Hodgson CV Aug2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Curriculum Vitae
January 2021 Curriculum Vitae Rajiv Vohra Ford Foundation Professor of Economics Brown University Providence, RI 02912 rajiv [email protected] http://www.brown.edu/Departments/Economics/Faculty/Rajiv Vohra Education Ph.D. (Economics), 1983, Johns Hopkins University, Baltimore, Maryland. M.A. (Economics), 1981, Johns Hopkins University, Baltimore, Maryland. M.A. (Economics), 1979, Delhi School of Economics, University of Delhi, India. B.A. (Economics Hons.), 1977, St. Stephen's College, University of Delhi, India. Current Position Ford Foundation Professor of Economics, Brown University, July 2006 - Other Positions Dean of the Faculty, Brown University, July 2004 - June 2011. Professor of Economics, Brown University, July 1989 - June 2006. Morgenstern Visiting Professor of Economic Theory, New York University, Fall 2001. Fulbright Research Scholar, Indian Statistical Institute, 1995-1996. Chairman, Department of Economics, Brown University, July 1991 - June 1995. Visiting Fellow, Indian Statistical Institute, New Delhi, August 1987 - July 1988. Associate Professor of Economics, Brown University, January 1987 - June 1989. Assistant Professor of Economics, Brown University, July 1983 - December 1986. 1 Professional Activities Associate Editor, Journal of Public Economic Theory, 2017 - . Co-Organizer, 2016, NSF-CEME Decentralization Conference, Brown Uni- versity. Organizer, Conference in Honor of M. Ali Khan, Johns Hopkins University, 2013. Associate Editor, International Journal of Game Theory, 2003 - 2009. Associate Editor, Journal of Mathematical Economics, 1994 - 2009. Associate Editor, Journal of Public Economic Theory, 2001 - 2005. Member, Program Committee, World Congress of the Econometric Society, 2005. Co-Chair, Program Committee, 2004 Econometric Society North American Summer Meetings, Brown University. Co-Organizer, 2001 NSF-CEME General Equilibrium Conference, Brown University. Organizer, 1994 NSF-CEME General Equilibrium Conference, Brown Uni- versity. -

The Ohio State University, College of Nursing, Centennial Alumni Transformer in Nursing & Healthcare 2014 CNA Virginia A
CURRICULUM VITAE Part I PERSONAL DATA Nancy Reynolds, PhD, RN, C-NP, FAAN Office: Johns Hopkins University, Room 431 525 N Wolfe Street Baltimore, MD 21205 Phone: (410) 955-3096 Email: [email protected] EDUCATION Year Degree Institution/Location 1995 ANP (Post-Master’s) University of Rochester Rochester, NY 1993 PhD Ohio State University Columbus, OH 1988 MS Wright State University Dayton, OH 1977 BSN University of Michigan Ann Arbor, MI POSTDOCTORAL 2004-05 Fellow Ohio State University Committee on Institutional CIC Academic Leadership Columbus, OH Cooperation Program Sponsor: CIC Chief Academic Officers 1998 Fellow University of Minnesota NIH, NCRR (R25RR013127) Interdisciplinary Training Minneapolis, MN Sponsor: Robert Kane, MD in Outcomes Research 1993-95 Postdoctoral Fellow University of Rochester NIH, NINR (T32NR0764) Rochester, NY Sponsor: M. Schmitt, PhD, RN, FAAN CURRENT LICENSE AND CERTIFICATION Year Source Type License Number 2019 MARYLAND RN #T20170897 2018-2020 American Heart Assoc. CPR 185501992606 1 PROFESSIONAL EXPERIENCE Years Position Institution Location 2017- Present Associate Dean of Global Johns Hopkins University, Baltimore, MD Affairs School of Nursing 2015- 2017 Associate Dean Global Yale University, School of Nursing New Haven, CT Health (Interim) 2015-2017 Independence Foundation Yale University, School of Nursing New Haven, CT Professor of Nursing 2008-2013 Director Doctoral and Yale University, School of Nursing, New Haven, CT Postdoctoral Programs 2007- 2017 Professor (Tenured) Yale University, School -

