Preclinical and Clinical Studies on LSD, Psilocybin, MDMA, and Ketamine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hallucinogens - LSD, Peyote, Psilocybin, and PCP
Hallucinogens - LSD, Peyote, Psilocybin, and PCP Hallucinogenic compounds found in some • Psilocybin (4-phosphoryloxy-N,N- plants and mushrooms (or their extracts) dimethyltryptamine) is obtained from have been used—mostly during religious certain types of mushrooms that are rituals—for centuries. Almost all indigenous to tropical and subtropical hallucinogens contain nitrogen and are regions of South America, Mexico, and classified as alkaloids. Many hallucinogens the United States. These mushrooms have chemical structures similar to those of typically contain less than 0.5 percent natural neurotransmitters (e.g., psilocybin plus trace amounts of acetylcholine-, serotonin-, or catecholamine- psilocin, another hallucinogenic like). While the exact mechanisms by which substance. hallucinogens exert their effects remain • PCP (phencyclidine) was developed in unclear, research suggests that these drugs the 1950s as an intravenous anesthetic. work, at least partially, by temporarily Its use has since been discontinued due interfering with neurotransmitter action or to serious adverse effects. by binding to their receptor sites. This DrugFacts will discuss four common types of How Are Hallucinogens Abused? hallucinogens: The very same characteristics that led to • LSD (d-lysergic acid diethylamide) is the incorporation of hallucinogens into one of the most potent mood-changing ritualistic or spiritual traditions have also chemicals. It was discovered in 1938 led to their propagation as drugs of abuse. and is manufactured from lysergic acid, Importantly, and unlike most other drugs, which is found in ergot, a fungus that the effects of hallucinogens are highly grows on rye and other grains. variable and unreliable, producing different • Peyote is a small, spineless cactus in effects in different people at different times. -

Hallucinogens - LSD, Peyote, Psilocybin, and PCP
Information for Behavioral Health Providers in Primary Care Hallucinogens - LSD, Peyote, Psilocybin, and PCP What are Hallucinogens? Hallucinogenic compounds found in some plants and mushrooms (or their extracts) have been used— mostly during religious rituals—for centuries. Almost all hallucinogens contain nitrogen and are classified as alkaloids. Many hallucinogens have chemical structures similar to those of natural neurotransmitters (e.g., acetylcholine-, serotonin-, or catecholamine-like). While the exact mechanisms by which hallucinogens exert their effects remain unclear, research suggests that these drugs work, at least partially, by temporarily interfering with neurotransmitter action or by binding to their receptor sites. This InfoFacts will discuss four common types of hallucinogens: LSD (d-lysergic acid diethylamide) is one of the most potent mood-changing chemicals. It was discovered in 1938 and is manufactured from lysergic acid, which is found in ergot, a fungus that grows on rye and other grains. Peyote is a small, spineless cactus in which the principal active ingredient is mescaline. This plant has been used by natives in northern Mexico and the southwestern United States as a part of religious ceremonies. Mescaline can also be produced through chemical synthesis. Psilocybin (4-phosphoryloxy-N, N-dimethyltryptamine) is obtained from certain types of mushrooms that are indigenous to tropical and subtropical regions of South America, Mexico, and the United States. These mushrooms typically contain less than 0.5 percent psilocybin plus trace amounts of psilocin, another hallucinogenic substance. PCP (phencyclidine) was developed in the 1950s as an intravenous anesthetic. Its use has since been discontinued due to serious adverse effects. How Are Hallucinogens Abused? The very same characteristics that led to the incorporation of hallucinogens into ritualistic or spiritual traditions have also led to their propagation as drugs of abuse. -

Design and Synthesis of Cyclic Analogs of the Kappa Opioid Receptor Antagonist Arodyn
Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn By © 2018 Solomon Aguta Gisemba Submitted to the graduate degree program in Medicinal Chemistry and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Dr. Michael Rafferty Dr. Teruna Siahaan Dr. Thomas Tolbert Date Defended: 18 April 2018 The dissertation committee for Solomon Aguta Gisemba certifies that this is the approved version of the following dissertation: Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Date Approved: 10 June 2018 ii Abstract Opioid receptors are important therapeutic targets for mood disorders and pain. Kappa opioid receptor (KOR) antagonists have recently shown potential for treating drug addiction and 1,2,3 4 8 depression. Arodyn (Ac[Phe ,Arg ,D-Ala ]Dyn A(1-11)-NH2), an acetylated dynorphin A (Dyn A) analog, has demonstrated potent and selective KOR antagonism, but can be rapidly metabolized by proteases. Cyclization of arodyn could enhance metabolic stability and potentially stabilize the bioactive conformation to give potent and selective analogs. Accordingly, novel cyclization strategies utilizing ring closing metathesis (RCM) were pursued. However, side reactions involving olefin isomerization of O-allyl groups limited the scope of the RCM reactions, and their use to explore structure-activity relationships of aromatic residues. Here we developed synthetic methodology in a model dipeptide study to facilitate RCM involving Tyr(All) residues. Optimized conditions that included microwave heating and the use of isomerization suppressants were applied to the synthesis of cyclic arodyn analogs. -

