Can Copper Products and Surfaces Reduce the Spread of Infectious Microorganisms and Hospital-Acquired Infections?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effectiveness of Surface Coatings Containing Silver Ions in Bacterial Decontamination in a Recovery Unit Rafael Manuel Ortí-Lucas1,2* and Julio Muñoz-Miguel1,2
Ortí-Lucas and Muñoz-Miguel Antimicrobial Resistance and Infection Control (2017) 6:61 DOI 10.1186/s13756-017-0217-9 RESEARCH Open Access Effectiveness of surface coatings containing silver ions in bacterial decontamination in a recovery unit Rafael Manuel Ortí-Lucas1,2* and Julio Muñoz-Miguel1,2 Abstract Background: HAIs remain a frequent complication for hospitalised patients and pose a challenge that must be tackled by our health systems. Methods: Quasi-experimental study. In order to determine the antimicrobial effectiveness of surface coating agents containing silver ions (BactiBlock®) the degree of contamination of several surfaces in two ICU wards was compared. The association between application of Bactiblock® and surface contamination was analysed using a relative risk (RR). Multivariate logistic regressions were performed for each product applied and each sampling location to adjust for the RR of the contamination of surfaces treated with Bactiblock® for the independent variables. Results: Surface contamination was observed in 31.5% of treated samples and 27.4 of untreated samples. Contamination was equally prominent on bedside Tables (38.7%), bed rails (38.4%) and sinks (38.3%), while the walls showed minimum contamination (2.6%). For beds under isolation protocols, contamination was higher (32.6%) than when no protocol was followed (26.5%) but the difference was not significant (p = 0.148). After stratification for application method and adjusting the multivariate models for period of the study and presence of isolated patients, the risk of contamination after the intervention increased when the coating agent was applied using a spray (OR = 1. 79; 95% CI: 1.08-2.95, particularly in a dry and rugged surface such as that of bedside Tables (OR = 2.59; 95% CI: 1.22-5. -

Impact of a Novel Antimicrobial Surface Coating
HeadB/HeadA=HeadC=HeadB/HeadA=HeadC/HeadB Clinical Infectious Diseases HeadC/HeadB=HeadD=HeadC/HeadB=HeadC/HeadB HeadC=NList_dot_numeric1=HeadC=NList_dot_numeric MAJOR ARTICLE HeadC/HeadB=NList_dot_numeric1=HeadC/HeadB=NList_dot_numeric HeadD=NList_dot_numeric1=HeadD=NList_dot_numeric HeadD/HeadC=NList_dot_numeric1=HeadD/HeadC=NList_dot_numeric Impact of a Novel Antimicrobial Surface Coating on SubBList2=NList_dot_numeric2=SubBList=NList_dot_numeric2 SubBList2=NList_dot_numeric=SubBList=NList_dot_numeric Health Care–Associated Infections and Environmental NList_dot_numeric2=HeadB=NList_dot_numeric=HeadB NList_dot_numeric3=HeadB=NList_dot_numeric=HeadB Bioburden at 2 Urban Hospitals Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciz1077/5610270 by guest on 27 January 2020 NList_dot_numeric2=SubBList1=NList_dot_numeric=SubBList1 Katherine D. Ellingson,1 Kristen Pogreba-Brown,1 Charles P. Gerba,2 and Sean P. Elliott3 1Department of Epidemiology and Biostatistics, The University of Arizona College of Public Health, Tucson, Arizona, USA, 2Department of Soil, Water, and Environmental Science, The University of NList_dot_numeric3=SubBList1=NList_dot_numeric=SubBList1 Arizona, Tucson, Arizona, USA, and 3The University of Arizona College of Medicine, Tucson, Arizona, USA SubBList3=HeadD=SubBList_Before_Head=HeadD SubBList2=HeadD=SubBList_Before_Head=HeadD Background. Approximately 1 in 25 people admitted to a hospital in the United States will suffer a health care–associated in- SubBList2=HeadB=SubBList=HeadB -
Antimicrobial Surface Protection
We have the solution. 24/7 Antimicrobial Surface Protection A cleaned surface only stays Effective Against clean until it is touched. We have the solution. BACTERIA Pseudomonas aeruginosa Protects surfaces with an antimicrobial shield that lasts Staphylococcus aureus between cleanings. Salmonella enterica Listeria monocytogenens Monofoil is a patented, EPA-approved, non-toxic antimicrobial which employs Enterococcus faecium nanotechnology to create an undetectable molecularly bonded polymer shield that provides proven sustained antimicrobial protection up to 3 months. MRSA Staphylococcus aureus Community associated MonoFoil is non-toxic, environmentally friendly, hypoallergenic and is effective in killing 70+ strains of bacteria, molds, fungi and algae. MRSA Escherichia coli Acinetobacter baumannii Campylobacter jejuni Stop