AFTD's 2020 Education Conference
AFTD’s 2020 Education Conference Sheraton Inner Harbor Hotel | Baltimore, MD April 17, 2020, 9:00 a.m. to 5:00 p.m. Every year, AFTD convenes persons diagnosed, care partners, researchers, healthcare professionals and others for our annual Education Conference. Join us this April in Baltimore for a day of learning, sharing and connecting. Find help and share hope with people who understand the FTD journey. Highlights: • Learn about the latest updates in FTD science straight from the researchers who are helping to deepen our understanding of this disease • Take part in interactive breakout sessions focusing on clinical issues and FTD care strategies • Make important connections during specially tailored networking sessions and our evening social reception • Experience a truly unique and rewarding day surrounded by people whose lives have been touched by FTD Register Today! Visit http://tinyurl.com/AFTD2020 today to register for AFTD’s 2020 Education Conference! If you would like to attend but cannot afford the registration fee, please contact [email protected] to request a waiver code to use at registration. Only people living with FTD and current care partners/caregivers and family members are eligible for this option. AFTD’s 2020 Education Conference Sheraton Inner Harbor Hotel | Baltimore, MD April 17, 2020, 9:00 a.m. to 5:00 p.m. Featured Speakers Keynote Speaker: Halima Amjad, Katie Brandt, MM, Rome Hartman MD, MPH, Assistant Director of Caregiver is a producer of Professor of Support Services the venerable Medicine at Johns in the FTD Unit at CBS news Hopkins University Mass General and program 60 School of Medicine Co-Chair of the NAPA Advisory Minutes, which Council last May aired a segment he Murray Grossman, produced about FTD. -

Recruitment.Pdf
Three Ph.D. Positions in Computer Science @ The Johns Hopkins University Dr. Yinzhi Cao from Johns Hopkins University is looking for three Ph.D. students with strong engineering and/or computer science background. Interested students could email Dr. Cao at [email protected] for any questions (see his webpage https://www.yinzhicao.org for details), and apply through the web portal (https://www.cs.jhu.edu/graduate-studies/graduate-admissions- information/). The ideal candidate will have strong system building ability in cyber-security and privacy. Program analysis and/or machine learning background are preferred. He/she will be self- motivated and enjoy working with other people in a team. Dr. Yinzhi Cao graduated from Tsinghua University with bachelor of engineering and Northwestern University with a Ph.D. degree. After that, he spent one year at Columbia University as a postdoc, and three years at Lehigh University as an assistant professor. He will join Johns Hopkins University as an assistant professor in August 2018. Dr. Cao’s research spans from web/mobile security and privacy to adversarial machine learning. He has been actively publishing in top-tier security/system conferences, such as IEEE Security and Privacy (Oakland), SOSP, USENIX Security, NDSS and CCS. He has won two best paper awards, one at SOSP'17 and the other at IEEE CNS'15. His work has been widely reported by many media outlets, including CCTV, NSF Science News, and The Atlantic. Dr. Yinzhi Cao will be actively guiding Ph.D. students in pursuing research in cybersecurity and privacy. Johns Hopkins University is a private university located at Baltimore, MD. -