Radial Glia Reveal Complex Regulation by the Neuropeptide Secretoneurin
Transcriptomic and proteomic characterizations of goldfish (Carassius auratus) radial glia reveal complex regulation by the neuropeptide secretoneurin Dillon Da Fonte Thesis submitted to the Faculty of Graduate and Postdoctoral Studies University of Ottawa in partial fulfillment of the requirements for the Master of Science degree in biology Department of Biology Faculty of Science University of Ottawa © Dillon Da Fonte, Ottawa, Canada, 2016 Acknowledgements Finishing this thesis has been both a challenging and rewarding experience. This accomplishment would not have been possible without the never-ending support of colleagues, friends, family. First, I would like to express my most sincere gratitude to my supervisor and mentor, Dr. Vance Trudeau. Thank you for the opportunities you have given me, this experience has truly solidified my passion for research. I appreciate our many conversations that were enjoyed over a beer – it was truly a memorable experience. I would also like to thank my M.Sc. advisory committee, Dr. Michael Jonz and Dr. Marc Ekker for your time and insightful comments. A special thank you to Dr. Chris Martynuik who taught me the bioinformatics needed to analyze both transcriptomic and proteomic data and for all your help during my time at the University of Florida. I would like to also acknowledge my funding support from University of Ottawa, NSERC, and the Michael Smith Foreign Study Award for supporting my research stay at the University of Florida. To all current and past members of TeamENDO, thank you for the sense of community you all instilled in the lab. Both inside and outside the lab, I have made memories with all of you that I will cherish forever. -

SPRAVATO® Esketamine Hydrochloride DATA SHEET
SPRAVATO® esketamine hydrochloride DATA SHEET 1. PRODUCT NAME SPRAVATO® esketamine hydrochloride 32.3mg (equivalent to 28mg esketamine) nasal spray 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each single use nasal spray device delivers two sprays, one spray into each nostril. Total volume of drug product per device to be delivered is 0.2 mL containing a total of 32.3 mg of esketamine hydrochloride (equivalent to 28 mg of esketamine). For the full list of excipients, see Section 6.1 List of Excipients. 3. PHARMACEUTICAL FORM Nasal spray, solution. Clear, colourless, aqueous solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications SPRAVATO in conjunction with an oral antidepressant, is indicated for: - treatment resistant depression (Major Depressive Disorder in adults who have not responded adequately to at least two different antidepressants of adequate dose and duration to treat the current depressive episode). - rapid reduction of depressive symptoms in patients with Major Depressive Disorder who have acute suicidal ideation or behaviour. SPRAVATO is not indicated to prevent suicide or in reducing suicidal ideation or behaviour (see section 4.4. Special Warnings And Precautions For Use) 4.2 Dose and method of administration In patients with TRD, SPRAVATO should be administered in conjunction with a newly initiated oral antidepressant (AD) therapy. In patients with MDSI, SPRAVATO should be administered in conjunction with standard of care therapy. During the Phase III MDSI clinical program, standard of care oral AD treatment (either AD monotherapy or AD plus augmentation therapy) was initiated or optimised. Important Considerations Prior to Initiating and During Therapy SPRAVATO must be administered under the direct supervision of a healthcare provider. -

Around the Corner Canadian Equity Research Emerging Companies and Industries to Watch 3 March 2020
Around the Corner Canadian Equity Research Emerging companies and industries to watch 3 March 2020 Tania Gonsalves, CFA | Analyst | Canaccord Genuity Corp. (Canada) | [email protected] | 1.416.996.8346 Scott McFarland | Associate | Canaccord Genuity Corp. (Canada) | [email protected] | 1.416.998.7202 Around the Corner highlights what we believe are some of the most exciting Psychedelic-derived medicines and therapies emergent private companies in Canada, and/or industry themes and trends which are yet to be fully represented in the Mental health miracle or another bad trip? public markets. When most of us think of psychedelic drugs, we think of the 1960s counterculture. We We aim to offer insight into early industry think of anti-establishment, anti-war, anti-capitalist hippies, Woodstock, tie-dye, Lucy in trends, educate investors about private the Sky, peace, love and bell bottom jeans. But before psychedelics became ingrained in companies that are making a mark, and the counterculture, they were found in a lab. The first wave of scientific research on identify companies that may enter the psychedelics took place between 1950-65. Sandoz Pharmaceutics, what is now Novartis public markets in the future. AG (NVS-NYSE), the third largest pharmaceutical company in the world, used to market We do not provide any ratings or price LSD and psilocybin for psychotherapeutic purposes. Psychedelics weren’t born of the targets, nor should any be inferred, for counterculture. They were killed by it. The proliferation of recreational use spurred any uncovered company featured in government intervention and by 1971, psilocybin, LSD, ibogaine, mescaline, peyote, Around the Corner. -

