Exploring the Interaction of Activity Limitations with Context, Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Health Professions Act: List of Approved Facilities for the Purposes of Performing Community Service by Dentists in the Year
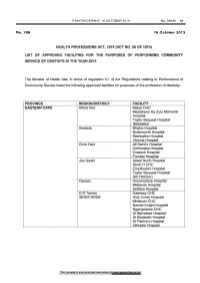
STAATSKOERANT, 16 OKTOBER 2013 No. 36936 13 No. 788 16 October 2013 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY DENTISTS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service listed the following approved facilities for purposes of the profession of dentistry. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Maluti CHC Madzikane Ka Zulu Memorial Hospital Taylor Bequest Hospital (Matatiele) Amato le Bhisho Hospital Butterworth Hospital Madwaleni Hospital Victoria Hospital Chris Hani All Saint's Hospital Cofimvaba Hospital Cradock Hospital Frontier Hospital Joe Gqabi Aliwal North Hospital Block H CHC Empilisweni Hospital Taylor Bequest Hospital (Mt Fletcher) Cacadu Humansdorp Hospital Midlands Hospital Settlers Hospital O.R Tambo Gateway CHC ISRDS NODE Holy Cross Hospital Mhlakulo CHC Nessie Knight Hospital Ngangelizwe CHC St Barnabas Hospital St Elizabeth Hospital St Patrick's Hospital Zithulele Hospital This gazette is also available free online at www.gpwonline.co.za 14 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 FREE STATE Motheo District(DC17) National Dental Clinic Botshabelo District Hospital Fezile Dabi District(DC20) Kroonstad Dental Clinic MafubefTokollo Hospital Complex Metsimaholo/Parys Hospital Complex Lejweleputswa DistrictWelkom Clinic Area(DC18) Thabo Mofutsanyana District Elizabeth Ross District Hospital* (DC19) Itemoheng Hospital* ISRDS NODE Mantsopa -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 32, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 8 August 2020 on the DATCOV platform. HIGHLIGHTS As of 8 August 2020, 965 (2.0%) of the 49106 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 161 facilities (47 public-sector and 114 private-sector) in all nine provinces of South Africa. Among 565/965 (58.5%) HCWs with available data on type of work, 262/565 (46.4%) were nurses, 175/565 (31.0%) were categorized as other HCWs, 30/565 (5.3%) porters or administrators, 29/565 (5.1%) allied HCWs, 24/565 (4.2%) doctors, 13/565 (2.3%) paramedics, and 6/565 (1.1%) laboratory scientists. There was an increase of 82 new HCW admissions since week 31. There were 214 (22.2%) and 751 (77.8%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (289, 29.9%), KwaZulu-Natal (267, 27.7%), Western Cape (115, 11.9%), Free State (99, 10.3%) and Eastern Cape (93, 9.6%). The median age of COVID-19 HCW admissions was 45 years, there were 92 (9.5%) admissions in HCWs aged 60 years and older. A total of 765 (79.3%) were female. -

An Exploration and Description of Rural Rehabilitation Service Model in the Mbhashe Municipality, Amathole District in the Easte
AN EXPLORATION AND DESCRIPTION OF RURAL REHABILITATION SERVICE MODEL IN THE MBHASHE MUNICIPALITY, AMATHOLE DISTRICT IN THE EASTERN CAPE PROVINCE OF SOUTH AFRICA: A PILOT STUDY (Presented in an article format for the African Journal of Disability). Nozipiwo Joyce Gysman Submitted in partial fulfilment of the re quirements for the degree MSc Med Sc. R ehabilitation Studies (Structured) Centre for Rehabilitation Studies Stellenbosch University 2020 Supervisor: Prof Gubela Mji Stellenbosch University https://scholar.sun.ac.za DECLARATION I, Nozipiwo Joyce Gysman declare that the work contained in this research assignment is entirely my own, original work (except where acknowledgement indicates otherwise), and it has not been previously submitted for any other degree at Stellenbosch University or at another University. Nozipiwo Joyce Gysma Date: March 2020 Copyright © 2020 Stellenbosch University All rights reserved Stellenbosch University