Community Spread in its Klebsiella pneumoniae tracks Klebieslla Pneumonia FUNGUS Current disinfectants are only active while the surface is wet. Once dry the surface quickly becomes re- Trichophyton contaminated upon contact. mentagrophytes (Athlete’s Foot Fungus) The active ingredient in MonoFoil forms a colorless, odorless, positively charged polymer barrier. VIRUSES This barrier bonds to the application surface, where instead of being metabolized For viruses we recommend using by the microbial cells, it creates a network of electrically charged molecules on the surface which rupture the cell wall on contact, causing instant cellular death. an EPA registered virucide, for novel Coronavirus (SARS- Through this mechanism of action, microbes cannot mutate, lowering the risk of CoV-2) use a virucide appearing resistant “super-bugs” forming. on the EPA list N (www.epa.gov) Contact us for price and availability CHEM MAX CORP. 800-858-7237, www.chemmax.com. -

Brass Alloys: Copper-Bottomed Solutions Against Hospital-Acquired Infections?
antibiotics Review Brass Alloys: Copper-Bottomed Solutions against Hospital-Acquired Infections? Emilie Dauvergne 1,2 and Catherine Mullié 1,3,* 1 Laboratoire AGIR-UR UPJV 4294, UFR de Pharmacie, Université de Picardie Jules Verne, 80037 Amiens, France; [email protected] 2 FAVI Limited Company, 80490 Hallencourt, France 3 Laboratoire Hygiène, Risque Biologique et Environnement, Centre Hospitalier Universitaire Amiens-Picardie, 80025 Amiens, France * Correspondence: [email protected] Abstract: Copper has been used for its antimicrobial properties since Antiquity. Nowadays, touch surfaces made of copper-based alloys such as brasses are used in healthcare settings in an attempt to reduce the bioburden and limit environmental transmission of nosocomial pathogens. After a brief history of brass uses, the various mechanisms that are thought to be at the basis of brass antimicrobial action will be described. Evidence shows that direct contact with the surface as well as cupric and cuprous ions arising from brass surfaces are instrumental in the antimicrobial effectiveness. These copper ions can lead to oxidative stress, membrane alterations, protein malfunctions, and/or DNA damages. Laboratory studies back up a broad spectrum of activity of brass surfaces on bacteria with the possible exception of bacteria in their sporulated form. Various parameters influencing the antimicrobial activity such as relative humidity, temperature, wet/dry inoculation or wear have been identified, making it mandatory to standardize antibacterial testing. Field trials using brass and Citation: Dauvergne, E.; Mullié, C. copper surfaces consistently report reductions in the bacterial bioburden but, evidence is still sparse Brass Alloys: Copper-Bottomed as to a significant impact on hospital acquired infections. -

Registration & Product Labeling Manual
Registration & Product Labeling Manual September 2013 1│ Registration & Product Labeling Manual ◦ September 2013 OB-0012-1309 September 6, 2011 Dear CuVerro Customer, Olin Brass has prepared this Registration and Product Labeling Manual to assist companies manufacturing and marketing products made with CuVerro® bactericidal copper alloy surfaces in complying with federal and state statutes, regulations, and rules. CuVerro is the registered trademark brand of copper alloy products manufactured by GBC Metals, LLC d.b.a Olin Brass, a subsidiary of Global Brass and Copper, Inc. CuVerro copper alloys are registered with the U.S Environmental Protection Agency (U.S. EPA), allowing public health claims that CuVerro products kill bacteria1. CuVerro’s bactericidal properties are unique for solid surfaces. CuVerro is the most effective class of solid material that can claim an inherent ability to kill bacteria; and it was the first class of solid surface material to be registered with the U.S. EPA to make public health claims. Accordingly, this manual will help guide your company with U.S. EPA compliance issues as you manufacture and market products made from CuVerro alloys.2 As you review the prepared information, please consider the following: The U.S. EPA mandates adherence to these requirements in order to make public health claims associated with CuVerro alloys. The information in this manual is provided as a supplement to the complete product labeling and registration requirements found at www.epa.gov. Among the benefits of being a registered CuVerro alloy customer are the breadth of product offerings from alloys and forms (including sheet, strip, tube, castable ingot) to the umbrella U.S. -