Psilocybin Mushrooms Fact Sheet
Psilocybin Mushrooms Fact Sheet January 2017 What are psilocybin, or “magic,” mushrooms? For the next two decades thousands of doses of psilocybin were administered in clinical experiments. Psilocybin is the main ingredient found in several types Psychiatrists, scientists and mental health of psychoactive mushrooms, making it perhaps the professionals considered psychedelics like psilocybin i best-known naturally-occurring psychedelic drug. to be promising treatments as an aid to therapy for a Although psilocybin is considered active at doses broad range of psychiatric diagnoses, including around 3-4 mg, a common dose used in clinical alcoholism, schizophrenia, autism spectrum disorders, ii,iii,iv research settings ranges from 14-30 mg. Its obsessive-compulsive disorder, and depression.xiii effects on the brain are attributed to its active Many more people were also introduced to psilocybin metabolite, psilocin. Psilocybin is most commonly mushrooms and other psychedelics as part of various found in wild or homegrown mushrooms and sold religious or spiritual practices, for mental and either fresh or dried. The most popular species of emotional exploration, or to enhance wellness and psilocybin mushrooms is Psilocybe cubensis, which is creativity.xiv usually taken orally either by eating dried caps and stems or steeped in hot water and drunk as a tea, with Despite this long history and ongoing research into its v a common dose around 1-2.5 grams. therapeutic and medical benefits,xv since 1970 psilocybin and psilocin have been listed in Schedule I of the Controlled Substances Act, the most heavily Scientists and mental health professionals criminalized category for drugs considered to have a consider psychedelics like psilocybin to be “high potential for abuse” and no currently accepted promising treatments as an aid to therapy for a medical use – though when it comes to psilocybin broad range of psychiatric diagnoses. -

Estrogen Receptor (ER) Expression and Function in the Pregnant Human Myometrium: Estradiol Via Era Activates ERK1/2 Signaling in Term Myometrium
227 Estrogen receptor (ER) expression and function in the pregnant human myometrium: estradiol via ERa activates ERK1/2 signaling in term myometrium Toni Welsh1,2, Matrika Johnson1, Lijuan Yi1, Huiqing Tan1, Roksana Rahman1, Amy Merlino1, Tamas Zakar2,3 and Sam Mesiano1 1Department of Reproductive Biology, Case Western Reserve University, 11100 Euclid Avenue, Cleveland, Ohio 44106, USA 2Mothers and Babies Research Centre, University of Newcastle, Newcastle, New South Wales 2308, Australia 3Department of Obstetrics and Gynaecology, John Hunter Hospital, Newcastle, New South Wales 2305, Australia (Correspondence should be addressed to S Mesiano; Email: [email protected]) Abstract Estrogens are thought to promote labor by increasing inhibition of 26S proteasome activity increased ERa protein the expression of pro-contraction genes in myometrial cells. abundance to detectable levels in term myometrial explants, The specific estrogen receptors ((ERs: ERa and ERb (also however, indicating rapid turnover of ERa protein by known as ESR1 and ESR2)) and G protein-coupled receptor proteasomal processing in the pregnant myometrium. E2 30 (GPR30; also known as G protein-coupled estrogen stimulated rapid extranuclear signaling in myometrial explants, receptor 1)) and signaling pathways that mediate these actions as evidenced by increased extracellularly regulated kinase are not clearly understood. In this study, we identified the ERs (ERK1/2) phosphorylation within 10 min. This effect was expressed in the pregnant human myometrium and determined inhibited by pre-treatment with an ER antagonist, ICI a key extranuclear signaling pathway through which estradiol 182 780, indicating the involvement of ERa. Inhibition of (E2) modulates expression of the gene encoding the oxytocin ERK signaling abrogated the ability of E2 to stimulate OXTR receptor (OXTR), a major pro-contraction protein. -

