Genetic Prothrombotic Mutations Are Common in Neonates but Are Not Associated with Umbilical Catheter-Associated Thrombosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Nursing Care of Neonatal Central Lines Presented for Thames Valley & Wessex Neonatal ODN Governance Group Approval on Date of Ratified by Governance Publication
Thames Valley & Wessex Operational Delivery Networks (Hosted by University Hospital Southampton NHS Foundation Trust) THAMES VALLEY & WESSEX NEONATAL OPERATIONAL DELIVERY NETWORK Nursing Care of Neonatal Central Lines Presented for Thames Valley & Wessex Neonatal ODN Governance Group approval on Date of Ratified by Governance publication Last Reviewed New Sept 2019- Final Draft Review date (Max December 2022 3 years) Authors Thames Valley Neonatal OD Network, Quality Care Group. Distribution Thames Valley and Wessex Lead Nurses and Practice Educator Group. Thames Valley and Wessex Neonatal Clinical Forums Thames Valley and Wessex Neonatal Network website Thames Valley and Wessex Neonatal Network e-bulletin Related References. documents AHRQ (2019) Agency for Healthcare Research and Quality. Found at; https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/education/curriculum- tools/clabsitools/clabsitools.pdf Ansary.A (2019) Arterial Line analysis. ICU Professor, Ain Shams, Cairo. Egypt. Found at; https://www.slideshare.net/samirelansary/arterial-line-analysis-46584416 BAPM (2015) Use of Central Venous Catheters and Neonates. A framework for practice. Revised Aug 2018. British Association of Perinatal Medicine. Berry et al (2017) Extravasation and Infiltration, Great Ormond Street Hospital, Found at; www.gosh.nhs.uk Charge Nurse (2006) Intravascular catheters, Doule and triple Lumen catheters, Administration of drugs and sterilisation of longlines/CVL using antibiotics. Newborn Services Clinical Guideline Found at www.adhb.govt.nz/newborn Clarkston. R (2018) Arterial waveform analysis. @Insight health data science. Found at http://www.rebeccaclarkson.com/blog/artform/ Chapman. S (2015) Infection prevention and Central venous Catheters: Evidence round up. Found at http://www.evidentlycochrane.net/infection-prevention-and-central-venous-catheters- evidence-round-up/ Collins.E (2018) Nursing guideline for care of a Hickman line. -

Umbilical Venous and Arterial Catheters
HALO 10 ....Anthelio ICD-10 ExpressLearn ICD-10-PCS: Umbilical Venous Catheters and Umbilical Arterial Catheters December 16, 2014 Vol. 2 Umbilical Venous Catheters Umbilical Arterial Catheters • Umbilical vein catheterization (UVC) may be a life-saving procedure in • Umbilical artery catheterization is a common procedure in the neonates who require vascular access and resuscitation. The umbilical neonatal intensive care unit and has become the standard of care for vein remains patent and viable for cannulation until approximately 1 arterial access in neonates. The umbilical artery can be used for week after birth. After proper placement of the umbilical line, arterial access during the first 5-7 days of life, but it is rarely used intravenous (IV) fluids and medication may be administered to beyond 7-10 days. critically ill neonates. • Umbilical artery catheterization provides direct access to the arterial • The cord is cut horizontally with the scalpel, approximately 1.5-2 cm blood supply and allows accurate measurement of arterial blood from the abdominal wall. Two thick-walled small arteries and one pressure, a source of arterial blood sampling, and intravascular access thin-walled larger vein should be identified. The umbilical vein may for fluids and medications. continue to ooze blood. Hemostasis is achieved by tightening the • Indications umbilical tape or suture. The arteries do not usually bleed secondary to • Continuous arterial blood pressure monitoring vasospasm. • Arterial blood gas sampling • A properly placed umbilical vein catheter appears to travel cephalad until it passes through the ductus venosus. • Blood sampling for other laboratory tests and studies • In the fetus, the ductus venosus shunts a portion of the left umbilical • Exchange transfusion vein blood flow directly to the inferior vena cava. -

