NOVEMBER 15, 2006 University of Chicago (Map Attached) Enter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tinea Versicolor Mimicking Pityriasis Rubra Pilaris
Tinea Versicolor Mimicking Pityriasis Rubra Pilaris Capt Matthew J. Darling, MC, USAF; CPT Matthew C. Lambiase, MC, USA; Capt R. John Young, MC, USAF Tinea versicolor is a common noninvasive cuta- neous fungal disease. We recount a case of tinea versicolor that mimicked type I (classic adult) pityriasis rubra pilaris. A 54-year-old white man reported a 20-year history of a recurrent pruritic eruption that had marginally improved with use of selenium sulfide shampoo and treatment with oral antihistamines. Results of a skin examination revealed erythematous plaques; islands of spared skin; and follicular erythematous keratotic papules on the trunk, shoulders, and upper arms. A lesion was scraped to obtain skin scales for potassium hydroxide staining. Examination of the stained samples revealed the characteristic “spaghetti and meatballs,” confirming the diagnosis. Cutis. 2005;75:265-267. Case Report A 54-year-old white man presented with a 20-year history of a recurrent pruritic eruption that had marginally improved with use of selenium sulfide shampoo and oral antihistamine therapy. Erythem- atous scaly plaques were noted over the trunk and extremities (Figure 1). Islands of spared skin were most notable on the trunk (Figure 2). Follicular, erythematous, keratotic papules were noted on the shoulders and upper arms (Figure 3). Results of Wood lamp examination revealed a yellow-green Figure 1. Erythematous scaly plaques and islands of fluorescence of the plaques. Results of potassium spared skin on the chest. hydroxide (KOH) staining revealed numerous yeast and hyphae. The patient was diagnosed with tinea versicolor and treated with itraconazole 200 mg/d for 2 weeks. -

Clinical Features of Benign Tumors of the External Auditory Canal According to Pathology
Central Annals of Otolaryngology and Rhinology Research Article *Corresponding author Jae-Jun Song, Department of Otorhinolaryngology – Head and Neck Surgery, Korea University College of Clinical Features of Benign Medicine, 148 Gurodong-ro, Guro-gu, Seoul, 152-703, South Korea, Tel: 82-2-2626-3191; Fax: 82-2-868-0475; Tumors of the External Auditory Email: Submitted: 31 March 2017 Accepted: 20 April 2017 Canal According to Pathology Published: 21 April 2017 ISSN: 2379-948X Jeong-Rok Kim, HwibinIm, Sung Won Chae, and Jae-Jun Song* Copyright Department of Otorhinolaryngology-Head and Neck Surgery, Korea University College © 2017 Song et al. of Medicine, South Korea OPEN ACCESS Abstract Keywords Background and Objectives: Benign tumors of the external auditory canal (EAC) • External auditory canal are rare among head and neck tumors. The aim of this study was to analyze the clinical • Benign tumor features of patients who underwent surgery for an EAC mass confirmed as a benign • Surgical excision lesion. • Recurrence • Infection Methods: This retrospective study involved 53 patients with external auditory tumors who received surgical treatment at Korea University, Guro Hospital. Medical records and evaluations over a 10-year period were examined for clinical characteristics and pathologic diagnoses. Results: The most common pathologic diagnoses were nevus (40%), osteoma (13%), and cholesteatoma (13%). Among the five pathologic subgroups based on the origin organ of the tumor, the most prevalent pathologic subgroup was the skin lesion (47%), followed by the epithelial lesion (26%), and the bony lesion (13%). No significant differences were found in recurrence rate, recurrence duration, sex, or affected side between pathologic diagnoses. -