https://scholar.sun.ac.za ABSTRACT Background People with disabilities are still disadvantaged in accessing health and rehabilitation services, especially those who reside in rural areas, despite the available policies. Rehabilitation is one of the components of Primary Health Care (PHC) but it remains excluded and poorly understood in PHC programmes. Despite available policies to address rehabilitation for people with disabilities (PWDs), PWDs still have difficulty accessing the rehabilitation services. Rehabilitation remains: • excluded and poorly understood in PHC programmes, • fragmented and uncoordinated with services inaccessible to some parts of society especially in the rural context compared to urban counterparts, • dominated by the medical model and institutionalization of services, and • questionable in terms of relevance of services as there is less involvement, guidance and support from communities where these rehabilitation services are being provided. -

Eastern Cape Department of Health Applications
ANNEXURE K PROVINCIAL ADMINISTRATION: EASTERN CAPE DEPARTMENT OF HEALTH APPLICATIONS : Applications should be posted to the addresses as indicated below or Hand delivered as indicated below: Isilimela Hospital - Post to: Isilimela Hospital P/Bag X1021, Port St Johns, 5120 or Hand deliver to Isilimela Hospital Port St Johns, 5120, Enquiries: Ms N Gwiji Tel No: 047 564 2805 St Lucys Hospital - Post to: Human Resource Office, St Lucy’s Hospital, P.O St Cuphberts, Tsolo, 5171. Enquiries: Ms Mayikana Tel No: 047 532 6259. St Barnabas Hospital - Post to: Human Resource Office, St Barnabas Hospital, P.O. Box 15, Libode, 5160. Enquiries: Ms Ndamase – Tel No: 047 555 5300 St Elizabeth Regional Hospital - Post to: Human Resource Office, St Elizabeth Regional Hospital, Private Bag x1007, Lusikisiki, 4820. Enquiries: Mr M Nozaza – Tel No: 039 253 5012. Nyandeni Sub District - Post to Human Resource Office Nyandeni LSA P. O. Box 208, Libode, 5160, or Hand Deliver to Nomandela Drive opposite traffic Department, Libode, 5160, Enquiries: Ms Daniso – Tel No: 047 555 0151 Nelson Mandela Academic Hospital - Post to: Nelson Mandela Academic Hospital, Private Bag x5014 Mthatha 5099. Hand Deliver to: Human Resource Office, Nelson Mandela Academic Hospital, Nelson Mandela Drive, Mthatha 5099. Enquiries: Ms Calaza Tel No: 047 502 4469 Canzibe Hospital - Post to Human Resource Office Canzibe Hospital, P/Bag X104, Ngqeleni, 5140 or Hand Deliver to Hospital, Ngqeleni Enquiries: Ms Solwandle – Tel No: 047 562 8812 /7 OR Tambo District Office - Post to: District Manager, OR Tambo Health District Office, Private Bag X 5005, Mthatha 5099 or Hand Delivery 9th Floor Room 19 Botha Sigcawu Building Enquiries: Mr S Stuma Tel No: 047 502 9000. -
Health Professions Act: List of Approved Facilities for Community
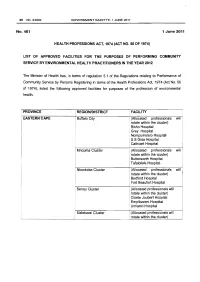
36 No.34332 GOVERNMENT GAZETTE, 1 JUNE 2011 No. 461 1 June 2011 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY ENVIRONMENTAL HEALTH PRACTITIONERS IN THE YEAR 2012 rhe Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 197 4 ), listed the following approved facilities for purposes of the profession of environmental health. I PROVINCE REGION/DISTRICT FACILITY • EASTERN CAPE Buffalo City (Allocated professionals will rotate within the cluster) Bisho Hospital Grey Hospital Nompumelelo Hospital S.S Gida Hospital Cathcart Hospital I Mnquma Cluster (Allocated professionals will rotate within the cluster) Butterworth Hospital Tafalofefe Hospital Nkonkobe Cluster (Allocated professionals will rotate within the cluster) Bedford Hospital Fort Beaufort Hospital Senqu Cluster (Allocated professionals will rotate within the cluster) Cloete Joubert Hospital Empilisweni Hospital Umlamli Hospital Maletswai Cluster (Allocated professionals will rotate within the cluster) STAATSKOERANT, 1 JUNIE 2011 No.34332 37 Aliwal North Hospital Steynsburg Hospital Burgersdorp Hospital Sakhisizwe Cluster (Allocated professionals will rotate within the cl~ster) Cala Hospital Elliot Hospital Glen Grey Hospital i ' Makana Cluster (Allocated professionals will ! rotate within the cluster) • Port Alfred Hospital ! Settlers Hospital Camdeboo Cluster -