Early Intracardiac Thrombosis in Preterm Infants and Thrombolysis with Recombinant Tissue Type Plasminogen Activator
F66 Arch Dis Child Fetal Neonatal Ed 2001;85:F66–F72 Arch Dis Child Fetal Neonatal Ed: first published as 10.1136/fn.85.1.F66 on 1 July 2001. Downloaded from CASE REPORT Early intracardiac thrombosis in preterm infants and thrombolysis with recombinant tissue type plasminogen activator F Ferrari, F Vagnarelli, G Gargano, M F Roversi, O Biagioni, A Ranzi, G B Cavazzuti Abstract and superior or inferior vena cava syndrome45; Objectives—To determine the incidence of occlusion of the right pulmonary artery has catheter related thrombosis and to test the also been reported.6 eYcacy of recombinant tissue type plas- Cardiotomy with surgical removal of the minogen activator (rt-PA) in preterm thrombus can be performed even in preterm infants. infants,7 but it has a high rate of mortality and, Study design—From January 1995 to De- being a hazardous procedure, is considered too cember 1998, echocardiography was per- risky.6 formed in the first few days of life in 76 Thrombolytic agents such as heparin and very low birthweight (< 1500 g) infants out streptokinase are no longer considered to be of a total of 147 having an umbilical cath- the ideal treatment in the neonatal period, as eter placed. When intracardiac thrombo- they lead to a systemic coagulopathic state.8 sis was diagnosed, rt-PA infusion was per- Newer plasminogen activators, including formed. recombinant tissue type plasminogen activator Results—Four infants (5%) developed an (rt-PA), are more clot selective and may repre- intracardiac thrombosis during the first sent a good alternative for thrombolytic few days of life. -

Umbilical Lines and Infusions Feb 2017
Neonatal Intensive Care Unit Clinical Guideline Umbilical Artery and Vein Catheterisation Indications for umbilical catheterisation For frequent measurement of arterial blood gases / other blood tests For continuous arterial blood pressure monitoring. For exchange transfusion. For fluids, inotropes The decision to place semi-elective umbilical lines should take into account benefits and potential risks. If in doubt, this should be discussed with the attending / duty consultant. For UVC, we always use the double-lumen UVC catheter which may avoid the need for peripheral cannulation. Contraindications Gastroschisis Omphalocele Omphalitis Risks Infection is the main complication for deep lines. Do you need umbilical lines? Assessment of the baby Make sure that the baby’s condition and vital signs are stable especially temperature prior to undertaking invasive procedures such as insertion of UAC and UVC where possible. Babies with umbilical lines can be safely nursed prone . This is provided that the lines have been correctly secured (see below) and the site has been observed in the supine position during the procedure. Provided all oozing of blood has stopped the baby should then be nursed in the prone position if there is respiratory distress. NOTE If the baby was hypotensive at the time of UAC insertion bleeding may occur from the umbilicus once the blood pressure is restored if care was not taken to ensure haemostasis at the time of insertion. Equipment Sterile UAC or cut-down set: sterile drapes, fine non-toothed forceps, blind-end dilator, scissors and suture holder, artery forceps x 3, toothed forceps, gauze and cotton wool, scalpel. Standalone lighting Some may wish to use head-mounted magnification Sterile gown, sterile gloves (2 pairs for double-gloving). -
Guide to Preventing Central Line-Associated Bloodstream Infections
ImpGuide_CLABSI_Cover_wSpine17x11_rev3.indd 1 10/6/2015 6:21:59 PM Guide to Preventing Central Line-Associated Bloodstream Infections About APIC APIC’s mission is to create a safer world through prevention of infection. The association’s more than 15,000 members direct infection prevention programs that save lives and improve the bottom line for hospitals and other healthcare facilities. APIC advances its mission through patient safety, implementation science, competencies and certification, advocacy, and data standardization. About the Sponsor As a long-standing APIC Strategic Partner, BD is pleased to support the dissemination as a free resource of the revised APIC Implementation Guide on CLABSI. About the Implementation Guide Series APIC Implementation Guides help infection preventionists apply current scientific knowledge and best practices to achieve targeted outcomes and enhance patient safety. This series reflects APIC’s commitment to implementation science and focus on the utilization of infection prevention research. Topic-specific information is presented in an easy-to-understand and use format that includes numerous examples and tools. Visit www.apic.org/implementationguides to learn more and to access all of the titles in the Implementation Guide series. Printed in the United States of America First edition, December 2015 ISBN: 1-933013-56-7 All inquiries about this guide or other APIC products and services may be directed addressed to: APIC 1275 K Street NW, Suite 1000 Washington, DC 20005 Phone: 202-789-1890 Fax: 202-789-1899 Email: [email protected] Web: www.apic.org © 2015, Association for Professionals in Infection Control and Epidemiology, Inc. (APIC). Disclaimer All rights reserved. -