Technical Program
Technical Program Third International Symposium on Nanoporous Materials by Alloy Corrosion Philadelphia, PA, USA February 24-28, 2019 Organizers: Joshua Snyder, Ian McCue, Haijun Jin Conference Website: http://www.chemeng.drexel.edu/snyderlab/symposium/index.html Third International Symposium on Nanoporous Materials by Alloy Corrosion Sunday, Feb 24 Monday, Feb 25 Tuesday, Feb 26 Wednesday, Feb 27 Thursday, Feb 28 Time 7:30 - 8:40 Breakfast Breakfast Breakfast Breakfast Fundamentals of Pattern Self Organized Fromation During Selective Morphologies via New Catalysis at the Nanoscale I Dissolution Mechanisms Session Chair: Laetitia Dubau Session Chair: Qing Chen Session Chair: Zhen Lu 8:40 - 9:20 Jonah Erlebacher Qing Chen Feng Jiao 9:20 - 10:00 Ian McCue Mingwei Chen Frederic Maillard 10:00 - 10:40 Roger Newman Joseph Ryan Jurgen Biener Departure 10:40 - 11:00 Break Haomin Liu Break Morphological Coarsening Liquid Metal Dealloying Catalysis at the Nanoscale II Session Chair: Eva-Maria Session Chair: Karen Chen- Session Chair: Pietro Lopes Steyskal Wiegart 11:00 - 11:20 Samuel Welbron Gina Greenidge Matthias Graf 11:20 - 12:00 Peter Voorhees Hidemi Kato Eric Desti 12:00 - 13:30 Lunch Lunch Lunch In-situ and Direct Understanding the Impact Mechanical Response at the Measurements at the of Kinetics on Pattern Nanoscale I Nanoscale Formation Session Chair: Haijun Jin Session Chair: Qi Zhen Session Chair: Ian McCue 13:30 - 14:10 Diana Farkas Mitsu Murayama Karen Chen-Wiegart 14:10 - 14:50 Jorg Weissmuller Erica Lilleodden Alain Karma 14:50 -
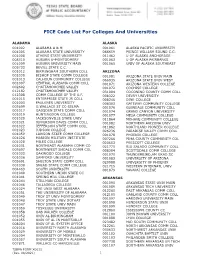
FICE Code List for Colleges and Universities (X0011)
FICE Code List For Colleges And Universities ALABAMA ALASKA 001002 ALABAMA A & M 001061 ALASKA PACIFIC UNIVERSITY 001005 ALABAMA STATE UNIVERSITY 066659 PRINCE WILLIAM SOUND C.C. 001008 ATHENS STATE UNIVERSITY 011462 U OF ALASKA ANCHORAGE 008310 AUBURN U-MONTGOMERY 001063 U OF ALASKA FAIRBANKS 001009 AUBURN UNIVERSITY MAIN 001065 UNIV OF ALASKA SOUTHEAST 005733 BEVILL STATE C.C. 001012 BIRMINGHAM SOUTHERN COLL ARIZONA 001030 BISHOP STATE COMM COLLEGE 001081 ARIZONA STATE UNIV MAIN 001013 CALHOUN COMMUNITY COLLEGE 066935 ARIZONA STATE UNIV WEST 001007 CENTRAL ALABAMA COMM COLL 001071 ARIZONA WESTERN COLLEGE 002602 CHATTAHOOCHEE VALLEY 001072 COCHISE COLLEGE 012182 CHATTAHOOCHEE VALLEY 031004 COCONINO COUNTY COMM COLL 012308 COMM COLLEGE OF THE A.F. 008322 DEVRY UNIVERSITY 001015 ENTERPRISE STATE JR COLL 008246 DINE COLLEGE 001003 FAULKNER UNIVERSITY 008303 GATEWAY COMMUNITY COLLEGE 005699 G.WALLACE ST CC-SELMA 001076 GLENDALE COMMUNITY COLL 001017 GADSDEN STATE COMM COLL 001074 GRAND CANYON UNIVERSITY 001019 HUNTINGDON COLLEGE 001077 MESA COMMUNITY COLLEGE 001020 JACKSONVILLE STATE UNIV 011864 MOHAVE COMMUNITY COLLEGE 001021 JEFFERSON DAVIS COMM COLL 001082 NORTHERN ARIZONA UNIV 001022 JEFFERSON STATE COMM COLL 011862 NORTHLAND PIONEER COLLEGE 001023 JUDSON COLLEGE 026236 PARADISE VALLEY COMM COLL 001059 LAWSON STATE COMM COLLEGE 001078 PHOENIX COLLEGE 001026 MARION MILITARY INSTITUTE 007266 PIMA COUNTY COMMUNITY COL 001028 MILES COLLEGE 020653 PRESCOTT COLLEGE 001031 NORTHEAST ALABAMA COMM CO 021775 RIO SALADO COMMUNITY COLL 005697 NORTHWEST -

Irene-Pang-Cv.Pdf
