Breastfeeding Management for the Clinician: Using the Evidence, Second Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Approach to the Treatment of Gynecomastia According to Its Classification
ARTIGO ORIGINAL Abordagem cirúrgica para o tratamentoVendraminFranco da T ginecomastia FSet al.et al. conforme sua classificação Abordagem cirúrgica para o tratamento da ginecomastia conforme sua classificação Surgical approach to the treatment of gynecomastia according to its classification MÁRIO MÚCIO MAIA DE RESUMO MEDEIROS1 Introdução: A ginecomastia é a proliferação benigna mais comum do tecido glandular da mama masculina, causada pela alteração do equilíbrio entre as concentrações de estrógeno e andrógeno. Na maioria dos casos, o principal tratamento é a cirurgia. O objetivo deste tra- balho foi demonstrar a aplicabilidade das técnicas cirúrgicas consagradas para a correção da ginecomastia, de acordo com a classificação de Simon, e apresentar uma nova contribuição. Método: Este trabalho foi realizado no período de março de 2009 a março de 2011, sendo incluídos 32 pacientes do sexo masculino, com idades entre 13 anos e 45 anos. A escolha da incisão foi relacionada à necessidade ou não de ressecção de pele. Foram utilizadas quatro técnicas da literatura e uma modificação da técnica por incisão circular com prolongamentos inferior, superior, lateral e medial, quando havia excesso de pele também no polo inferior da mama. Resultados: A principal causa da ginecomastia identificada entre os pacientes foi idiopática, seguida pela obesidade e pelo uso de esteroides anabolizantes. Conclusões: A técnica mais utilizada foi a incisão periareolar inferior proposta por Webster, quando não houve necessidade de ressecção de pele. Na presença de excesso de pele, a técnica escolhi- da variou de acordo com a quantidade do tecido a ser ressecado. A nova técnica proposta permitiu maior remoção do tecido dermocutâneo glandular e gorduroso da mama, quando comparada às demais técnicas utilizadas na experiência do cirurgião. -

Tongue and Lip Ties: Best Evidence June 16, 2015
Tongue and Lip Ties: Best Evidence June 16, 2015 limited elevation in tongue tied baby Tongue and Lip Ties: Best Evidence By: Lee-Ann Grenier Tongue and lip tie (often abbreviated to TT/LT) have become buzzwords among lactation consultants bloggers and new mothers. For many these are strange new words despite the fact that it is a relatively common condition. Treating tongue tie fell out of medical favour in the early 1950s. In breastfeeding circles, it was talked about occasionally, but until recently few health care professionals screened babies for tongue tie and it was frequently overlooked as a cause of common breastfeeding difficulties. In the last few years tongue tie and the related condition lip tie have exploded into the consciousness of mothers and breastfeeding helpers. So why all the fuss about tongue and lip ties all of a sudden? Tongue tie seems to be a relatively common problem, affecting 4-11%1 of the population and it can have a drastic impact on breastfeeding. The presence of tongue tie triples the risk of weaning in the first week of life.2 Here in Alberta it has been challenging to find competent assessment and treatment, prompting several Alberta mothers and their babies to fly to New York in 2011 and 2012 to receive treatment. The dedication and persistence of these mothers has spurred action on providing education and treatment options for Alberta families. In August of 2012, The Breastfeeding Action Committee of Edmonton (BACE) brought Dr. Lawrence Kotlow to Edmonton to provide information and training to area health care providers. -

