery of Active Agents
111111111111111111111111111111111111111111111111111111111111111111111111111111 (12) United States Patent (io) Patent No.: US 10,143,658 B2 Ferrari et al. (45) Date of Patent: Dec. 4, 2018 (54) MULTISTAGE DELIVERY OF ACTIVE 6,355,270 B1 * 3/2002 Ferrari ................. A61K 9/0097 AGENTS 424/185.1 6,395,302 B1 * 5/2002 Hennink et al........ A61K 9/127 (71) Applicants:Board of Regents of the University of 264/4.1 2003/0059386 Al* 3/2003 Sumian ................ A61K 8/0241 Texas System, Austin, TX (US); The 424/70.1 Ohio State University Research 2003/0114366 Al* 6/2003 Martin ................. A61K 9/0097 Foundation, Columbus, OH (US) 424/489 2005/0178287 Al* 8/2005 Anderson ............ A61K 8/0241 (72) Inventors: Mauro Ferrari, Houston, TX (US); 106/31.03 Ennio Tasciotti, Houston, TX (US); 2008/0280140 Al 11/2008 Ferrari et al. Jason Sakamoto, Houston, TX (US) FOREIGN PATENT DOCUMENTS (73) Assignees: Board of Regents of the University of EP 855179 7/1998 Texas System, Austin, TX (US); The WO WO 2007/120248 10/2007 Ohio State University Research WO WO 2008/054874 5/2008 Foundation, Columbus, OH (US) WO WO 2008054874 A2 * 5/2008 ............... A61K 8/11 (*) Notice: Subject to any disclaimer, the term of this OTHER PUBLICATIONS patent is extended or adjusted under 35 U.S.C. 154(b) by 0 days. Akerman et al., "Nanocrystal targeting in vivo," Proc. Nad. Acad. Sci. USA, Oct. 1, 2002, 99(20):12617-12621. (21) Appl. No.: 14/725,570 Alley et al., "Feasibility of Drug Screening with Panels of Human tumor Cell Lines Using a Microculture Tetrazolium Assay," Cancer (22) Filed: May 29, 2015 Research, Feb. -

Chemotherapy Protocol
Chemotherapy Protocol BREAST CANCER CYCLOPHOSPHAMIDE-DOCETAXEL-DOXORUBICIN (TAC) Regimen Breast Cancer – Cyclophosphamide-Docetaxel-Doxorubicin (TAC) Indication Adjuvant therapy for node positive early breast cancer WHO Performance status 0, 1, 2 Toxicity Drug Adverse Effect Cyclophosphamide Dysuria, haemorrhagic cystitis, taste disturbances Hypersensitivity, fluid retention, neuropathy, joint pains, nail Docetaxel changes, fatigue Doxorubicin Cardio toxicity, urinary discolourisation (red) The adverse effects listed are not exhaustive. Please refer to the relevant Summary of Product Characteristics for full details. Monitoring Regimen FBC, U&E’s and LFT’s prior to each cycle. Ensure adequate cardiac function before starting treatment. Baseline LVEF should be measured, particularly in patients with a history of cardiac problems or in the elderly. Dose Modifications The dose modifications listed are for haematological, liver and renal function only. Dose adjustments may be necessary for other toxicities as well. In principle all dose reductions due to adverse drug reactions should not be re- escalated in subsequent cycles without consultant approval. It is also a general rule for chemotherapy that if a third dose reduction is necessary treatment should be stopped. Version 1.1 (Aug 2014) Page 1 of 8 Breast – Cyclophosphamide-Docetaxel-Doxorubicin (TAC) Please discuss all dose reductions / delays with the relevant consultant before prescribing if appropriate. The approach may be different depending on the clinical circumstances. The following is a general guide only. Haematological Prior to prescribing the following treatment criteria must be met on day one of treatment. Criteria Eligible Level Neutrophil equal to or more than 1x109/L Platelets equal to or more than 100x109/L Consider blood transfusion if patient symptomatic of anaemia or has a haemoglobin of less than 8g/dL If counts on day one are below these criteria for neutrophils and/or platelets then delay treatment for seven days. -

Innovative Design of Early Phase Clinical Trials in Radiation Oncology
Integration of chemotherapy and radiation therapy Adam P. Dicker, M.D., Ph.D. Chair, Department of Radiation Oncology Kimmel Cancer Center Jefferson Medical College of Thomas Jefferson University Philadelphia, PA No Disclosures 2 U.S. Cancer Statistics - 1998 1.2 Million New Cases Each Year 600,000 600,000 Localized Disseminated Tumors Tumors 570,000 Cured 70,000 Cured Via Surgery or Via Radiotherapy Chemotherapy Outline • Current Status • Rationale for combination of chemotherapy with Radiation • Mechanism of action and resistance • Disease sites and toxicity of combination therapies • New targets 4 The past decade • Radiotherapy has Improved & will Improve Further • Most Recent Advances Relate to Imaging & Planning • Future Advances will be in New Delivery Approaches • RT Dose and Fractionation Paradigms will Shift • RT Target Volume “Rules” will Also Shift • RT/Drug Interactions Could Dictate Dose & Fractionation Therapeutic Ratio Curves Reasons to use Chemoradiation • Sterilize micrometastases outside of the XRT portal • Tumor cell sensitization • Improved nutrition and reoxygenation to hypoxic tumor cell (decrease tumor burden) – Better blood supply to remaining tumor cells • Cells cycle into a more radiation sensitive phase • Inhibit cell division between radiation doses • Inhibit cellular repair of damage between therapies Rationale for combined chemotherapy and radiotherapy • Spatial cooperation • Toxicity independence • Action as a radiosensitizer (possible synergism) • Eliminate need for surgical procedure. – Not all patients -

Testimony of Manon Ress on Behalf of the Union for Affordable Cancer Treatment (UACT)
Testimony of Manon Ress on behalf of the Union for Affordable Cancer Treatment (UACT) United States International Trade Commission (USITC) hearing on "Economic Impact of Trade Agreements Implemented Under Trade Authorities Procedure, 2016 Report. Inv. No.: 332-555 November 17, 2015 The Union for Affordable Cancer Treatment (UACT), is an international network of people who share *he conviction that cancer treatment and care should be available everywhere for everyone, regardless of gender, age, nationality, or financial resources. Our web page is http://cancerunion.org. We are a union of people - people affected by cancer, their family members and friends, people who take care of people with cancer, health care professionals and cancer researchers - committed to increasing access to effective cancer treatment and care. I myself am a stage IV HER2 positive breast cancer patient in active treatment since May 2010. I am extremely fortunate to have access to the most advanced cancer treatment available. Thanks to successful and efficient treatments, my cancer as for many cancer patients has become a chronic disease. It is costly and will be more and more costly for all of us as the price of insurance will increase to keep up with the many cancer patients living for longer and longer time. We believe that cancer medicines and other essential medical tools, such as diagnostic tests, should be affordable. They are not, and things are getting worse. Like many patients, caregivers, doctors, insurers... and policymakers, we are extremely concerned about the rapidly escalating cost of cancer medication. For example, according to one large private payer of health care: the average per cycle cost of cancer drugs in 2014 was almost $18,650.