Health Professions Act: List of Approved Facilities for Performing Community Service by Pharmacists: in 2010
STAATSKOERANT, 11 JUNIE 2009 No.32308 3 GOVERNMENT NOTICES DEPARTMENT OF HEALTH No. R. 659 11 June 2009 PHARMACY ACT, 1974 (ACT NO. 53 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY PHARMACISTS IN THE YEAR 2010 The Minister of Health has, in terms of regulation 3 of the Regulations relating to Performance of Pharmaceutical Community Service, listed the following approved facilities for purposes of the profession of pharmacy. PROVINCE Region (District) FACILITY DEPARTMENT OF HEALTH- PUBLIC HEALTH FACILlrlES EASTERN CAPE ALFRED NZO Khotsong Hospital* Maluti CHC* Mary Theresa Hospital ** Mt Ayliff Hospital ** Sipetu Hospital ** Tabankulu CHC** Tayler Bequest Hospital(Maluti) * Tayler Bequest Hospital(Elundi) * AMATHOLE Bhisho Hospital Bedford Hospital * Butterworth Hospital * Cathcart Hospital Cecilia Makiwane Hospital Duncan Village Day CHC Dutywa CHC Empilweni Gompo CHC Fort Beaufort Hospital Fort Grey Hospital Frere Hospital Grey Hospital Nompumelelo Hospital * SS Gida Hospital* Tafalofefe Hospital* Tower Hospital Victoria Hospital * Willowvale CHC Winterberg Hospital AIDS HELPLINE OBO()'Ol·23-22 4 No.3230B GOVERNMENT GAZETTE, 11 JUNE 2009 CACADU Andries Vosloo Hospital * Empilweni Hospital Fort England Hospital * Humansdorp Hospital * Margery parkes* Marjorie Parish Hospital * Midland Hospital * Orsmond Hospital* Port Alfred Hospital * PZ Meyer* Settlers Hospital * Temba Hospital* Uitenhage Hospital * CHRIS HANI All Saints Hospital ** Cala Hospital ** Cofimvaba Hospital ** Cradock Hospital ** -

Health Professions Act: List of Approved Facilities for the Purposes
STAATSKOERANT, 16 OKTOBER 2013 No. 36936 39 No. 791 16 October 2013 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY MEDICAL PRACTITIONERS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of medicine. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Khotsong Hospital* Madzikane kaZulu Hospital ** Umzimvubu Cluster Mt Ayliff Hospital** Taylor Bequest Hospital* (Matatiele) Amathole Bhisho CHH Cathcart Hospital * Amahlathi/Buffalo City Cecilia Makiwane Hospital Cluster Dimbaza CHC Duncan Village Day Hospital Empilweni Gompo CHC Fort Grey TB Hospital Frere Hospital Grey Hospital * Komga Hospital Nkqubela TB Hospital Nompumelelo Hospital* SS Gida Hospital* Stutterheim FPA Hospital* Mnquma Sub-District Butterworth Hospital* Nqgamakwe CHC* Nkonkobe Sub-District Adelaide FPA Hospital Tower Hospital* Victoria Hospital * Mbashe /KSD District Elliotdale CHC* Idutywa CHC* Madwaleni Hospital* Chris Hani All Saints Hospital** Engcobo/IntsikaYethu Cofimvaba Hospital** Martjie Venter FPA Hospital This gazette is also available free online at www.gpwonline.co.za 40 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 Sub-District Mjanyana Hospital * InxubaYethembaSub-Cradock Hospital** Wilhelm Stahl Hospital** District Inkwanca -
A Dialogue on ART Delivery