The Ins and Outs of Inverted Nipple Repair
The Ins and Outs of Inverted Nipple Repair plasticsurgerypractice.com/2009/11/the-ins-and-outs-of-inverted-nipple-repair/ The proper appearance of the breast and the nipple can be very important to women and men alike. An inverted nipple, something that women may notice increasing at the onset of puberty, is something that can be rectified with a simple 15-minute surgical procedure. PSP recently spoke with M. Mark Mofid, MD, FACS, a plastic surgeon in La Jolla, Calif, about the various techniques of inverted nipple surgery as well as nipple reduction. Mofid is a staff surgeon at several California hospitals, including Scripps Memorial Hospital in La Jolla, Palomar Medical Center in Escondido, and Sharp Chula Vista Medical Center. In addition, he serves on the clinical faculty of the University of California, San Diego, Division of Plastic Surgery. He earned his undergraduate degree magna cum laude from Harvard University. He then attended The Johns Hopkins University School of Medicine, where he completed his medical degree training in general surgery and plastic surgery, and well as completed an advanced craniofacial research fellowship. PSP: How new is the inverted nipple procedure, and how popular is it? Mofid: Numerous techniques have been described over the last several decades for inverted nipple repair. In my own practice, at least one to two patients per month request this procedure. PSP: Are there different types of inverted nipple surgery and different ways of performing the surgery? Mofid: Virtually all techniques involve some variation of a release of the nipple from its basilar attachments. Fixation (whether internal or external) prevents the nipple from re-retracting during the healing process. -
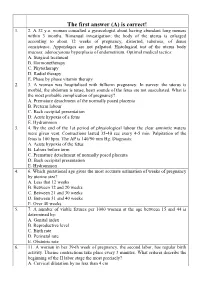
The First Answer (A) Is Correct! 1
The first answer (A) is correct! 1. 2. A 32 y.o. woman consulted a gynecologist about having abundant long menses within 3 months. Bimanual investigation: the body of the uterus is enlarged according to about 12 weeks of pregnancy, distorted, tuberous, of dense consistence. Appendages are not palpated. Histological test of the uterus body mucosa: adenocystous hyperplasia of endometrium. Optimal medical tactics: A. Surgical treatment B. Hormonetherapy C. Phytotherapy D. Radial therapy E. Phase by phase vitamin therapy 2. 3. A woman was hospitalised with fullterm pregnancy. In survey: the uterus is morbid, the abdomen is tense, heart sounds of the fetus are not auscultated. What is the most probable complication of pregnancy? A. Premature detachment of the normally posed placenta B. Preterm labour C. Back occipital presentation D. Acute hypoxia of a fetus E. Hydramnion 3. 4. By the end of the 1st period of physiological labour the clear amniotic waters were given vent. Contractions lasted 35-40 sec every 4-5 min. Palpitation of the fetus is 100 bpm. The AP is 140/90 mm Hg. Diagnosis: A. Acute hypoxia of the fetus B. Labors before term C. Premature detachment of normally posed placenta D. Back occipital presentation E. Hydramnion 4. 6. Which gestational age gives the most accurate estimation of weeks of pregnancy by uterine size? A. Less that 12 weeks B. Between 12 and 20 weeks C. Between 21 and 30 weeks D. Between 31 and 40 weeks E. Over 40 weeks 5. 7. A number of viable fetuses per 1000 women at the age between 15 and 44 is determined by: A. -

Breast Concerns
Section 12.0: Preventive Health Services for Women Clinical Protocol Manual 12.2 BREAST CONCERNS TITLE DESCRIPTION DEFINITION: Breast concerns in women of all ages are often the source of significant fear and anxiety. These concerns can take the form of palpable masses or changes in breast contours, skin or nipple changes, congenital malformation, nipple discharge, or breast pain (cyclical and non-cyclical). 1. Palpable breast masses may represent cysts, fibroadenomas or cancer. a. Cysts are fluid-filled masses that can be found in women of all ages, and frequently develop due to hormonal fluctuation. They often change in relation to the menstrual cycle. b. Fibroadenomas are benign sold tumors that are caused by abnormal growth of the fibrous and ductal tissue of the breast. More common in adolescence or early twenties but can occur at any age. A fibroadenoma may grow progressively, remain the same, or regress. c. Masses that are due to cancer are generally distinct solid masses. They may also be merely thickened areas of the breast or exaggerated lumpiness or nodularity. It is impossible to diagnose the etiology of a breast mass based on physical exam alone. Failure to diagnose breast cancer in a timely manner is the most common reason for malpractice litigation in the U.S. Skin or nipple changes may be visible signs of an underlying breast cancer. These are danger signs and require MD referral. 2. Non-spontaneous or physiological discharge is fluid that may be expressed from the breast and is not unusual in healthy women. 3. Galactorrhea is a spontaneous, multiple duct, milky discharge most commonly found in non-lactating women during childbearing years. -

