Sex Differences in Urate Handling
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Viewed Under 23 (B) Or 203 (C) fi M M Male Cko Mice, and Largely Unaffected Magni Cation; Scale Bars, 500 M (B) and 50 M (C)
BRIEF COMMUNICATION www.jasn.org Renal Fanconi Syndrome and Hypophosphatemic Rickets in the Absence of Xenotropic and Polytropic Retroviral Receptor in the Nephron Camille Ansermet,* Matthias B. Moor,* Gabriel Centeno,* Muriel Auberson,* † † ‡ Dorothy Zhang Hu, Roland Baron, Svetlana Nikolaeva,* Barbara Haenzi,* | Natalya Katanaeva,* Ivan Gautschi,* Vladimir Katanaev,*§ Samuel Rotman, Robert Koesters,¶ †† Laurent Schild,* Sylvain Pradervand,** Olivier Bonny,* and Dmitri Firsov* BRIEF COMMUNICATION *Department of Pharmacology and Toxicology and **Genomic Technologies Facility, University of Lausanne, Lausanne, Switzerland; †Department of Oral Medicine, Infection, and Immunity, Harvard School of Dental Medicine, Boston, Massachusetts; ‡Institute of Evolutionary Physiology and Biochemistry, St. Petersburg, Russia; §School of Biomedicine, Far Eastern Federal University, Vladivostok, Russia; |Services of Pathology and ††Nephrology, Department of Medicine, University Hospital of Lausanne, Lausanne, Switzerland; and ¶Université Pierre et Marie Curie, Paris, France ABSTRACT Tight control of extracellular and intracellular inorganic phosphate (Pi) levels is crit- leaves.4 Most recently, Legati et al. have ical to most biochemical and physiologic processes. Urinary Pi is freely filtered at the shown an association between genetic kidney glomerulus and is reabsorbed in the renal tubule by the action of the apical polymorphisms in Xpr1 and primary fa- sodium-dependent phosphate transporters, NaPi-IIa/NaPi-IIc/Pit2. However, the milial brain calcification disorder.5 How- molecular identity of the protein(s) participating in the basolateral Pi efflux remains ever, the role of XPR1 in the maintenance unknown. Evidence has suggested that xenotropic and polytropic retroviral recep- of Pi homeostasis remains unknown. Here, tor 1 (XPR1) might be involved in this process. Here, we show that conditional in- we addressed this issue in mice deficient for activation of Xpr1 in the renal tubule in mice resulted in impaired renal Pi Xpr1 in the nephron. -

Differential Expression of Hydroxyurea Transporters in Normal and Polycythemia Vera Hematopoietic Stem and Progenitor Cell Subpopulations
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2021 Differential expression of hydroxyurea transporters in normal and polycythemia vera hematopoietic stem and progenitor cell subpopulations Tan, Ge ; Meier-Abt, Fabienne Abstract: Polycythemia vera (PV) is a myeloproliferative neoplasm marked by hyperproliferation of the myeloid lineages and the presence of an activating JAK2 mutation. Hydroxyurea (HU) is a standard treat- ment for high-risk patients with PV. Because disease-driving mechanisms are thought to arise in PV stem cells, effective treatments should target primarily the stem cell compartment. We tested for theantipro- liferative effect of patient treatment with HU in fluorescence-activated cell sorting-isolated hematopoietic stem/multipotent progenitor cells (HSC/MPPs) and more committed erythroid progenitors (common myeloid/megakaryocyte-erythrocyte progenitors [CMP/MEPs]) in PV using RNA-sequencing and gene set enrichment analysis. HU treatment led to significant downregulation of gene sets associated with cell proliferation in PV HSCs/MPPs, but not in PV CMP/MEPs. To explore the mechanism underlying this finding, we assessed for expression of solute carrier membrane transporters, which mediate trans- membrane movement of drugs such as HU into target cells. The active HU uptake transporter OCTN1 was upregulated in HSC/MPPs compared with CMP/MEPs of untreated patients with PV, and the HU diffusion facilitator urea transporter B (UTB) was downregulated in HSC/MPPs compared withCM- P/MEPs in all patient and control groups tested. These findings indicate a higher accumulation ofHU within PV HSC/MPPs compared with PV CMP/MEPs and provide an explanation for the differential effects of HU in HSC/MPPs and CMP/MEPs of patients with PV. -