Galleria Mellonella As a Model to Study the Effect of Antimicrobial Surfaces on Contamination by Staphylococcus Aureus
Arch Clin Biomed Res 2019; 3 (5): 315-325 DOI:10.26502/acbr.50170076 Research Article Galleria mellonella as a Model to Study the Effect of Antimicrobial Surfaces on Contamination by Staphylococcus aureus Astrid Mayr1,2, Dorothea Orth-Höller1*, Holger Heinrich3, Guido Hinterberger1, Isabella Wille1,2, Verena Naschberger1, Cornelia Lass-Flörl1,2, Ulrike Binder1 1Department of Hygiene, Microbiology and Social Medicine, Division of Hygiene and Medical Microbiology, Medical University of Innsbruck, Innsbruck, Schoepfstr. 41, 6020 Innsbruck, Austria 2Christian Doppler Laboratory for Invasive Fungal Infections (Module 3 – self disinfecting surfaces), Austria 3EGGER Holzwerkstoffe Wismar GmbH & Co. KG, Am Haffeld 1, 23970 Wismar, Germany. * Corresponding author Abstract Objective: The role of the inanimate environment in the transmission of Dorothea. Orth-Höller, Department healthcare-associated infections (HCAIs) is increasingly recognized. of Hygiene, Microbiology and Hence, several self-disinfecting surfaces have gained attention as new Social Medicine, Division of infection control strategies. The objective of this study was to assess the Hygiene and Medical antimicrobial efficacy of membrane-active polycation (maPK) surfaces Microbiology, Medical University against Staphylococcus aureus (S. aureus) applying the in vivo Galleria of Innsbruck, Innsbruck, mellonella (G. mellonella) contamination model. Schoepfstr. 41, 6020 Innsbruck, Austria, Tel: +43 512 9003 70772; Methods: In the first set-up maPK surfaces were contaminated with S. aureus and G. mellonella larvae were placed on the surface for 45 min. In E-mail: dorothea.orth@i- the second set- up larvae were contaminated with S. aureus and med.ac.at transferred to maPK surfaces. Finally, the cross-over rates to larvae and Received: 23 August 2019; maPK-surface were determined. -

Reduction of Health Care-Associated Infections (Hais) with Antimicrobial Inorganic Nanoparticles Incorporated in Medical Textiles: an Economic Assessment
nanomaterials Article Reduction of Health Care-Associated Infections (HAIs) with Antimicrobial Inorganic Nanoparticles Incorporated in Medical Textiles: An Economic Assessment Finbarr Murphy 1,2,* , Anat Tchetchik 3 and Irini Furxhi 1,2 1 Transgero Limited, Naomh Treasa, Cullinagh, Newcastle West, Co., V42 V384 Limerick, Ireland; [email protected] 2 Kemmy Business School, University of Limerick, V94 PH93 Limerick, Ireland 3 Department of Geography and Environment, Bar-Ilan University, 5290002 Ramat-Gan, Israel; [email protected] * Correspondence: fi[email protected]; Tel.: +353-61-202-181 Received: 19 April 2020; Accepted: 21 May 2020; Published: 23 May 2020 Abstract: Health care-associated infections (HAIs) affect millions of patients annually with up to 80,000 affected in Europe on any given day. This represents a significant societal and economic burden. Staff training, hand hygiene, patient identification and isolation and controlled antibiotic use are some of the standard ways to reduce HAI incidence but this is time consuming and subject and subject to rigorous implementation. In addition, the lack of antimicrobial activity of some disinfectants against healthcare-associated pathogens may also affect the efficacy of disinfection practices. Textiles are an attractive substrate for pathogens because of contact with the human body with the attendant warmth and moisture. Textiles and surfaces coated with engineered nanomaterials (ENMs) have shown considerable promise in reducing the microbial burden on those surfaces. Studies have also shown that this antimicrobial affect can reduce the incidence of HAIs. For all of the promising research, there has been an absence of study on the economic effectiveness of ENM coated materials in a healthcare setting. -
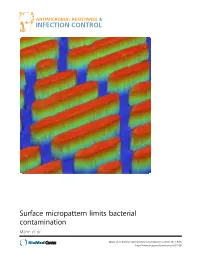
Surface Micropattern Limits Bacterial Contamination Mann Et Al