Human Anatomy As Related to Tumor Formation Book Four
SEER Program Self Instructional Manual for Cancer Registrars Human Anatomy as Related to Tumor Formation Book Four Second Edition U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutesof Health SEER PROGRAM SELF-INSTRUCTIONAL MANUAL FOR CANCER REGISTRARS Book 4 - Human Anatomy as Related to Tumor Formation Second Edition Prepared by: SEER Program Cancer Statistics Branch National Cancer Institute Editor in Chief: Evelyn M. Shambaugh, M.A., CTR Cancer Statistics Branch National Cancer Institute Assisted by Self-Instructional Manual Committee: Dr. Robert F. Ryan, Emeritus Professor of Surgery Tulane University School of Medicine New Orleans, Louisiana Mildred A. Weiss Los Angeles, California Mary A. Kruse Bethesda, Maryland Jean Cicero, ART, CTR Health Data Systems Professional Services Riverdale, Maryland Pat Kenny Medical Illustrator for Division of Research Services National Institutes of Health CONTENTS BOOK 4: HUMAN ANATOMY AS RELATED TO TUMOR FORMATION Page Section A--Objectives and Content of Book 4 ............................... 1 Section B--Terms Used to Indicate Body Location and Position .................. 5 Section C--The Integumentary System ..................................... 19 Section D--The Lymphatic System ....................................... 51 Section E--The Cardiovascular System ..................................... 97 Section F--The Respiratory System ....................................... 129 Section G--The Digestive System ......................................... 163 Section -

Open Dissertation FINAL.Pdf
The Pennsylvania State University The Graduate School College of Education “I SAW A WRONG AND I WANTED TO STAND UP FOR WHAT I THOUGHT WAS RIGHT:” A NARRATIVE STUDY ON BECOMING A BREASTFEEDING ACTIVIST A Dissertation in Adult Education by Jennifer L. Pemberton © 2016 Jennifer L. Pemberton Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Education May 2016 ii The dissertation of Jennifer L. Pemberton was reviewed and approved* by the following: Elizabeth J. Tisdell Professor of Adult Education Dissertation Adviser Chair of Committee Doctoral Program Coordinator Robin Redmon Wright Assistant Professor of Adult Education Ann Swartz Senior Lecturer, RN-BS Program Janet Fogg Assistant Professor of Nursing Hershey Coordinator *Signatures are on file in the Graduate School. iii ABSTRACT The purpose of this narrative study was two-fold: (a) to examine how breastfeeding mothers learn they are members of a marginalized group; and (b) to investigate how some of these mothers move from marginalization to activism. This study was grounded in two interconnected theoretical frameworks: critical feminism (also with attention to embodied learning) and women’s emancipatory learning in relation to breastfeeding and activism. There were 11 participants in the study, chosen according to purposeful criteria related to the study’s purpose; they represent diversity in age, race/ethnicity, sexual orientation, religion, and educational background. Data collection included narrative semi-structured interviews, which were co-constructed between the researcher and the participants, and researcher-generated artifacts. Both narrative and constant-comparative analysis were used to analyze the data. There were three sets of findings that emerged from the data. -