Activity-Dependent Regulation of Prestin Expression in Mouse Outer Hair Cells
J Neurophysiol 113: 3531–3542, 2015. First published March 25, 2015; doi:10.1152/jn.00869.2014. Activity-dependent regulation of prestin expression in mouse outer hair cells Yohan Song, Anping Xia, Hee Yoon Lee, Rosalie Wang, Anthony J. Ricci, and John S. Oghalai Department of Otolaryngology-Head and Neck Surgery, Stanford University, Stanford, California Submitted 4 November 2014; accepted in final form 19 March 2015 Song Y, Xia A, Lee HY, Wang R, Ricci AJ, Oghalai JS. patch-clamp recording conditions (Kakehata and Santos-Sac- Activity-dependent regulation of prestin expression in mouse outer chi, 1995 and 1996; Santos-Sacchi 1991; Santos-Sacchi et al. hair cells. J Neurophysiol 113: 3531–3542, 2015. First published 1998a). Thus, measuring the NLC is a common way of assess- March 25, 2015; doi:10.1152/jn.00869.2014.—Prestin is a membrane protein necessary for outer hair cell (OHC) electromotility and normal ing the amount of functional prestin within an OHC (Abe et al. 2007; Oliver and Fakler 1999;). hearing. Its regulatory mechanisms are unknown. Several mouse Downloaded from models of hearing loss demonstrate increased prestin, inspiring us to There are many ways to modulate the voltage dependence of investigate how hearing loss might feedback onto OHCs. To test force production by prestin protein within the plasma mem- whether centrally mediated feedback regulates prestin, we developed brane, such as changing the surrounding lipid environment, a novel model of inner hair cell loss. Injection of diphtheria toxin (DT) intracellular Ca2ϩ level, membrane tension, membrane poten- into adult CBA mice produced significant loss of inner hair cells tial, and ionic composition of the intracellular and extracellular without affecting OHCs. -
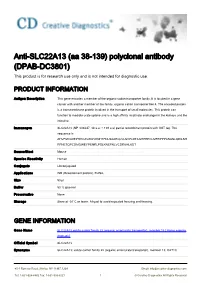
Anti-SLC22A13 (Aa 38-139) Polyclonal Antibody (DPAB-DC3801) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-SLC22A13 (aa 38-139) polyclonal antibody (DPAB-DC3801) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description This gene encodes a member of the organic-cation transporter family. It is located in a gene cluster with another member of the family, organic cation transporter like 4. The encoded protein is a transmembrane protein involved in the transport of small molecules. This protein can function to mediate urate uptake and is a high affinity nicotinate exchanger in the kidneys and the intestine. Immunogen SLC22A13 (NP_004247, 38 a.a. ~ 139 a.a) partial recombinant protein with GST tag. The sequence is AHVFMVLDEPHHCAVAWVKNHTFNLSAAEQLVLSVPLDTAGHPEPCLMFRPPPANASLQDILSH RFNETQPCDMGWEYPENRLPSLKNEFNLVCDRKHLKDT Source/Host Mouse Species Reactivity Human Conjugate Unconjugated Applications WB (Recombinant protein), ELISA, Size 50 μl Buffer 50 % glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name SLC22A13 solute carrier family 22 (organic anion/urate transporter), member 13 [ Homo sapiens (human) ] Official Symbol SLC22A13 Synonyms SLC22A13; solute carrier family 22 (organic anion/urate transporter), member 13; OAT10; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved OCTL1; OCTL3; ORCTL3; ORCTL-3; solute carrier family 22 member 13; organic cation transporter-like 3; organic-cation transporter like 3; organic cationic transporter-like 3; solute carrier family 22, member 13; solute carrier family 22 (organic anion transporter), member 13; Entrez Gene ID 9390 Protein Refseq NP_004247 UniProt ID Q9Y226 Chromosome Location 3p21.3 Function nicotinate transporter activity; organic cation transmembrane transporter activity; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 2 © Creative Diagnostics All Rights Reserved. -