IRENE PANG Buffett Institute for Global Studies Northwestern University 1902 Sheridan Road, Evanston, IL 60208 Email:[email protected] Phone: (443) 527-5809 ACADEMIC POSITION 2017 – Postdoctoral Fellow, Buffett Institute for Global Studies, Northwestern University EDUCATION Ph.D. Sociology, Brown University, 2017 Dissertation: Becoming Citizens: Construction Workers in Beijing and Delhi Committee: Nitsan Chorev (Chair), Joel Andreas (Johns Hopkins), Patrick Heller, José Itzigsohn Preliminary Exam Areas: Social Theory (passed with distinction), Political Economy of Development and Globalization (passed with distinction) Visiting Scholar, Center for Modern Indian Studies & Center for Modern East Asian Studies, Georg-August-Universität Göttingen, Germany (Summer 2016) A.M. Sociology, Brown University, 2012 B.A. (Hons) Sociology, Johns Hopkins University, 2009 Semester Abroad: Freie-Universität Berlin / Humboldt-Universität zu Berlin (Spring 2009) Semester Abroad: University of Ghana (Fall 2007) RESEARCH INTERESTS Political Sociology, Development, Citizenship, Labor, Ethnography, Comparative Research, China and India PUBLICATIONS 2016. “Banking is for Others: Contradictions of Microfinance in the Ghanaian Market,” Journal of World-Systems Research 22(2):335-66. * Terence K. Hopkins Graduate Student Paper Award, American Sociological Association, Political Economy of the World-System Section n.d. “The Legal Construction of Precarity: Lessons from the Construction Sector in Beijing and Delhi,” under review at Critical Sociology. WORKING -

555 Pennsylvania Avenue
555 Pennsylvania Avenue July 3, 2019 • Establish a greater Johns Hopkins University identity in the District of Columbia • Provide a portal for Baltimore programs in Washington, D.C. and vice versa • Offerconvening space for topic experts, policymakers, academic and policy leaders • Create a collaborative learning and working environment • Provide a platform to introduce innovative pedagogy • Provide long term flexibility to support expanded Johns Hopkins University programs • Integrate best practices for sustainability and resilience and operational efficiency • Leverage transparency to reinforce and create new community • Increase access to natural daylight throughout the entire building • Organize and simplify to create circulation patterns ideal for higher education use • Promote health and wellness throughout • Enliven Pennsylvania Avenue and the surrounding neighborhood Project Goals 555 Pennsylvania Avenue | Johns Hopkins University July 3, 2019 2 While in the early stages, JHU and the SmithGroup/Ennead The street level along Pennsylvania Avenue will be updated team is working on a design that refreshes 555 Pennsylvania to provide greater transparency and sidewalk activation, Avenue to create a place that is distinctly associated with creating a fluid and inviting interface with the public. Together, the Johns Hopkins University mission and at the same time the combined changes will reinforce the facility’s new identity respects the surrounding context. as the D.C. home for Johns Hopkins. The scale and massing of the original building design, including regulating boundary lines The design under consideration proposes enhancements to respectful of the historic Pennsylvania Avenue corridor, will be the building façade that strengthen continuity with traditional unchanged. Pennsylvania Avenue landmarks of note, including the use of stone reminiscent of the warm color and texture found on the Internal revisions will include the introduction of flexible, National Gallery and East Building. -

Mid-Atlantic Conference on British Studies 2015 Annual Meeting The