A Dialogue on ART Delivery A dialogue on the delivery of antiretroviral treatment in resource-limited settings, held at Maropeng, Cradle of Humankind, Gauteng, South Africa, September 2006 A DIALOGUE ON ART MODELS Foreword by Nelson Mandela IN 2003, I launched the Siyaphila La HIV and AIDS treatment programme in Lusikisiki, in the Eastern Cape, a joint project between Médecins Sans Frontières (MSF) and my Foundation. The project has been a shining example of how an antiretroviral (ARV) treatment programme can be implemented successfully, even in a rural area with few resources. Today, the project is a useful touchstone in talking about how to achieve the universal delivery of ARV drugs. If we can learn from the lessons of Lusikisiki and other similar projects, it can help us in our long-term fight against HIV and AIDS. Through the communication and sharing that dialogue allows, we will be able to save more lives. We are now at a point where the project has been handed over to the provinicial Department of Health, to continue to run as a successful model for ARV rollout. We salute the community of Lusikisiki for its active support and participation in this campaign against HIV and AIDS, as well the valuable contribution of the health professionals and government officials who have participated in this initiative. The success of the Siyaphila La project shows that we are breaking down the stigma surrounding the disease, and creating a supportive environment in which HIV-positive patients can speak openly about their status. This project shows that the fight against HIV and AIDS can only be won if it is led by the communities affected by the disease, and if government and civil society unite with one another in partnership against the pandemic. -

Ptc Eastern Cape Course Report
PTC EASTERN CAPE COURSE REPORT By Dr. R. JAYAKRISHNAN CHIEF MEDICAL OFFICER DEPARTMENT OF SURGERY NELSON MANDELA ACADEMIC HOSPITAL MTHATHA, EASTERN CAPE PROVINCE INTRODUCTION Following a very successful foundation course held early in 2007, PTC Eastern Cape conducted the first course in South Africa. The course was run with ample support from the provincial department of health of Eastern Cape and Walter Sisulu University. The Departments of Surgery, Anaesthesia and Family Medicine of Nelson Mandela Academic Hospital participated by contributing their staff that was trained on the earlier occasion as trainers. BACKGROUND Trauma is one of the commonest pathologies encountered in South Africa and the Province of eastern cape is no exception. All medical personals are expected to have a sound understanding of managing trauma patients. It was noticed that the standard of care offered to trauma patients was not up to standards expected resulting in significant mortality and morbidity, which is to a large extent avoidable. Prof Adekunle from the Department of Surgery discussed with Dr KLN Mafanya, the Head of the Clinical Governance of Nelson Mandela Academic Hospital Complex about offering PTC course to professionals in the peripheral hospitals thereby empowering them with the knowledge to manage trauma patients. The department fully supported the idea and it was decided to conduct the first PTC course on the 5 th and 6 th of November to be followed by further courses in the future PTC COURSE The venue of the course was Walter Sisulu University in Mthatha. Prof. E L Mazwai, the Dean for the Faculty of Health Sciences opened the programme. -

Health Professions Act: List of Approved Facilities for Purposes Of
40 No. 35624 GOVERNMENT GAZETTE, 27 AUGUST 2012 No. 676 27 August 2012 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY MEDICAL PRACTITIONERS IN THE YEAR 2013 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following facilities for purposes of the profession of medicine. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Khotsong Hospital* Madzikane kaZulu Hospital ** Umzimvubu Cluster Mt Ayliff Hospital ** Taylor Bequest Hospital* (Matatiele) Amato le Cathcart Hospital * Cecilia Makiwane Hospital Amahlathi/Buffalo City Dimbaza CHC Cluster Fort Grey TB Hospital Grey Hospital * Komga Hospital Nkqubela TB Hospital Nompumelelo Hospital* SS Gida Hospital* Stutterheim FPA Hospital* Mnquma Sub-District Butterworth Hospital* Nqgamakhwe CHC* Nkonkobe Sub-District Adelaide FPA Hospital Tower Hospital* Victoria Hospital * Mbashe /KSD District Elliotdale CHC* Idutywa