Bone and Soft Tissue Tumors Have Been Treated Separately
EPIDEMIOLOGY z Sarcomas are rare tumors compared to other BONE AND SOFT malignancies: 8,700 new sarcomas in 2001, with TISSUE TUMORS 4,400 deaths. z The incidence of sarcomas is around 3-4/100,000. z Slight male predominance (with some subtypes more common in women). z Majority of soft tissue tumors affect older adults, but important sub-groups occur predominantly or exclusively in children. z Incidence of benign soft tissue tumors not known, but Fabrizio Remotti MD probably outnumber malignant tumors 100:1. BONE AND SOFT TISSUE SOFT TISSUE TUMORS TUMORS z Traditionally bone and soft tissue tumors have been treated separately. z This separation will be maintained in the following presentation. z Soft tissue sarcomas will be treated first and the sarcomas of bone will follow. Nowhere in the picture….. DEFINITION Histological z Soft tissue pathology deals with tumors of the classification connective tissues. of soft tissue z The concept of soft tissue is understood broadly to tumors include non-osseous tumors of extremities, trunk wall, retroperitoneum and mediastinum, and head & neck. z Excluded (with a few exceptions) are organ specific tumors. 1 Histological ETIOLOGY classification of soft tissue tumors tumors z Oncogenic viruses introduce new genomic material in the cell, which encode for oncogenic proteins that disrupt the regulation of cellular proliferation. z Two DNA viruses have been linked to soft tissue sarcomas: – Human herpes virus 8 (HHV8) linked to Kaposi’s sarcoma – Epstein-Barr virus (EBV) linked to subtypes of leiomyosarcoma z In both instances the connection between viral infection and sarcoma is more common in immunosuppressed hosts. -

CASE REPORT Intradermal Nevus of the External Auditory Canal
Int. Adv. Otol. 2009; 5:(3) 401-403 CASE REPORT Intradermal Nevus of the External Auditory Canal: A Case Report Sedat Ozturkcan, Ali Ekber, Riza Dundar, Filiz Gulustan, Demet Etit, Huseyin Katilmis Department of Otorhinolaryngology and Head and Neck Surgery ‹zmir Atatürk Research and Training Hospital, Ministry of Health, ‹ZM‹R-TURKEY (SO, AE, FG, DE, HK) Department of Otorhinolaryngology and Head and Neck Surgery Etimesgut Military Hospital , ANKARA-TURKEY (RD) Intradermal nevus is the most common skin tumor in humans; however, its occurrence in the external auditory canal (EAC) is uncommon. The clinical manifestations of pigmented nevus of the EAC have been reported to include ear fullness, foreign body sensation, hearing impairment, and otalgia, but some cases were asymptomatic and were found incidentally. The treatment of choice for a symptomatic intradermal nevus in the EAC is complete excision. There has been no recurrence reported in the literature . A pedunculated, papillomatous hair-bearing lesion was detected in the external auditory canal of the patient who was on follow-up for pruritus. Clinical and pathologic features of an intradermal nevus of the external auditory canal are presented, and the literature reviewed. Submitted : 14 October 2008 Revised : 01 July 2009 Accepted : 09 July 2009 Intradermal nevus is the most common skin tumor in left external auditory canal. Otomicroscopic humans; however, its occurrence in the external examination revealed a pedunculated, papillomatous auditory canal (EAC) is uncommon [1-4]. Intradermal hair-bearing lesion in the postero-inferior cartilaginous nevus is considered to be a form of benign cutaneous portion of the external auditory canal (Figure 1). -