Benign Breast Diseases1
BENIGN BREAST DISEASES PROFFESOR.S.FLORET NORMAL STRUCTURE DEVELOPMENTAL/CONGENITAL • Polythelia • Polymastia • Athelia • Amastia ‐ poland syndrome • Nipple inversion • Nipple retraction • NON‐BREAST DISORDERS • Tietze disease • Sebaceous cyst & other skin disorders. • Monder’s disease BENIGN DISEASE OF BREAST • Fibroadenoma • Fibroadenosis‐ ANDI • Duct ectasia • Periductal papilloma • Infective conditions‐ Mastitis ‐ Breast abscess ‐ Antibioma ‐ Retromammary abscess Trauma –fat necrosis. NIPPLE INVERSION • Congenital abnormality • 20% of women • Bilateral • Creates problem during breast feeding • Cosmetic surgery does not yield normal protuberant nipple. NIPPLE INVERSION NIPPLE RETRACTION • Nipple retraction is a secondary phenomenon due to • Duct ectasia‐ bilateral nipple retarction. • Past surgery • Carcinoma‐ short history,unilateral,palpable mass. NIPPLE RETRACTION ABERRATIONS OF NORMAL DEVELOPMENT AND INVOLUTION (ANDI) • Breast : Physiological dynamic structure. ‐ changes seen throught the life. • They are ‐ developmental & involutional ‐ cyclical & associated with pregnancy and lactation. • The above changes are described under ANDI. PATHOLOGY • The five basic pathological features are: • Cyst formation • Adenosis:increase in glandular issue • Fibrosis • Epitheliosis:proliferation of epithelium lining the ducts & acini. • Papillomatosis:formation of papillomas due to extensive epithelial hyperplasia. ANDI & CARCINOMA • NO RISK: • Mild hyperplasia • Duct ectasia. • SLIGHT INCREASED RISK(1.5‐2TIMES): • Moderate hyperplasia • Papilloma -

Breastfeeding After Breast Surgery-V3-Formatted
Breastfeeding After Breast and Nipple Surgeries: A Guide for Healthcare Professionals By Diana West, BA, IBCLC, RLC PURPOSE A satisfying breastfeeding relationship is not precluded by insufficient milk production. When measures are taken to protect the milk supply that exists, minimize supplementation, The purpose of this guide is to provide the healthcare and increase milk production when possible, a mother with professional with an understanding of breast and nipple compromised milk production can have a satisfying surgeries and their effects upon lactation and the breastfeeding relationship with her baby. breastfeeding relationship. The effect of breast and nipple surgery upon lactation functionality and breastfeeding dynamics varies according to the type of surgery performed. This guide has delineated discussion of breastfeeding after PREDICTING LACTATION breast and nipple surgeries according to the three broad CAPABILITY AFTER BREAST AND categories: diagnostic, ablative, and therapeutic breast procedures, cosmetic breast surgeries, and nipple surgeries. NIPPLE SURGERIES The reasons, motivations, issues, concerns, stresses, and physical and psychological results share some The aspect of breast and nipple surgeries that is most likely to commonalities, but are largely unique to the type of surgery affect lactation is the surgical treatment of the areola and performed. For this reason, each type of surgery and its nipple. The location, orientation, and length of the incision effect upon lactation will be discussed independently. directly affect lactation capability by severing the parenchyma Methods to assess milk production and an overview of and innervation to the nipple/areolar complex. An incision feeding options to maximize milk production when near or on the areola, particularly in the lower, outer quadrant supplementation is necessary are presented. -