CHC* Madwaleni Hospital* Zitulele Hospital * Chris Hani All Saints Hospital ** Cofimvaba Hospital ** Engcobo/IntsikaYethu Martjie Venter FPA Hospital Sub-District Mjanyana Hospital * STAATSKOERANT, 27 AUGUSTUS 2012 No. 35624 41 lnxubaYethemba Sub-Cradock Hospital ** Wilhelm Stahl Hospital ** District Inkwanca Molteno FPA Hospital Lukhanji Frontier Hospital* Hewu Hospital * Komani Hospital* Sakhisizwe/Emalahleni Cala Hospital ** Dordrecht FPA Hospital Glen Grey Hospital ** Indwe FPA Hospital Ngonyama CHC* Nelson Mandela Metro Dora Nginza Hospital Empilweni TB Hospital PE Metro Jose Pearson TB Hospital Orsmond TB Hospital Letticia Barn CHC PE Provincial Uitenhage Hospital Kouga Sub-District Humansdorp Hospital BJ Voster FPA Hospital O.R.Tambo Dr Lizo Mpehle Memorial Hospital ** Nessie Knight Hospital ** Mhlontlo Sub-District Qaukeni North Sub-Greenville Hospital ** Holly Cross Hospital ** District Isipethu Hospital* Port St Johns CHC* St. -

Division of Revenue Act: Health Infrastructure Projects List Funded
STAATSKOERANT, 13 JUNIE 2013 No. 36564 3 GENERAL NOTICE NOTICE 612 OF 2013 DEPARTMENT OF HEALTH PUBLICATION OF HEALTH INFRASTRUCTURE PROJECTS LIST FUNDED THROUGH THE HEALTH FACILITY REVITALISATION GRANT AND THE NATIONAL HEALTH GRANT (INFRASTRUCTURE COMPONENT) IN TERMS OF SECTION 13, OF THE DIVISION OF REVENUE ACT, 2013 I,Dr Aaron Motsoaledi, Minister of Health, hereby publish in the gazette Health Infrastructure Projects list funded through Health Facility Revitalisation Grant and the National Health Infrastructure Grant, which will be implemented during 2013/14 finan, ear as submitted by provinces. N MOTSOALEDI, MP I ISTEROF EALTH I DATE: '13 Correspondence on the published Health Infrastructure Projects list can be directed to the Director-General of Health for the attention of the Programme Manager: DeputyDirector-General: Hospitals, TertiaryandWorkforce Management, Dr. T Carter or ActingCluster Manager: Health Facilities and Infrastructure Management, Mr NN Mphaphuli at Department of Health, P/Bag X828, Pretoria, 0001 This gazette is also available free online at www.gpwonline.co.za 4 PROJECTPROVINCE LIST FORFACILITY HEALTH NAME FACILITY REVITALISATIONPROJECT DESCRIPTION GRANT: 2013/14 FINANCIAL YEAR SOURCEFUNDING OF 2013/14ALLOCATION BUDGET No. 36564 GAZETTE,13JUNE2013 GOVERNMENT EC Cecilia Makiwane Hospital Phase 4C - Construction of Main Hospital HRG 173R000' 528 This gazette isalsoavailable freeonline at EC Frontier Hospital Construction of Prefabricated units for Nurses College NCSG 3 992 EC Frontier Hospital Construction of -

Health Professions Act, 1974 (Act No
102 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 No. 796 16 October 2013 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY RADIOGRAPHERS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of radiography. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE AMATHOLE (Allocated professionals to rotate within the cluster) Buffalo City/AmahlathiBhisho Hospital Cluster Cathcart Hospital Grey Hospital Nompumelelo Hospital S.S Gida Hospital Fort Grey TB Hospital Nkqubela TB Hospital East London Complex Cecilia Makiwane Hospital Empilweni Gompo Hospital Frere Hospital Mnquma Cluster Butterworth Hospital Ngqamakhwe CHC Tafalofefe Hospital Mbashe Cluster Idutywa CHC Madwaleni Hospital Nkonkobe Cluster Bedford Hospital Fort Beaufort Hospital Victoria Hospital ALFRED NZO (Allocated professionals to rotate within the cluster) Maluti Cluster Taylor Bequest Hospital (Maluti) Khotsong TB Hospital Umzimvubu Cluster Madzikane ka Zulu Hospital Mt Ayliff Hospital Sipetu Hospital CACADU (Allocated professionals to rotate within This gazette is also available free online at www.gpwonline.co.za STAATSKOERANT, 16 OKTOBER 2013 No. 36936 103 the cluster) Camdeboo Cluster Midlands Hospital Andries Vosloo Hospital Makana Cluster Settlers Hospital