Critical Evaluation of the So-Called “Junction Nevus”
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector CRITICAL EVALUATION OF THE SO-CALLED "JUNCTION NEVUS* S. WILLIAM BECKER, MS., M.D. The serious study of pigmented nevi was undertaken by many workers in the closing years of the 19th Century. All recognized that the microscopic picture of nevi differed from anything seen in other organs. The presence of nevus cells in both the epidermis and dermis led to concepts of origin at one or the other site, or at both sites. Dermal Origin: Demieville (1) believed that the nevus cells arose from adven- titial and endothelial cells of blood vessels. Bauer (2) and vonRecklinghausen (3) thought that the origin was from endothelium of lymph vessels rather than of blood vessels. Epidermal Origin: According to Abesser (4), Duranti, in 1871, was the first to suggest an epidermal origin of nevus cells. Kromayer (5) stated that the endo- thelium-like cells originate in the basal portion of the epidermis as "Bläschen- zellen", migrate to the dermis and develop connective tissue and elastic fibers, a change which he called "desmoplasia". Abesser (4) agreed that the cells origi- ated in the epithelium and lost their intercellular bridges, but migrated into the dermis as epithelium-like cells, and remained such. Unna (6) advanced the concept that the epithelial cells changed by losing their intercellular bridges and multiplied in groups, a process which he called "Ab- sonderung", then migrated as groups to the dermis, which he called "Abtrop- fung", thus forming pigmented nevi. -
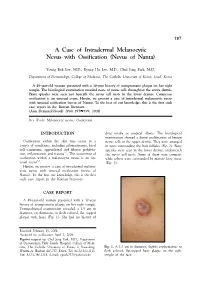
A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta)
197 A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta) Young Bok Lee, M.D., Kyung Ho Lee, M.D., Chul Jong Park, M.D. Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. The histological examination revealed nests of nevus cells throughout the entire dermis. Bony spicules were seen just beneath the nevus cell nests in the lower dermis. Cutaneous ossification is an unusual event. Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best of our knowledge, this is the first such case report in the Korean literature. (Ann Dermatol (Seoul) 20(4) 197∼199, 2008) Key Words: Melanocytic nevus, Ossification INTRODUCTION drug intake or medical illness. The histological examination showed a dense proliferation of benign Ossification within the skin may occur in a nevus cells in the upper dermis. They were arranged variety of conditions, including pilomatricoma, basal in nests surrounding the hair follicles (Fig. 2). Bony cell carcinoma, appendageal and fibrous prolifera- spicules were seen in the lower dermis, underneath 1,2 tion, inflammation and trauma . The occurrence of the nevus cell nests. Some of them were compact ossification within a melanocytic nevus is an un- while others were surrounded by mature fatty tissue 3-5 usual event . (Fig. 3). Herein, we present a case of intradermal melano- cytic nevus with unusual ossification (nevus of Nanta). To the best our knowledge, this is the first such case report in the Korean literature. -

Primary Follicular Mucinosis
International Journal of Scientific & Engineering Research Volume 8, Issue 6, June-2017 1303 ISSN 2229-5518 Case Report Primary Follicular Mucinosis: A Case Report From Saudi Arabia With Successful Treatment And Literature Review SalaimanAlsaiari1 AwadhAlAmri2 AmerAlmuqati Ibrahim Allihibi ABSTRACT: Background:Follicular mucinosis is an uncommon inflammatory disorder that characteristically presents as clearly defined, erythematous plaques or papules, with follicular projections, superficial scaling, and alopecia in terminal hair bearing areas, characterized histologically by mucin accumulation in pilosebaceous units (follicular epithelium and sebaceous glands) . The condition is generally divided into primary (idiopathic) and secondary forms in association with several conditions including benign and malignant diseases. There are many local and systemic treatments. Main observations: We report a case of 15 years old male with primary follicular mucinosis treated effectively by intralesional steroid injections. Conclusions: This is a new case of Primary follicular mucinosis from Saudi Arabia was treated successfully with intralesional corticosteroids without relapse. KEYWORDS:follicular mucinosis, intralesional corticosteroids, treatment. —————————— —————————— INTRODUCTIONIJSER Follicular mucinosis is a rare condition, of unknown cause, which affects all races, ages and both sexes.1,2It is defined as the accumulation of mucin in the follicular epithelium and sebaceous glands.3,5 It was initially described in 1957 by Pinkus who named it -