Umbilical Venous Catheterisation
Neonatal Intensive Care Unit St Peter’s Hospital Umbilical Venous Catheterisation Amendments Date Pages Comment (s) Approved by 2019 Updated guideline Primary Author: Dr Tracy Lawson Consultant Neonatologist Contact for comments: [email protected] Status: Approval date: September 2019 Ratified by: Neonatal Guidelines Group Review date: September 2024 Section 1 Current Version First ratified: Review date: Issue Page 1 of 21 Organisational is held on the September 2019 September 2024 1 Policy Intranet Neonatal Intensive Care Unit St Peter’s Hospital Contents 1. Guideline Indications 3 Insertion length 4 Procedure 5 Assessing position/documentation 7 Nursing care and monitoring 9 2. Appendices Appendix 1: Required equipment for UVC insertion 10 Appendix 2: How to secure UVC 11 Appendix 3: Line placement examples 13 Appendix 4: Neonatal UVC insertion check list 15 3. Supporting References 16 4. Supporting Trust Guidelines 16 5. Guideline Governance a) Scope, Purpose, Duties and Responsibilities, Approval and Ratification, 17 Dissemination and Implementation, Review and Revision Arrangements b) Equality Impact Assessment 19 c) Document Checklist 20 Section 1 Current Version First ratified: Review date: Issue Page 2 of 21 Organisational is held on the September 2019 September 2024 1 Policy Intranet Neonatal Intensive Care Unit St Peter’s Hospital Umbilical Vein Catheterisation Policy Indications For administration of IV fluids, Dextrose concentrations >12.5%, TPN, inotropes, antibiotics, blood products, sedation If obtaining peripheral IV access is difficult In conjunction with UAC for exchange transfusion Always site a double-lumen UVC as this may avoid the need for peripheral cannulation. Contra-indications Gastroschisis Omphalocele Omphalitis Necrotising Enterocolitis Risks INFECTION Infection is the most common complication, with a potential to be extremely serious. -

Umbilical Line Guidelines
Newborn Critical Care Center (NCCC) Guidelines Umbilical Line Placement GENERAL INFORMATION Umbilical vein and/or artery catheterization is an imperative and potentially life-saving measure performed for critically ill infants that require timely and reliable vascular access. This vascular access may be used for the administration of fluids (e.g., parenteral nutrition, crystalloid, colloid, and medications), the obtainment of laboratory values, as well as accurate and continuous blood pressure monitoring. I. Indications for Placement A. Umbilical arterial catheterization 1. Frequent monitoring of arterial blood gases and/or blood sampling 2. Continuous monitoring of arterial blood pressure 3. If no venous access, infusion of maintenance glucose/electrolyte solutions 4. Exchange transfusion B. Umbilical venous catheterization 1. Emergency vascular access for fluid resuscitation and medication administration 2. Central venous access for parenteral nutrition 3. Hypertonic fluid administration 4. Vasoactive drug administration (e.g., inotropes, vasopressors) 5. Exchange transfusion II. Selection of Catheter and Fluids A. Catheter size 1. Umbilical artery catheter (UAC) a) Use 5 Fr catheter for term infants and infants > 1500 grams b) Use 3.5 Fr catheter for infants ≤ 1500 grams c) Use 2.5 Fr for ELBWs that will not accommodate a 3.5 Fr catheter 2. Umbilical venous catheter (UVC) a) Select catheter size based on the size of the infant B. UVC type 1. Use of multiple lumen UVCs is associated with decreased usage of PIVs in the first week of -