The Oxytocin/Vasopressin Receptor Family Has at Least Five Members in the Gnathostome Lineage, Including Two Distinct V2 Subtypes
The oxytocin/vasopressin receptor family has at least five members in the gnathostome lineage, including two distinct V2 subtypes General and Comparative Endocrinology 175(1): 135-143 doi:10.1016/j.ygcen.2011.10.011 Accepted October 20, 2011 E-pub October 28, 2012 Published January 1, 2012 Figshare doi:10.6084/m9.figshare.811860. Shared October 1, 2013 Daniel Ocampo Daza*, Michalina Lewicka¹, Dan Larhammar Department of Neuroscience, Science for Life Laboratory, Uppsala Universitet, Box 593, SE-751 24 Uppsala, Sweden * Corresponding author. E-mail address: [email protected] ¹ Current address: Department of Neuroscience, Karolinska Institutet, SE-171 77 Stockholm, Sweden Cite as D. Ocampo Daza, M. Lewicka and D. Larhammar. The oxytocin/vasopressin family has at least five members in the gnathostome lineage, including two distinct V2 subtypes. General and Comparative Endocrinology, 175 (1) (2012) 135-143. This document corresponds to the article as it appeared upon acceptance. You are free to download, print and distribute it for any purposes under a Creative Commons Attribution 3.0 Unported License (http://creativecommons.org/licenses/by/3.0/), provided the original work is cited as specified. Errata: The introduction incorrectly states that “the V2 receptor inhibits adenylyl cyclase, thereby reducing the production of cAMP” on page 3. In fact the V2-type vasopressin receptors stimulate adenylyl cyclase and increase the cytosolic cyclic AMP release, see for instance Schöneberg et al., Molecular aspects of vasopressin receptor function, Advances in experimental medicine and biology 449 (1998) 347–58. This mistake was reported in the proofreading phase of pre-publication, but the correction was not carried to the final version of the article. -
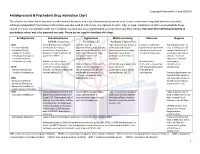
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

G Protein-Coupled Receptors: What a Difference a ‘Partner’ Makes
Int. J. Mol. Sci. 2014, 15, 1112-1142; doi:10.3390/ijms15011112 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review G Protein-Coupled Receptors: What a Difference a ‘Partner’ Makes Benoît T. Roux 1 and Graeme S. Cottrell 2,* 1 Department of Pharmacy and Pharmacology, University of Bath, Bath BA2 7AY, UK; E-Mail: [email protected] 2 Reading School of Pharmacy, University of Reading, Reading RG6 6UB, UK * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +44-118-378-7027; Fax: +44-118-378-4703. Received: 4 December 2013; in revised form: 20 December 2013 / Accepted: 8 January 2014 / Published: 16 January 2014 Abstract: G protein-coupled receptors (GPCRs) are important cell signaling mediators, involved in essential physiological processes. GPCRs respond to a wide variety of ligands from light to large macromolecules, including hormones and small peptides. Unfortunately, mutations and dysregulation of GPCRs that induce a loss of function or alter expression can lead to disorders that are sometimes lethal. Therefore, the expression, trafficking, signaling and desensitization of GPCRs must be tightly regulated by different cellular systems to prevent disease. Although there is substantial knowledge regarding the mechanisms that regulate the desensitization and down-regulation of GPCRs, less is known about the mechanisms that regulate the trafficking and cell-surface expression of newly synthesized GPCRs. More recently, there is accumulating evidence that suggests certain GPCRs are able to interact with specific proteins that can completely change their fate and function. These interactions add on another level of regulation and flexibility between different tissue/cell-types. -

Janssen Research & Development, LLC Advisory Committee Briefing
Janssen Research & Development, LLC Advisory Committee Briefing Document Esketamine Nasal Spray for Patients with Treatment-resistant Depression JNJ-54135419 (esketamine) Status: Approved Date: 16 January 2019 Prepared by: Janssen Research & Development, LLC EDMS number: EDMS-ERI-171521650, 1.0 ADVISORY COMMITTEE BRIEFING MATERIALS: AVAILABLE FOR PUBLIC RELEASE 1 Status: Approved, Date: 16 January 2019 JNJ-54135419 (esketamine) Treatment-resistant Depression Advisory Committee Briefing Document GUIDE FOR REVIEWERS This briefing document provides 3 levels of review with increasing levels of detail: The Executive Overview (Section 1, starting on page 11) provides a narrative summarizing the disease, need for novel treatments, key development program characteristics for esketamine nasal spray, study results, and conclusions. References are made to the respective supporting sections in the core document. The core document (Section 2 to Section 11, starting on page 30) includes detailed summaries and discussion in support of the Executive Overview. The appendices (starting on page 180) provide additional or more detailed information to complement brief descriptions provided in sections of the core document (e.g., demographic and baseline characteristics of the study populations, additional efficacy analyses in the Phase 3 studies, statistical methods). These appendices are referenced in the core document when relevant. This review structure allows review at varying levels of detail; however, reviewers who read at multiple levels will necessarily