Dermatology Volume 58 Issue 2 March-April 2013 Indian Journal Of
Indian Journal of ISSN: 0019-5154 Dermatology Volume 58 Issue 2 March-April 2013 Indian Journal of Highlights of the issue Dermatology • Update on cutaneous calciphylaxis • Macrophage migration inhibitory factor in • V Dermatology olume • Fixed duration therapy in leprosy 58 • Issue • Environmental dermatoses in Ladakh • Demodex folliculorum as a risk factor in 2 • Diagnosing rosacea March-April • Annular lesions in Dermatology 2013 • Pages Clinical and photomicrograph of Mycosis fungoides, PET-CT for staging and response assessment IJD® Symposium: Integrative Dermatology 87-**** Guest Editor: S R Narahari IJD® www.e-ijd.org E‑Case Report Angiolymphoid Hyperplasia with Eosinophilia with Follicular Mucinosis Rameshwar Gutte, Bhavana Doshi, Uday Khopkar From the Department of Dermatology, Seth G. S. Medical College and King Edward Memorial Hospital, Mumbai, India Abstract Follicular mucinosis occurring along with angiolymphoid hyperplasia with eosinophils (ALHE) has been described in a 49-year-old male. The patient presented with pruritic hyperpigmented papules and nodules on the vertex and right parietal scalp. There was no any other complaint. Histopathological examination from one of the papule showed prominent blood vessels in the dermis lined by plump histiocytoid endothelial cells that were surrounded by a dense lymphoid infiltrate with numerous eosinophils; these findings are typical of angiolymphoid hyperplasia with eosinophilia. Features of follicular mucinosis were observed in the same section with 3 hyperplastic follicular infundibula containing pools of mucin in the infundibular epithelium. The concurrent occurrence of these 2 distinct histopathological patterns in the same biopsy specimen has been reported rarely. Key Words: Angiolymphoid hyperplasia, eosinophilia, follicular mucinosis, scalp What was known? perivascular area and other parts of the dermis. -

Alopecia, Particularly: Alopecia Areata Androgenetic Alopecia Telogen Effluvium Anagen Effluvium
432 Teams Dermatology Hair disorders Color Code: Original, Team’s note, Important, Doctor’s note, Not important, Old teamwork Done by: Shaikha Aldossari Reviewer: Lama AlTawil 8 Team Leader: Basil Al Suwaine&Lama Al Tawil 432 Dermatology Team Lecture 8: Hair Disorders Objectives 1- Normal anatomy of hair follicle and hair cycle. 2- Causes, features and management of non scarring alopecia, particularly: Alopecia areata Androgenetic alopecia Telogen effluvium Anagen effluvium 3- Causes and features of scarring alopecia. 4- Causes and features of Excessive hair growth. hair disorder Excessive hair Alopecia growth non scarring Hirsutism Hypertrichosis scarring Anagen Telogen Androgenetic Alopecia effluvium effluvium Alopecia Areata P a g e | 1 432 Dermatology Team Lecture 8: Hair Disorders Anatomy of hair follicle: The Arrector piliResponsible for piloerection (goose bumps ) that happens when one is cold (produces energy and therefor warmth) . hair follicle becomes vertical instead of oblique Cuticle is the last layer here . what we can see outside . it has 7 layers of keratinocytes How many hairs in the body? 5 millions hairs in the body, 100,000 in the scalp. Growth rate: 0.3mm/day for scalp hair i.e.1cm/month Hair follicle bulge: -Very important part since it has stem cells .its the inertion of the arrector pili Hair follicle on vertical section: -So any pathological process affecting any part other Initially the shaft and the follicle are one than this, hair would still be able to regrow. organ then when you reach 1/3 the follicle -If we want to destroy a hair follicle, we’d target the bulge. -