A Review of Umbilical Venous Catheter-Related Complications at a Tertiary Neonatal Unit in Singapore
Singapore Med J 2021; 62(1): 29-33 Original Article https://doi.org/10.11622/smedj.2019140 A review of umbilical venous catheter-related complications at a tertiary neonatal unit in Singapore Sharon Si Min Goh1, MBBS, Sheau Yun Kan1, MBBS, MMed, Srabani Bharadwaj1, MRCPCH, FRCPCH, Woei Bing Poon1, MRCPCH, FAMS INTRODUCTION: Umbilical venous catheters (UVCs), commonly inserted in neonates for vascular access, are not without complications. METHODS: A single-centre retrospective cohort study that reviewed complications related to UVC insertion in neonates was conducted in a tertiary neonatal unit in Singapore from January 2016 to July 2017. Ideal UVC position was defined as catheter tip within 0.5 cm above or below the diaphragm. Catheter-related sepsis was defined as clinical or biochemical abnormalities suggesting any new-onset or worsening sepsis 72 hours before or after removal of UVCs, with or without positive culture. Catheter-associated bloodstream infection (CABSI) was defined as positive microbiological growth in one or more blood cultures obtained from a symptomatic infant up to two days after UVC placement or within 48 hours of catheter removal. RESULTS: 108 patients had UVC insertions. Mean gestational age and birth weight were 30.4 ± 4.0 weeks and 1,536.2 g ± 788.9 g, respectively. Mean UVC duration was 6.6 days. The UVC was in an ideal position in 27 (25.0%), deep in 13 (12.0%) and short in 35 (32.4%) neonates. One-third of the UVCs (n = 33) were malpositioned. Catheter-related sepsis was observed in 16 (14.8%) neonates, with 5 (4.6%) having CABSI. -

Ultrasound-Guided Umbilical Catheter Insertion in Neonates
Journal of Perinatology (2011) 31, 344–349 r 2011 Nature America, Inc. All rights reserved. 0743-8346/11 www.nature.com/jp ORIGINAL ARTICLE Ultrasound-guided umbilical catheter insertion in neonates SE Fleming and JH Kim Division of Neonatology, UCSD Medical Center, San Diego, CA, USA Introduction Objective: Umbilical catheter placement is a routine neonatal emergency Inserting umbilical venous (UVC) and umbilical arterial (UAC) procedure that has large variability in technical methods. Commonly catheters is a routine urgent procedure in sick preterm and term used methods are unable to accurately estimate insertion lengths, and neonates. Two of the most common methods used to guide catheter X-rays cannot always identify malpositioned catheters. In clinical practice, insertion length are the shoulder–umbilicus length graph1 and the placement of umbilical lines takes time away from nursing during a a regression equation based on birth weight (BW).2 In these critical transition period. Ultrasound is a safe and commonly used tool in methods, catheters are inserted and advanced blindly to the the nursery for clinical management of sick neonates and has been shown predetermined length from the umbilicus. Both anterior-posterior to readily identify central catheter tip position. In this study, we sought to and lateral radiographs are taken after placement of the catheters determine a more time-efficient and accurate means of umbilical catheter to check the adequacy of catheter positioning. Many times, the placement using bedside ultrasound. catheters are not placed at the optimal position, thus necessitating Study Design: This is a prospective, randomized, pilot trial of infants them to be repositioned and X-rays repeated. -

Case Report Prenatal and Postnatal Sonographic Confirmation of Congenital Absence of the Ductus Venosus in a Child with Noonan Syndrome
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by IUPUIScholarWorks Hindawi Case Reports in Radiology Volume 2017, Article ID 3068178, 3 pages https://doi.org/10.1155/2017/3068178 Case Report Prenatal and Postnatal Sonographic Confirmation of Congenital Absence of the Ductus Venosus in a Child with Noonan Syndrome Christopher L. Newman,1,2 Matthew R. Wanner,2 and Brandon P. Brown2,3,4 1 Department of Anatomy and Cell Biology, Indiana University School of Medicine, Indianapolis, IN, USA 2Department of Radiology, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, USA 3Department of Medical Humanities and Health Studies, Indiana University School of Liberal Arts, Indianapolis, IN, USA 4Department of Philosophy, Indiana University School of Liberal Arts, Indianapolis, IN, USA Correspondence should be addressed to Brandon P. Brown; [email protected] Received 16 May 2017; Accepted 30 July 2017; Published 6 September 2017 Academic Editor: Daniel P. Link Copyright © 2017 Christopher L. Newman et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The ductus venosus serves as an important vascular pathway for intrauterine circulation. This case presents a description of an absent ductus venosus in a female patient with Noonan syndrome, including both prenatal and postnatal imaging of the anomaly. In the setting of the anomalous vascular connection, the umbilical vein courses inferiorly to the iliac vein in parallel configuration with the umbilical artery. This finding was suspected based on prenatal imaging and the case was brought to attention when placement of an umbilical catheter was thought to be malpositioned given its appearance on radiography. -