Mid-Atlantic Conference on British Studies 2015 Annual Meeting The Johns Hopkins University March 27-28, 2015 Friday March 27 All events will take place at Charles Commons unless otherwise noted. 10:00am–12:00pm Registration and Coffee Registration Area SESSION ONE: 12:00-1:30pm i. Historicizing the English Garden: Space, Nature, and National Identity in Modern Britain Salon A i. Robyn Curtis (Australian National University): “‘The Voice of Nature’: Conservation in Nineteenth Century England” ii. Ren Pepitone (Johns Hopkins University): “‘Common People in the Temple Gardens’: Regulating Space in the Metropolitan Center” iii. Terry Park (Miami University): “De/militarized Garden of Feeling: Jihae Hwang’s Quiet Time: DMZ Forbidden Garden” iv. Chair/Comment: Douglas Mao (Johns Hopkins University) ii. The Nation in Print: Text, Image, and Readership in Early Modern Britain Salon B i. Melissa Reynolds (Rutgers University): “Icons and Almanacs: Visual Practice and Non-Elite Book Culture in Late Medieval and Early Modern England” ii. Jessica Keene (Johns Hopkins University): “‘Certain most godly, fruitful, and comfortable letters’: Prison Letters, Protestantism, and Gender in Reformation England” iii. Joshua Tavenor (Wilfred Laurier University): “When Words are not Enough: the Promotion of Cuper’s Cove, Newfoundland in Seventeenth-century England” iv. Chair/Comment: Mary Fissell (Johns Hopkins University School of Medicine) iii. Charity and Commerce Interwoven in the British Empire Salon C i. Amanda Moniz (National History Center): “White’s Ventilator, or How the Lifesaving Cause Aided Abolition and the Slave Trade” ii. Karen Sonnelitter (Siena College): “Financing Improvement: Funding Charity in Eighteenth-Century Ireland” iii. Karen Auman (Brigham Young University): “For Faith and Profit: German Lutherans and the British Empire” iv. -

BEAM Programming and Curriculum
BEAM Programming and Curriculum Manuel Santiago, Tracy Downs, Tiajuana Rice MS.Ed. MD, FACS Angela Byars-Winston, Christine Sorkness, Carrie Brinkmeier PhD RPh, PharmD 2021 BEAM Mentors Ticiana A. Leal, MD Makeba Williams, Patricia Téllez-Girón, Dawd Siraj, MD, MPH Miguel Leal, MD, NCMP, FACOG MD MD, FACC, FHRS Jason Stephenson, MD Pablo Gómez, Héctor Valdivia, Erick Tarula, MD Maria Daniela Martin, MD, PhD MD, PhD MD Shaneda Warren Marcus Chacon, MD Sheryl Henderson, Sancia Ferguson, Christine Sharkey, MD Andersen, MS, PhD MD, PhD MD, MPH Thalia Marie Williams, Lisa Jones, Elizabeth Felton, Freddy Caldera, Tiffany Green, PhD MA, MS, CLA-Cert., PhD MD, MPH, MMCi MD, PhD DO, MS Reinier Hernandez, Tracy Downs, PhD MD, FACS Tracy Downs, MD, FACS [email protected] Department: Urology Specialty: Minimally invasive urologic surgery and urologic oncology Dr. Downs is a Professor of Urology at the University of Wisconsin School of Medicine and Public Health in Madison, Wisconsin. He is also a board-certified urologist, specializing in the surgical treatment of urologic cancers. He has a special interest in the treatment of bladder cancer and prostate cancer. Surgically he has extensive experience in performing complex urinary reconstruction to make a new internalized bladder from a patient’s intestinal tissue (orthotopic neobladder). Dr. Downs’ clinical care philosophy is to provide compassionate, cutting-edge urologic cancer care to his patients. He has a joint appointment with the UW Carbone Cancer Center, and his clinical research emphasizes developing new therapies for genitourinary cancers. Dr. Downs completed his medical training at the University of California-San Diego (UCSD) School of Medicine, his urologic surgery residency at Harvard, and a two-year urologic oncology fellowship at the University of California-San Francisco (UCSF). -