Expression of SLC2A9 Isoforms in the Kidney and Their Localization in Polarized Epithelial Cells
Expression of SLC2A9 Isoforms in the Kidney and Their Localization in Polarized Epithelial Cells Toru Kimura1, Michi Takahashi1, Kunimasa Yan2, Hiroyuki Sakurai1* 1 Department of Pharmacology and Toxicology, Kyorin University School of Medicine, Mitaka, Tokyo, Japan, 2 Department of Pediatrics, Kyorin University School of Medicine, Mitaka, Tokyo, Japan Abstract Background: Many genome-wide association studies pointed out that SLC2A9 gene, which encodes a voltage-driven urate transporter, SLC2A9/GLUT9 (a.k.a. URATv1), as one of the most influential genes for serum urate levels. SLC2A9 is reported to encode two splice variants: SLC2A9-S (512 amino acids) and SLC2A9-L (540 amino acids), only difference being at their N- termini. We investigated isoform-specific localization of SLC2A9 in the human kidney and role of N-terminal amino acids in differential sorting in vitro. Methodology/Principal Findings: Isoform specific antibodies against SLC2A9 were developed and human kidney sections were stained. SLC2A9-S was expressed in the apical side of the collecting duct while SLC2A9-L was expressed in the basolateral side of the proximal tubule. GFP fused SLC2A9s were expressed in MDCK cells and intracellular localization was observed. SLC2A9-S was expressed at both apical and basolateral membranes, whereas SLC2A9-L was expressed only at the basolateral membrane. Although SLC2A9-L has a putative di-leucine motif at 33th and 34th leucine, deletion of the motif or replacement of leucine did not affect its subcellular localization. When up to 16 amino acids were removed from the N- terminal of SLC2A9-S or when up to 25 amino acids were removed from the N-terminal of SLC2A9-L, there was no change in their sorting. -

Cellular and Molecular Signatures in the Disease Tissue of Early
Cellular and Molecular Signatures in the Disease Tissue of Early Rheumatoid Arthritis Stratify Clinical Response to csDMARD-Therapy and Predict Radiographic Progression Frances Humby1,* Myles Lewis1,* Nandhini Ramamoorthi2, Jason Hackney3, Michael Barnes1, Michele Bombardieri1, Francesca Setiadi2, Stephen Kelly1, Fabiola Bene1, Maria di Cicco1, Sudeh Riahi1, Vidalba Rocher-Ros1, Nora Ng1, Ilias Lazorou1, Rebecca E. Hands1, Desiree van der Heijde4, Robert Landewé5, Annette van der Helm-van Mil4, Alberto Cauli6, Iain B. McInnes7, Christopher D. Buckley8, Ernest Choy9, Peter Taylor10, Michael J. Townsend2 & Costantino Pitzalis1 1Centre for Experimental Medicine and Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK. Departments of 2Biomarker Discovery OMNI, 3Bioinformatics and Computational Biology, Genentech Research and Early Development, South San Francisco, California 94080 USA 4Department of Rheumatology, Leiden University Medical Center, The Netherlands 5Department of Clinical Immunology & Rheumatology, Amsterdam Rheumatology & Immunology Center, Amsterdam, The Netherlands 6Rheumatology Unit, Department of Medical Sciences, Policlinico of the University of Cagliari, Cagliari, Italy 7Institute of Infection, Immunity and Inflammation, University of Glasgow, Glasgow G12 8TA, UK 8Rheumatology Research Group, Institute of Inflammation and Ageing (IIA), University of Birmingham, Birmingham B15 2WB, UK 9Institute of -

2.1 Drosophila Melanogaster
Overend, Gayle (2010) Drosophila as a model for the Anopheles Malpighian tubule. PhD thesis, University of Glasgow. http://theses.gla.ac.uk/1604/ Copyright and moral rights for this thesis are retained by the author A copy can be downloaded for personal non-commercial research or study, without prior permission or charge This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the Author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the Author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Glasgow Theses Service http://theses.gla.ac.uk/ [email protected] Drosophila as a model for the Anopheles Malpighian tubule A thesis submitted for the degree of Doctor of Philosophy at the University of Glasgow Gayle Overend Integrative and Systems Biology Faculty of Biomedical and Life Sciences University of Glasgow Glasgow G11 6NU UK August 2009 2 The research reported within this thesis is my own work except where otherwise stated, and has not been submitted for any other degree. Gayle Overend 3 Abstract The insect Malpighian tubule is involved in osmoregulation, detoxification and immune function, physiological processes which are essential for insect development and survival. As the Malpighian tubules contain many ion channels and transporters, they could be an effective tissue for targeting with novel pesticides to control populations of Diptera. Many of the insecticide compounds used to control insect pest species are no longer suited to their task, and so new means of control must be found. -

Distribution of Glucose Transporters in Renal Diseases Leszek Szablewski
Szablewski Journal of Biomedical Science (2017) 24:64 DOI 10.1186/s12929-017-0371-7 REVIEW Open Access Distribution of glucose transporters in renal diseases Leszek Szablewski Abstract Kidneys play an important role in glucose homeostasis. Renal gluconeogenesis prevents hypoglycemia by releasing glucose into the blood stream. Glucose homeostasis is also due, in part, to reabsorption and excretion of hexose in the kidney. Lipid bilayer of plasma membrane is impermeable for glucose, which is hydrophilic and soluble in water. Therefore, transport of glucose across the plasma membrane depends on carrier proteins expressed in the plasma membrane. In humans, there are three families of glucose transporters: GLUT proteins, sodium-dependent glucose transporters (SGLTs) and SWEET. In kidney, only GLUTs and SGLTs protein are expressed. Mutations within genes that code these proteins lead to different renal disorders and diseases. However, diseases, not only renal, such as diabetes, may damage expression and function of renal glucose transporters. Keywords: Kidney, GLUT proteins, SGLT proteins, Diabetes, Familial renal glucosuria, Fanconi-Bickel syndrome, Renal cancers Background Because glucose is hydrophilic and soluble in water, lipid Maintenance of glucose homeostasis prevents pathological bilayer of plasma membrane is impermeable for it. There- consequences due to prolonged hyperglycemia or fore, transport of glucose into cells depends on carrier pro- hypoglycemia. Hyperglycemia leads to a high risk of vascu- teins that are present in the plasma membrane. In humans, lar complications, nephropathy, neuropathy and retinop- there are three families of glucose transporters: GLUT pro- athy. Hypoglycemia may damage the central nervous teins, encoded by SLC2 genes; sodium-dependent glucose system and lead to a higher risk of death. -

Dopaminergic Loss of Cyclin-Dependent Kinase-Like 5 Recapitulates Methylphenidate-Remediable Hyperlocomotion in Mouse Model of CDKL5 Deficiency Disorder
Dopaminergic loss of cyclin-dependent kinase-like 5 recapitulates methylphenidate-remediable hyperlocomotion in mouse model of CDKL5 deficiency disorder Downloaded from https://academic.oup.com/hmg/article-abstract/doi/10.1093/hmg/ddaa122/5863032 by University of Exeter user on 26 June 2020 Cian-Ling Jhang1, Hom-Yi Lee3,4, Jinchung Chen5, Wenlin Liao1,2 * 1 Institute of Neuroscience, 2 Research Center for Mind, Brain and Learning, National Cheng-Chi University, Taipei 116, Taiwan 3 Department of Psychology, 4 Department of Speech Language Pathology and Audiology, Chung Shan Medical University, Taichung 402, Taiwan 5 Graduate Institute of Biomedical Sciences, Chang Gung University, Taoyuan 333, Taiwan UNCORRECTED MANUSCRIPT © The Author(s) 2020. Published by Oxford University Press. All rights reserved. For Permissions, please email: [email protected] page 1 Downloaded from https://academic.oup.com/hmg/article-abstract/doi/10.1093/hmg/ddaa122/5863032 by University of Exeter user on 26 June 2020 * To whom correspondence should be addressed: Wenlin Liao, PhD Associate Professor Institute of Neuroscience, National Cheng-Chi University 64, Sec. 2, Chi-Nan Road, Wen-Shan District Taipei 116, Taiwan Phone: 886-2-29393091 ext. 89621 UNCORRECTEDEmail: [email protected] MANUSCRIPT page 2 ABSTRACT Cyclin-dependent kinase-like 5 (CDKL5), a serine-threonine kinase encoded by an X-linked gene, is highly expressed in mammalian forebrain. Mutations in this gene Downloaded from https://academic.oup.com/hmg/article-abstract/doi/10.1093/hmg/ddaa122/5863032 by University of Exeter user on 26 June 2020 cause CDKL5 deficiency disorder, a neurodevelopmental encephalopathy characterized by early-onset seizures, motor dysfunction and intellectual disability. -

The Hearing Gene Prestin Reunites Echolocating Bats
The hearing gene Prestin reunites echolocating bats Gang Li*, Jinhong Wang*, Stephen J. Rossiter†‡, Gareth Jones§, James A. Cotton†, and Shuyi Zhang*‡ *School of Life Science, East China Normal University, Shanghai 200062, China; †School of Biological and Chemical Sciences, Queen Mary, University of London, London E1 4NS, United Kingdom; and §School of Biological Sciences, University of Bristol, Bristol BS8 1UG, United Kingdom Edited by Morris Goodman, Wayne State University School of Medicine, Detroit, MI, and approved July 10, 2008 (received for review March 4, 2008) The remarkable high-frequency sensitivity and selectivity of the Among all mammals, sensitivity to the highest frequencies occurs mammalian auditory system has been attributed to the evolution of in echolocating cetaceans and bats (17), which use sound for mechanical amplification, in which sound waves are amplified by orientation and often for the detection, localization, and classifi- outer hair cells in the cochlea. This process is driven by the recently cation of prey (18, 19). The processing of echolocation signals discovered protein prestin, encoded by the gene Prestin. Echolocating begins at the hair cells in the organ of Corti, continues along the bats use ultrasound for orientation and hunting and possess the auditory nerve, and terminates in the auditory cortex in the brain highest frequency hearing of all mammals. To test for the involve- (1). Prestin seems to be of major importance for hearing high ment of Prestin in the evolution of bat echolocation, we sequenced frequencies and for selective hearing, and both of these processes the coding region in echolocating and nonecholocating species. The are vital for echolocation. -