Surface micropattern limits bacterial contamination Mann et al. Mann et al. Antimicrobial Resistance and Infection Control 2014, 3:28 http://www.aricjournal.com/content/3/1/28 Mann et al. Antimicrobial Resistance and Infection Control 2014, 3:28 http://www.aricjournal.com/content/3/1/28 RESEARCH Open Access Surface micropattern limits bacterial contamination Ethan E Mann1, Dipankar Manna1, Michael R Mettetal1, Rhea M May1, Elisa M Dannemiller1, Kenneth K Chung1, Anthony B Brennan2 and Shravanthi T Reddy1* Abstract Background: Bacterial surface contamination contributes to transmission of nosocomial infections. Chemical cleansers used to control surface contamination are often toxic and incorrectly implemented. Additional non-toxic strategies should be combined with regular cleanings to mitigate risks of human error and further decrease rates of nosocomial infections. The Sharklet micropattern (MP), inspired by shark skin, is an effective tool for reducing bacterial load on surfaces without toxic additives. The studies presented here were carried out to investigate the MP surfaces capability to reduce colonization of methicillin-sensitive Staphylococcus aureus (MSSA) and methicillin-resistant S. aureus (MRSA) compared to smooth control surfaces. Methods: The MP and smooth surfaces produced in acrylic film were compared for remaining bacterial contamination and colonization following inoculation. Direct sampling of surfaces was carried out after inoculation by immersion, spray, and/or touch methods. Ultimately, a combination assay was developed to assess bacterial contamination after touch transfer inoculation combined with drying (persistence) to mimic common environmental contamination scenarios in the clinic or hospital environment. The combination transfer and persistence assay was then used to test antimicrobial copper beside the MP for the ability to reduce MSSA and MRSA challenge. -

A Light-Activated Antimicrobial Surface Is Active Against Bacterial
www.nature.com/scientificreports OPEN A Light-Activated Antimicrobial Surface Is Active Against Bacterial, Viral and Fungal Organisms Received: 11 May 2016 Tim Walker1, Melisa Canales1, Sacha Noimark2, Kristopher Page2, Ivan Parkin2, Jane Faull3, Accepted: 26 October 2017 Manni Bhatti1 & Lena Ciric1 Published: xx xx xxxx Evidence has shown that environmental surfaces play an important role in the transmission of nosocomial pathogens. Deploying antimicrobial surfaces in hospital wards could reduce the role environmental surfaces play as reservoirs for pathogens. Herein we show a signifcant reduction in viable counts of Staphylococcus epidermidis, Saccharomyces cerevisiae, and MS2 Bacteriophage after light treatment of a medical grade silicone incorporating crystal violet, methylene blue and 2 nm gold nanoparticles. Furthermore, a migration assay demonstrated that in the presence of light, growth of the fungus-like organism Pythium ultimum and the flamentous fungus Botrytis cinerea was inhibited. Atomic Force Microscopy showed signifcant alterations to the surface of S. epidermidis, and electron microscopy showed cellular aggregates connected by discrete surface linkages. We have therefore demonstrated that the embedded surface has a broad antimicrobial activity under white light and that the surface treatment causes bacterial envelope damage and cell aggregation. Infections originating in hospitals (nosocomial infections, or healthcare associated infections) are a major prob- lem in modern healthcare. A 2011 survey found the prevalence of nosocomial infections in Scotland to be 4.6%1. Up until the last decade, it was believed that contamination of environmental surfaces played a minimal role in transmission of nosocomial infections and eforts to control transmission focused on efective hand hygiene of healthcare workers2. -

Antimicrobial Evaluation of a Surface Protector System
Duong (2016) Antimicrobial Evaluation of a Surface Protector System Andrew Duong Edited by: Michael Diamond Reviewed by: Dr. Uyen Nguyen Disclaimer: The authors of this report and InfectionControl.tips declare no conflict of interest with the following critical evaluation and research. No funds or influence were provided to the authors or InfectionControl.tips by any parties. Abstract: The spread of hospital acquired infections has been spurned by the overuse of antibiotics and the challenges of hospital cleaning. In this study, the effectiveness of an antimicrobial surface protector was evaluated. Following exposure to the Clean2Touch surface protector, it was shown that the protector was effective in reducing the growth of Staphylococcus aureus,Clostridium difficile, Escherichia coli, and methicillin-resistant S. aureus.After 2 h of incubation on the surface, there was a significant reduction in the number of viable microorganisms. Interestingly, the experiments demonstrated that a large majority of bacteria were killed instantaneously upon exposure to the antimicrobial film. Introduction: hospital visit [3]. In The World Health Organization has immunocompromised patients, this published numerous documents