OSU Winter Invite - Saturday Finals
McCorkle Aquatic Pavilion - Site License HY-TEK's MEET MANAGER 7.0 - 6:16 PM 2/15/2020 Page 1 Ohio State Winter Invite 2020 - 2/14/2020 to 2/16/2020 Results - OSU Winter Invite - Saturday Finals Event 11 Women 200 Yard Medley Relay 1:36.40 A 1:37.05 B Team Relay Finals Time 1 Akron, University of-LE B 1:40.67 1) Kaufman, Victoria E FR 2) r:0.10 Fischer, Andrea SO 3) r:0.09 Nogaj, Paulina JR 4) r:0.10 Henell, Sofia SO 13.18 26.44 (26.44) 38.88 (12.44) 54.38 (27.94) 1:05.09 (10.71) 1:18.10 (23.72) 1:28.65 (10.55) 1:40.67 (22.57) 2 Akron, University of-LE A 1:41.04 1) Gorecka, Weronika M FR 2) r:0.19 Garcia, Paula JR 3) r:0.21 Watson, Sarah SO 4) r:-0.31 Waggoner, Morgan SR 13.21 26.37 (26.37) 39.95 (13.58) 54.66 (28.29) 1:05.51 (10.85) 1:18.55 (23.89) 1:29.23 (10.68) 1:41.04 (22.49) 3 Notre Dame, University of-IN A 1:45.35 1) Deselm, Claire M SR 2) r:0.29 Eyolfson, Sammie SO 3) r:0.37 Potter, Madison FR 4) r:0.50 Jacob, Kelly SR 13.77 27.58 (27.58) 40.92 (13.34) 57.36 (29.78) 1:08.54 (11.18) 1:22.07 (24.71) 1:33.24 (11.17) 1:45.35 (23.28) --- Johns Hopkins University-MD A DQ Early take-off swimmer #2 1) Bisignani, Mikayla R JR 2) r:0.28 State, Claire SR 3) r:-0.06 Davis, Emerson FR 4) r:0.37 Alicea-Jorgensen, Kristen SO 13.38 26.65 (26.65) 40.37 (13.72) 57.58 (30.93) 1:09.43 (11.85) 1:23.83 (26.25) 1:34.91 (11.08) DQ (23.61) Event 12 Men 200 Yard Medley Relay 1:24.30 A 1:24.97 B Team Relay Finals Time 1 Ohio State University-OH A 1:29.85 1) Roy, Colin N SO 2) r:0.22 Mikesell, Ian FR 3) r:0.43 Silver, Kyle FR 4) r:0.20 Sugar, Jonathan FR -

Department of Economics Newsletter
DEPARTMENT OF ECONOMICS NEWSLETTER Department of Economics Newsletter May 2015 GENERAL DEPARTMENT NEWS The Economics Department at Johns 2016. Professor Quah is an economic Poster for the Richard Ely Distinguished Hopkins has had another busy year with theorist with many major works to his credit Lecture Series 2014-2015: multiple events and many developmentsMay 20and15 is an outstanding addition to the among the faculty and graduate students. Department. This Newsletter will cover many of them but feel free to keep track of all developments as The Department was well represented at the they happen on the department website, AEA Meetings in January, 2015 in Boston. http://www.econ.jhu.edu/. Among the faculty, Chris Carroll, Olivier Jeanne, Ali Khan, Anton Korinek, Robert We welcomed Assistant Professor Ying Chen Moffitt, Nick Papageorge, and Yuya Sasaki to the Department in September. Ying were on the program. The traditional cocktail specializes in Economic Theory and comes party and reception also drew a number of from Southampton and Arizona State and current and former graduate students and received her Ph.D. from Yale. Ying is faculty. We will be having another in January, teaching graduate and undergraduate 2016 in San Francisco. Mark it on your courses in micro theory. calendars. We look forward to the Spring 2016 Ely We are also happy to report that Dr. Robert Our annual Richard T. Ely Lecture this year Lectures as well, which will be given by Barbera, a graduate alumnus from our was given by John Geanakoplos (photo Professor Robert Porter of Northwestern Department, has continued his stepped up below) from Yale University, who gave four University.