Comparative Molecular Dynamics Investigation of the Electromotile Hearing Protein Prestin
International Journal of Molecular Sciences Article Comparative Molecular Dynamics Investigation of the Electromotile Hearing Protein Prestin Gianfranco Abrusci 1,2,†, Thomas Tarenzi 1,3,†, Mattia Sturlese 4 , Gabriele Giachin 5 and Roberto Battistutta 5 and Gianluca Lattanzi 1,3,∗ 1 Department of Physics, University of Trento, Via Sommarive 14, 38123 Trento, Italy; [email protected] (G.A.); [email protected] (T.T.) 2 Cineca, Via Magnanelli 6/3, Casalecchio di Reno, 40033 Bologna, Italy 3 TIFPA-INFN, Via Sommarive 14, 38123 Trento, Italy 4 Department of Pharmaceutical and Pharmacological Sciences, University of Padova, Via Marzolo 5, 35131 Padova, Italy; [email protected] 5 Department of Chemical Sciences, University of Padova, Via Marzolo 1, 35131 Padova, Italy; [email protected] (G.G.); [email protected] (R.B.) * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: The mammalian protein prestin is expressed in the lateral membrane wall of the cochlear hair outer cells and is responsible for the electromotile response of the basolateral membrane, following hyperpolarisation or depolarisation of the cells. Its impairment marks the onset of severe diseases, like non-syndromic deafness. Several studies have pointed out possible key roles of residues located in the Transmembrane Domain (TMD) that differentiate mammalian prestins as incomplete transporters from the other proteins belonging to the same solute-carrier (SLC) superfamily, which Citation: Abrusci, G.; Tarenzi, T.; are classified as complete transporters. Here, we exploit the homology of a prototypical incomplete Sturlese, M.; Giachin, G.; Battistutta, transporter (rat prestin, rPres) and a complete transporter (zebrafish prestin, zPres) with target R.; Lattanzi, G. -

1 Integrative Omics Analyses Reveal Epigenetic Memory in Diabetic Renal
Page 1 of 53 Diabetes Integrative Omics analyses reveal epigenetic memory in diabetic renal cells regulating genes associated with kidney dysfunction. Anita Bansal1, Sreeram Balasubramanian2, Sangeeta Dhawan3, Amy Leung1, Zhen Chen1, Rama Natarajan*1. 1Department of Diabetes Complications and Metabolism, Diabetes and Metabolism Research Institute, Beckman Research Institute of City of Hope, 1500 East Duarte Road, Duarte, CA 91010, 2 Division of Biology and Biological Engineering, California Institute of Technology, 1200 E California Blvd, Pasadena, CA 91125, 3Department of Translational Research and Cellular Therapeutics, Diabetes and Metabolism Research Institute, Beckman Research Institute of City of Hope, 1500 East Duarte Road, Duarte, CA 91010. Correspondence to * Rama Natarajan. Email: [email protected] 626-218-2289 Keywords Diabetic kidney disease, tubular epithelial cells, metabolic memory, epigenomics Running title: Epigenetic memory in diabetic renal tubular cells Word count: 4949 Number of Figures: 6 1 Diabetes Publish Ahead of Print, published online August 3, 2020 Diabetes Page 2 of 53 Abstract Diabetic kidney disease (DKD) is a major complication of diabetes and the leading cause of end- stage renal failure. Epigenetics has been associated with metabolic memory, in which prior periods of hyperglycemia enhance the future risk of developing DKD despite subsequent glycemic control. To understand the mechanistic role of such epigenetic memory in human DKD and identify new therapeutic targets, we profiled gene expression, DNA methylation, and chromatin accessibility in kidney proximal tubule epithelial cells (PTECs) derived from non-diabetic and Type-2 diabetic (T2D) subjects. T2D-PTECs displayed persistent gene expression and epigenetic changes with and without TGFβ1 treatment, even after culturing in vitro under similar conditions as non-diabetic PTECs, signified by deregulation of fibrotic and transport associated genes (TAGs).