on presents a serious and sometimes the rising threat of antimicrobial lethal threat. resistance and its impact on the future global health [5]. Much of this Hospitals use a variety of detergents resistance is driven by the and cleansers to clean rooms in widespread and irresponsible use of between patients. However, it antibiotics to treat patients when they requires vigilant employees to do not have a bacterial infection. The ensure that the standard operating overuse of antibiotics resulted in the procedures are followed and regular development and subsequent spread maintenance to remain effective in of drug-resistant, and more minimizing the bacterial population dangerously, multi-drug resistant (bioburden) [3,9]. -

Fast Disinfecting Antimicrobial Surfaces
1060 Langmuir 2009, 25, 1060-1067 Fast Disinfecting Antimicrobial Surfaces Ahmad E. Madkour,† Jeffery M. Dabkowski,†,‡ Klaus Nu¨sslein,‡ and Gregory N. Tew*,† Department of Polymer Science & Engineering and Department of Microbiology, UniVersity of Massachusetts, Amherst, Massachusetts 01003 ReceiVed September 8, 2008. ReVised Manuscript ReceiVed October 30, 2008 Silicon wafers and glass surfaces were functionalized with facially amphiphilic antimicrobial copolymers using the “grafting from” technique. Surface-initiated atom transfer radical polymerization (ATRP) was used to grow poly(butylmethacrylate)-co-poly(Boc-aminoethyl methacrylate) from the surfaces. Upon Boc-deprotection, these surfaces became highly antimicrobial and killed S. aureus and E. coli 100% in less than 5 min. The molecular weight and grafting density of the polymer were controlled by varying the polymerization time and initiator surface density. Antimicrobial studies showed that the killing efficiency of these surfaces was independent of polymer layer thickness or grafting density within the range of surfaces studied. Introduction were successfully applied as antimicrobial layers over glass14 15 Hospital-acquired infections pose a major global healthcare and poly(ethylene terephthalate) surfaces. Polymers containing issue. Over 2 million cases are reported annually in the USA QACs have been previously covalently attached onto different materials such as glass,14,16-19 polymers,20,21 paper,19 and alone, leading to 100 000 deaths and adding nearly 5 billion 22 dollars to U.S. healthcare costs.1,2 Contamination of medical metals. devices (catheters, implants, etc.) is responsible for 45% of these The killing mechanism of bacteria by those surfaces, and infections.3 Sources of infectious bacteria can be traced to surgical especially the effect of polymer length on killing efficiency, is equipment, medical staff clothing, resident bacteria on the patient’s still under debate. -
Antimicrobial Surface Protection
PreventX 24/7™ Bacteriostatic Update Connecting Historical Dots Antimicrobial Surface Protection Typical disinfectants kill viruses and bacteria within 10 minutes, but once the product dries, there's no further protection. The cleaned surface is now ready to be re-contaminated. Imagine someone wiping and disinfecting a surface every time new microorganisms contaminate it or spread further. PreventX 24/7™ is not a replacement for existing disinfecting protocols but serves as the secondary level of defense against microorganisms, bacteria, mold, and mildew. Our unique coating technology is an EPA approved bacteriostatic (EPA Reg #91116-1) as it kills without poison and will not leach off treated surfaces or create superbugs. The first and foremost thing to remember about PreventX 24/7™ is that by treating a surface, HealthCare Synergy in no way is making a public health claim. The EPA has not yet approved any registered antimcrobial for viral claims. PreventX 24/7™ is an EPA registered antimicrobial, allowing for durable bacteriostatic, fungistatic, and algaestatic surface protection. Highlighted benefits are: Environmentally Friendly Non-Toxic, non-poisonous microscopic electrostatically held on the surface "needles" puncture organisms using a physical kill, not a chemical kill, also means no superbugs. Protective Barrier The protective barrier reduces cross-contamination on high touch and at-risk surfaces. Prevents Mold, Mildew, and other Microorganisms Growth on Surfaces Biofilm cannot exist on a PreventX 24/7™ treated surfaces; therefore, mold, mildew, and other microorganisms cannot thrive. Long Lasting PreventX 24/7™ provides a protective surface that is not destroyed by daily cleaning and lasts up to 90 days, depending on surface abrasion/use, with each simple application.