Cutaneous Manifestations of Chronic Graft-Versus-Host Disease
Biology of Blood and Marrow Transplantation 12:1101-1113 (2006) ᮊ 2006 American Society for Blood and Marrow Transplantation 1083-8791/06/1211-0001$32.00/0 doi:10.1016/j.bbmt.2006.08.043 Cutaneous Manifestations of Chronic Graft-versus-Host Disease Sharon R. Hymes,1 Maria L. Turner,3 Richard E. Champlin,2 Daniel R. Couriel2 Departments of 1Dermatology and 2Blood and Marrow Transplantation, The MD Anderson Cancer Center, Houston, Texas; 3Dermatology Branch, National Cancer Institute, Bethesda, Maryland Correspondence and reprint requests: Sharon R. Hymes, MD, Department of Dermatology, The MD Anderson Cancer Center, Unit 434, FC5.3004, Houston, TX 77030 (e-mail: [email protected]). Received August 11, 2006; accepted August 29, 2006 ABSTRACT Cutaneous chronic graft versus host disease has traditionally been classified into lichenoid and scleroderma- like forms. However, the initial presentation is sometimes subtle and a variety of less common cutaneous manifestation may be prevalent. This clinical review focuses on the lesional morphology of chronic graft versus host disease, and presents a classification system that may prove useful in early diagnosis. In addition, this approach may help to facilitate the correlation of different morphologic entities with outcome and response to therapy. © 2006 American Society for Blood and Marrow Transplantation KEY WORDS Stem cell transplant ● GVHD ● Dermatology INTRODUCTION scribe and summarize the diversity of cutaneous manifestations of cGVHD in Table 1. In our pa- Hematopoietic stem cell transplantation (HSCT) tients, the diagnosis of cutaneous GVHD was con- using peripheral blood, cord blood, or bone marrow is firmed by a combination of elements including the used to treat a wide variety of genetic and immunologic clinical course and the presence of GVHD in other disorders and hematologic and solid organ malignancies. -

Aetiological and Clinicopathological Study of Erythroderma
1 AETIOLOGICAL AND CLINICOPATHOLOGICAL STUDY OF ERYTHRODERMA Dissertation Submitted in Partial fulfillment of the University regulations for MD DEGREE IN DERMATOLOGY, VENEREOLOGY AND LEPROSY (BRANCH XII A) MADRAS MEDICAL COLLEGE THE TAMILNADU DR.M.G.R. MEDICAL UNIVERSITY CHENNAI, INDIA. APRIL 2013 2 CERTIFICATE Certified that this dissertation titled “AETIOLOGICAL AND CLINICOPATHOLOGICAL STUDY OF ERYTHRODERMA” is a bonafide work done by Dr.AARTHI M, Post graduate student of the Department of Dermatology, Venereology and Leprosy, Madras Medical College, Chennai – 3, during the academic year 2010 – 2013. This work has not previously formed the basis for the award of any degree. Prof. K.MANOHARAN MD., D.D., Head of the Department, Department of Dermatology, Madras Medical College & Rajiv Gandhi Govt. General Hospital, Chennai-3. Prof. V. KANAGASABAI, M.D., Dean Madras Medical College Chennai-600003. 3 DECLARATION I, Dr. AARTHI M solemnly declare that this dissertation titled “AETIOLOGICAL AND CLINICOPATHOLOGICAL STUDY OF ERYTHRODERMA” is a bonafide work done by me at Madras Medical College during 2010-2013 under the guidance and supervision of Prof. K.MANOHARAN, M.D., D.D., Professor and Head, Department of Dermatology, Madras Medical College, Chennai – 600 003. This dissertation is submitted to The Tamil Nadu Dr.M.G.R. Medical University, Chennai towards partial fulfillment of the rules and regulations for the award of M.D Degree in Dermatology, Venereology and Leprology (BRANCH – XII A) PLACE : DATE : (Dr. AARTHI M) 4 SPECIAL ACKNOWLEDGEMENT My sincere thanks to Prof. V.Kanagasabai, M.D., Dean, Madras Medical College for allowing me to do this dissertation and utilize the Institutional facilities. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass.