Autoimmune Neutropenia (AIN) in Adults Helen A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
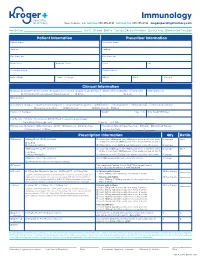
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

Infection Control for Neutropenic Cancer Patients : the Libraryuse of Prophylactic Antibiotics Lecture Author Jean A
Infection control for neutropenic cancer patients : the Libraryuse of prophylactic antibiotics Lecture author Jean A. Klastersky Onlineby Institut Jules Bordet,© Université Libre de Bruxelles (ULB) Brussels, Belgium ESCMID Complications and mortality associated with febrile neutropenia Library No Bacteremia Bacteremia Total ComplicationsLectureDeaths Total Complications Deaths author Solid tumors 784 60 (8 %) 25 135 30 (22 %) 17 Onlineby (3 %) (13 % ) © Hematological cancer 859 111 (13 %) 32 364 76 (21 %) 32 (4 %) (9 %) ESCMID J. Klastersky et al., 2007 2 Complications associated with febrile neutropenia Library Hypotension : systolic blood pressure less than 90 mmHg or need for pressor support to maintain blood pressure Respiratory failure : arterial oxygen pressure less than 60mmHg while breathing room air or needLecture for mechanical ventilation Disseminated intravascular coagulation Confusion or altered mental state author Congestive cardiac failure seen on chest X-ray and requiring treatment Onlineby Bleeding severe enough to require© transfusion Arrhythmia or ECG changes requiring treatment Renal failure requiring investigation and/or treatment with IV fluids, dialysis, or any other intervention ESCMID J. Klastersky et al., 2000 3 Cost of febrile neutropenia Library Initial hospitalization Initial hospitalization plus all downstreamLecture neutropenia care author 2.010 $ Onlineby 14.407 $ © ESCMID D. Weyckler et al., 2008 4 Use of oral antibiotics in protected units environment : clinical effectiveness and role in the emergence -

Neutropenia Fact Sheet
Neutropenia in Barth Syndrome i ii (Chronic, Cyclic or Intermittent) What problems can Neutropenia cause? Neutrophils are the main white blood cell for fighting or preventing bacterial or fungal infections. They may be referred to as polymorphonuclear cells (polys or PMNs), white cells with segmented nuclei (segs), or neutrophils in the complete blood cell count (CBC) report. Immature neutrophils are referred to as bands. When someone is neutropenic (an abnormally low level of neutrophils in the blood), the risk of infection increases. The absolute neutrophil count (ANC) is a measure of the total number of neutrophils present in the blood. When the ANC is less than 1,000, the risk of infection increases. Most infections occur in the ears, skin or throat and to a lesser extent, the chest. These infections can be very serious and may require antibiotics to clear infections. When someone with Barth syndrome is neutropenic his defenses are weakened, he is likely to become seriously ill more quickly than someone with a normal neutrophil count. Tips: • No rectal temperatures as any break in the skin can lead to an infection. • If the individual has a temperature > 100.4° F (38° C) or has infectious symptoms, the primary physician or hematologist should be notified. The individual may need to be seen. • If the individual has a temperature of 100.4° F (38° C) – 100.5° F (38.05° C)> 8 hours or a temperature > 101.5° F (38.61° C), an immediate examination by the physician is warranted. Some or all of the following studies may be ordered: CBC with differential and ANC Urinalysis Blood, urine, and other appropriate cultures C-Reactive Protein Echocardiogram if warranted • The physician may suggest antibiotics (and G-CSF if the ANC is low) for common infections such as otitis media, stomatitis. -

We Work at the Intersection of Immunology and Developmental Biology
Development and Homeostasis of Mucosal Tissues U934/UMR3215 – Genetics and Developmental Biology Pedro Hernández Chef d'équipe [email protected] We work at the intersection of immunology and developmental biology. Our primary goal is to understand how immune responses impact the development, integrity and function of mucosal tissue layers, such as the intestinal epithelium, during homeostasis and upon different types of stress, including infections. To study these questions we exploit the advantages of the zebrafish model such as ex utero and rapid development, transparency, large progeny, and simple genetic manipulation. We combine live imaging, flow cytometry, single-cell transcriptomics, and models inducing mucosal stress, including pathogenic challenges. Our research can be subdivided into three main topics: 1) Protection of intestinal epithelial integrity since early development: Epithelial cells are at the core of intestinal organ function. They are in charge of absorbing nutrients and water, and at the same time constitute a barrier for potential pathogens and harmful molecules. Epithelial cells perform all these functions before full development of the immune system, which promotes epithelial barrier function upon injury. We study how robust epithelial integrity is achieved prior and after maturation of the intestinal immune system, with a focus on the function of mucosal cytokines. 2) Epithelial-leukocyte crosstalk throughout development: Intestines become vastly populated by leukocytes after exposure to external cues from diet and colonization by the microbiota. We have recently reported the existence and diversity of zebrafish innate lymphoid cells (ILCs), a key component of the mucosal immune system recently discovered in mice and humans. ILCs mediate immune responses by secreting cytokines such as IL-22 which safeguards gut epithelial integrity. -

Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics
Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics Jennifer Giuliani, MSc Camosun College, Lansdowne Campus, 3100 Foul Bay Rd, Victoria BC V8P 5J2 [email protected] Abstract The immune response is a wonderfully complex aspect of our physiology that can sometimes confound students and instructors alike. How do we wade through the layers of detail to help our students develop an understanding of immunology? In this article, I will share some of the stories about immunology research that helped me strengthen my own understanding and improve my approach to helping students learn and understand this topic. In addition, we will explore some of the research on the power of storytelling, and how learning through stories might be a defining characteristic of what it means to be human. https://doi.org/10.21692/haps.2020.105 Key words: storytelling, immunology Introduction I have been trying to understand the immune response for a My personal journey to develop a better understanding of long time. Like many Anatomy and Physiology instructors, I the immune system was a compelling reminder to me of the did not have an immunology background beyond what was power of storytelling. Suddenly I saw examples of storytelling covered in my undergraduate physiology courses. When the everywhere that I saw authentic learning. In this article, I will time came for me to teach students about the immune system, share some of what I have learned about learning through I relied heavily on the information presented in our textbooks. stories, some of the fun and fascinating immunology stories I was able to present students with the key pieces of from Davis’ books, and my current approach to helping information and help them to remember a few facts, and the students understand the immune response. -

Journal of Microbiology, Immunology and Infection
JOURNAL OF MICROBIOLOGY, IMMUNOLOGY AND INFECTION AUTHOR INFORMATION PACK TABLE OF CONTENTS XXX . • Description p.1 • Impact Factor p.1 • Abstracting and Indexing p.2 • Editorial Board p.2 • Guide for Authors p.4 ISSN: 1684-1182 DESCRIPTION . Journal of Microbiology, Immunology and Infection, launched in 1968, is the official bi-monthly publication of the Taiwan Society of Microbiology, the Chinese Society of Immunology, the Infectious Diseases Society of Taiwan and the Taiwan Society of Parasitology. The journal is an open access journal, committed to disseminating information on the latest trends and advances in microbiology, immunology, infectious diseases and parasitology. Articles on clinical or laboratory investigations of relevance to microbiology, immunology, infectious diseases, parasitology and other related fields that are of interest to the medical profession are eligible for consideration. Article types considered include perspectives, review articles, original articles, brief reports and correspondence. The Editorial Board of the Journal comprises a dedicated team of local and international experts in the field of microbiology, immunology, infectious diseases and parasitology. All members of the Editorial Board actively guide and set the direction of the journal. With the aim of promoting effective and accurate scientific information, an expert panel of referees constitutes the backbone of the peer- review process in evaluating the quality and content of manuscripts submitted for publication. JMII is open access and indexed in SCIE, PubMed, MEDLINE, EMBASE, Scopus, AIDS & Cancer Reseach, CABI, BIOSIS Previews, Biological Abstracts, EBSCOhost, CancerLit, Reactions Weekly (online), Chemical Abstracts, HealthSTAR, Global Health, ProQuest. Benefits to authors We also provide many author benefits, such as free PDFs, a liberal copyright policy, special discounts on Elsevier publications and much more. -

Vancomycin-Resistant Enterococci Colonization in Patients with Hematological Malignancies: Screening and Its Cost-Effectiveness
Vancomycin-resistant enterococci colonization in patients with hematological malignancies: screening and its cost-effectiveness Gedik Habip1, Şimşek Funda1, Kantürk Arzu1, Yıldırmak Taner1, Arıca Deniz2, Aydın Demet2, Yokuş Osman2, Demirel Naciye2 1. Department of Infectious Diseases and Clinical Microbiology, Ministry of Health Okmeydanı Training and Research Hospital, Istanbul 2. Department of Hematology, Ministry of Health Okmeydanı Training and Research Hospital, Istanbul Abstract: Background and objective: We evaluated the rates of vancomycin-resistant enterococci (VRE) colonization and VRE- related bacteremia in patients with hematological malignancies in terms of routine screening culture and its cost-effective- ness. Materials and Methods: All patients of the hematology department who were older than 14 years of age and who devel- oped at least one febrile neutropenia episode during chemotherapy for hematological cancers between November 2010 and November 2012 were evaluated retrospectively. Results: We retrospectively analyzed 282 febrile episodes in 126 neutropenic patients during a two-year study period. The study included 65 cases in the first study-year and 78 cases in the second study-year. The numbers of colonization days and colonized patient were748 days of colonization in 29 patients (44%) in the first study-year and 547 colonization days in 21 patients (26%) in the second study-year, respectively. Routine screening culture for VRE cost $4516,4 (427 cultures) in the first study-year, $5082,7 (504 cultures) in the second study-year depending on the number of patients and their length of stay. Conclusion: In line with our study results, routine screening of hematological patients for VRE colonization is not cost- effective. Routine surveillance culture for VRE should be considered with respect to the conditions of health care setting. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Curriculum Vitae
Wayne T. McCormack, Ph.D. CURRICULUM VITAE PERSONAL DATA Name: Wayne Thomas McCormack Address: Dept. of Pathology, Immunology & Laboratory Medicine University of Florida College of Medicine 1249 Center Drive Communicore Building, Room CG-72K Gainesville, Florida 32610-0208 Telephone: office (352) 294-8334 fax (352) 392-3053 E-Mail: [email protected] Website: http://mccormacklab.pathology.ufl.edu/ EDUCATION High School: Bellevue High School, Bellevue, Nebraska, 1976 Undergraduate: Creighton University, Omaha, Nebraska B.S. (Biology), December 15, 1979 Graduate: Florida State University, Tallahassee, Florida M.S., Biological Science (Genetics & Cell Biology), December 18, 1982 Ph.D., Biological Science (Genetics & Cell Biology), December 12, 1987 POSTDOCTORAL TRAINING Research Associate, Howard Hughes Medical Institute, University of Michigan Medical School, Ann Arbor, Michigan. November 1987 – February 1989 Postdoctoral Fellow, Dept. of Internal Medicine, University of Michigan Medical School, Ann Arbor, Michigan. March 1989 – August 1991 Master Educators of Medical Education, University of Florida College of Medicine. January 2001 – June 2002 AAMC Medical Education Research Certificate (MERC) Program. November 2008 – November 2010 ACADEMIC POSITIONS Distinguished Teaching Scholar & Professor, Dept. of Pathology, Immunology and Laboratory Medicine, Univ. Florida College of Medicine, July 2015 – present Associate Professor, Dept. of Pathology, Immunology and Laboratory Medicine, Univ. Florida College of Medicine, July 1997 – June 2015 Director, Clinical & Translational Science Predoctoral Training Programs, UF Clinical & Translational Science Institute, April 2009 – present Associate Dean for Graduate Education, Univ. Florida College of Medicine, September 2001 – February 2011 Assistant Professor, Dept. of Pathology, Immunology and Laboratory Medicine, Univ. Florida College of Medicine, June 1991 – June 1997 1 Wayne T. McCormack, Ph.D. -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

Neonatal Leukopenia and Thrombocytopenia
Neonatal Leukopenia and Thrombocytopenia Vandy Black, M.D., M.Sc., FAAP March 3, 2016 April 14, 2011 Objecves • Summarize the differenHal diagnosis of leukopenia and/or thrombocytopenia in a neonate • Describe the iniHal steps in the evaluaon of a neonate with leukopenia and/or thrombocytopenia • Review treatment opHons for leukopenia and/ or thrombocytopenia in the NICU Clinical Case 1 • One day old male infant admiUed to the NICU for hypoglycemia and a sepsis rule out • Born at 38 weeks EGA by SVD • Birth weight 4 lbs 13 oz • Exam shows a small cephalohematoma; no dysmorphic features • PLT count 42K with an otherwise normal CBC Definions • Normal WBC count 9-30K at birth – Mean 18K • What is the ANC and ALC – <1000/mm3 is abnormal – 6-8% of infants in the NICU • Normal platelet count: 150-450,000/mm3 – Not age dependent – 22-35% of infants in the NICU have plts<150K Neutropenia Absolute neutrophil count <1500/mm3 Category ANC* InfecHon risk • Mild 1000-1500 None • Moderate 500-1000 Minimal • Severe <500 Moderate to Severe (Highest if <200) • Recurrent bacterial or fungal infecHons are the hallmark of symptomac neutropenia! • *ANC = WBC X % (PMNs + Bands) / 100 DefiniHon of Neutropenia Black and Maheshwari, Neoreviews 2009 How to Approach Cytopenias • Normal vs. abnormal (consider severity) • Malignant vs. non-malignant • Congenital vs. acquired • Is the paent symptomac • Transient, recurrent, cyclic, or persistent How to Approach Cytopenias • Adequate vs. decreased marrow reserve • Decreased producHon vs. increased destrucHon/sequestraon Decreased neutrophil/platelet producon • Primary – Malignancy/leukemia/marrow infiltraon – AplasHc anemia – Genec disorders • Secondary – InfecHous – Drug-induced – NutriHonal • B12, folate, copper Increased destrucHon/sequestraon • Immune-mediated • Drug-induced • Consumpon à Hypersplenism vs. -

Enterococcal Bacteremia in Febrile Neutropenic Children and Adolescents with Underlying Malignancies, and Clinical Impact of Vancomycin Resistance
Infection (2019) 47:417–424 https://doi.org/10.1007/s15010-018-1260-z ORIGINAL PAPER Enterococcal bacteremia in febrile neutropenic children and adolescents with underlying malignancies, and clinical impact of vancomycin resistance Kil‑Seong Bae1,2 · Ju Ae Shin1 · Seong koo Kim1,3 · Seung Beom Han1,2 · Jae Wook Lee1,3 · Dong‑Gun Lee2,3,4 · Nack‑Gyun Chung1,3 · Bin Cho1,3 · Dae Chul Jeong1,2 · Jin Han Kang1,2 Received: 28 August 2018 / Accepted: 15 December 2018 / Published online: 19 December 2018 © Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Purpose Enterococci are a common cause of bacteremia in immunocompromised patients. Although the increase of van- comycin-resistant enterococci (VRE) makes appropriate antibiotic therapy difficult, clinical characteristics of enterococcal bacteremia and the impact of VRE infection on outcomes have rarely been reported in immunocompromised children. Methods We enrolled children and adolescents (< 19 years of age) with underlying malignancies who were diagnosed with enterococcal bacteremia during febrile neutropenia between 2010 and 2017. Medical records of the enrolled children were retrospectively reviewed to evaluate the clinical characteristics of enterococcal bacteremia and impact of VRE infection on outcomes. Results Thirty-six episodes of enterococcal bacteremia were identified in 30 patients. VRE infection was identified in 11 epi- sodes (30.6%); the 7- and 30-day mortalities were 27.8% and 44.4%, respectively. Acute lymphoblastic leukemia (50.0%) and acute myeloid leukemia (30.6%) were the most common underlying disorders. Three (8.3%) of the patients were in complete remission, and palliative and reinduction chemotherapies were administered in 47.2% and 36.1% of episodes, respectively.