Breast Uplift (Mastopexy) Procedure Aim and Information
Breast Uplift (Mastopexy) Procedure Aim and Information Mastopexy (Breast Uplift) The breast is made up of fat and glandular tissue covered with skin. Breasts may change with variable influences from hormones, weight change, pregnancy, and gravitational effects on the breast tissue. Firm breasts often have more glandular tissue and a tighter skin envelope. Breasts become softer with age because the glandular tissue gradually makes way for fatty tissue and the skin also becomes less firm. Age, gravity, weight loss and pregnancy may also influence the shape of the breasts causing ptosis (sagging). Sagging often involves loss of tissue in the upper part of the breasts, loss of the round shape of the breast to a more tubular shape and a downward migration of the nipple and areola (dark area around the nipple). A mastopexy (breast uplift) may be performed to correct sagging changes in the breast by any one or all of the following methods: 1. Elevating the nipple and areola 2. Increasing projection of the breast 3. Creating a more pleasing shape to the breast Mastopexy is an elective surgical operation and it typifies the trade-offs involved in plastic surgery. The breast is nearly always improved in shape, but at the cost of scars on the breast itself. A number of different types of breast uplift operations are available to correct various degrees of sagginess. Small degrees of sagginess can be corrected with a breast enlargement (augmentation) only if an increase in breast size is desirable, or with a scar just around the nipple with or without augmentation. -

Phd Thesis Summary
University of Medicine and Pharmacy of Craiova DOCTORAL SCHOOL PhD Thesis BREAST RECONSTRUCTION AFTER SURGERY FOR BREAST HIPERTROPHY AND BENIGN TUMORS Summary Ph.D. SUPERVISOR: Prof. univ. dr. Mihai Brăila Ph.D. CANDIDATE: Radu Claudiu Gabriel CRAIOVA 2013 INTRODUCTION According to statistics, only in the United States in 2012 over 14 million cosmetic surgery of the breasts were made, but only about 3% of these were for surgical breast reconstruction after mastectomy as an interventional oncology treatment, although about 300,000 women are diagnosed each year with mammary tumors and most of them suffer breast surgery that can vary from partial, segmental or total removal of the breast. This creates a major gap between the number of surgeons able to successfully carry out such intervention and the number of patients who would require them, making obvious the need to increase the number of professionals that are able to perform breast reconstruction after mastectomy, especially the aesthetic mastectomy in people diagnosed with breast hypertrophy. Based on medical literature data, in this study we aimed to elucidate, using specific research methods, the impact of clinical and psychological intervention of breast reconstruction in patients suffering from breast hypertrophy and benign tumors. We hope that our study will shade some light on the need of brest reconstruction, its impact on specific pathology (mammary hypertrophy and benign tumors) and to contribut in improving breast reconstruction techniques that can help to avoid any complication that may arise. CHAPTER I Functional anatomy of the mammary gland Adult female mammary gland is located on both side of the anterior chest having it's base stretching from about the second to the sixth rib. -

CASE REPORT Severe Gynaecomastia Associated with Highly Active Antiretroviral Therapy Faith C
Open Access CASE REPORT Severe gynaecomastia associated with highly active antiretroviral therapy Faith C. Muchemwa1,2, Clarice T. Madziyire2 1. Department of Surgery, College of Health Sciences, University of Zimbabwe, Harare, Zimbabwe 2. Department of Immunology, College of Health Sciences, University of Zimbabwe, Harare, Zimbabwe Correspondence: Dr Faith C. Muchemwa ([email protected]) © 2018 F.C. Muchemwa & C.T. Madziyire. This open access article is licensed under a Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), East Cent Afr J Surg. 2018 Aug;23(2):80–82 which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. https://dx.doi.org/10.4314/ecajs.v23i2.6 Abstract The association between gynaecomastia and HIV infection was first reported in 1987; however, there were no subsequent pub- lished reports of gynaecomastia linked to HIV infection until highly active antiretroviral therapy (HAART) was introduced. Although HAART significantly improves the prognosis of HIV infection, its extensive use has resulted in multiple adverse effects, including benign breast enlargement. We present a rare case of severe gynaecomastia in a male patient with vertically transmitted HIV on HAART. He was surgically treated with mastectomy with no nipple-areolar complex reconstruction. The pathology report con- firmed the benign nature of the breast tissue. Surgical intervention resulted in an improvement of daily activities and enhanced psychosocial wellbeing. Benign bilateral breast enlargement of this magnitude in a male patient has never been reported.