Umbilical Catheter Insertion
NTS Clinical Guideline Title: Umbilical Catheter Insertion U Kariholu 2013 Authored by: Updated L Collier 2015 Reviewed date: November 2020 Updated K Jamieson 2020 Next review Reviewed by: Nandiran Ratnavel, Syed Mohinuddin November 2022 date: This guideline is applicable to all medical staff, ANNPs or extended role practitioners placing umbilical catheters in neonates. Indications for Umbilical Arterial Catheter Direct blood pressure measurement Frequent acid-base and oxygen monitoring Frequent blood sampling Exchange transfusion Indications for Umbilical Venous Catheter During resuscitation for administration of emergency drugs/fluids Difficult peripheral IV access Extreme prematurity in advance of long line insertion Infusion of hypertonic solutions (eg >12.5% dextrose) Administration of vaso-active drugs Exchange transfusion The umbilical vessels can be catheterised up to 7-10 days after delivery although it is easiest just after birth. If the cord is dry, application of saline-soaked gauze around the cord for at least one hour prior to the procedure may be helpful. Relative Contraindications Anterior abdominal wall defects o Exomphalos, Gastroschisis, Umbilical fistula Infection o NEC, Peritonitis, Omphalitis Evidence of local vascular compromise in lower limbs Abdominal surgery requiring an incision above the umbilicus Considerations There are three key considerations when siting umbilical catheters: protecting the infant’s safety by maintaining warmth, comfort and humidity and avoiding exposure to harm e.g. chemical -
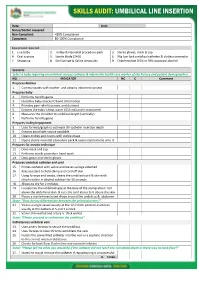
Skills Audit: Umbilical Line Insertion
SKILLS AUDIT: UMBILICAL LINE INSERTION Date: Unit: Nurse/Doctor assessed: Non-Compliant: <80% Compliance Compliant: 80-100% Compliance Equipment required: 1. Live baby 2. Trolley & Neonatal procedure pack 3. Sterile gloves, mask & cap 4. Oral sucrose 5. Sterile blade (24G) 6. 5Fg luer lock umbilical catheter & clotless connector 7. Strapping 8. 5ml Syringe & Saline Ampoules 9. Chlorhexidine 0.5% in 70% isopropyl alcohol Scenario Select a baby requiring an umbilical venous catheter & inform the health care worker of the history and patient demographics. NO. INDICATOR NC C Comment Prepares Mother 1. Communicates with mother and obtains informed consent Prepares baby 2. Performs hand hygiene 3. Identifies baby-checks ID band information 4. Provides pain relief (sucrose, and dummy) 5. Ensures the baby is kept warm (ICU crib) and is monitored 6. Measures the shoulder to umbilical-length (vertically) 7. Performs hand hygiene Prepares trolley/equipment 8. Uses formula/graph to estimate UV catheter insertion depth 9. Ensures good light source available 10. Cleans trolley and covers with sterile drape 11. Opens sterile neonatal procedure pack & opens sterile items onto it Prepares for aseptic technique 12. Dons mask and cap 13. Performs sterile procedure hand wash 14. Dons gown and sterile gloves Prepares umbilical catheter and cord 15. Primes catheter with saline and leaves syringe attached 16. Asks assistant to hold clamp and cord off skin 17. Using forceps and swabs, cleans the umbilical cord & skin with chlorhexidine in alcohol solution for 30 seconds 18. Allows to dry for 2 minutes 19. Loosely ties the umbilical tape at the base of the stump about 1cm above the abdominal skin & cuts the cord about 2cm above the skin 20.