Best Practices for Coloring Medical and Healthcare Plastic Products
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Catalog for Other Products and Patterns.15 Cantilever Forms and Pool Accessories
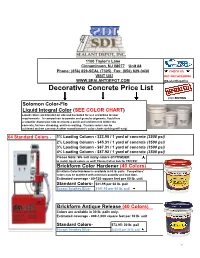
1100 Taylor's Lane Cinnaminson, NJ 08077 Unit #4 Phone: (856) 829-SEAL (7325) Fax: (856) 829-0430 CHECK US VISIT US! OUT ON FACEBOOK WWW.SEALANTDEPOT.COM @SealantDepotInc Decorative Concrete Price List 2020 EDITION Solomon Color-Flo Liquid Integral Color (SEE COLOR CHART) Liquid colors are blended on site and bucketed for use according to your requirements. In comparison to powder and granular pigments, liquid has a superior dispersion rate to ensure a quick and uniform mix within the concrete, far less streaking, and less waiting. Custom colors can be achieved and we can match other manufacturer's color charts (pricing will vary). 64 Standard Colors - 1% Loading Column - $23.95 / 1 yard of concrete (3500 psi) 2% Loading Column - $45.31 / 1 yard of concrete (3500 psi) 3% Loading Column - $67.31 / 1 yard of concrete (3500 psi) 4% Loading Column - $87.92 / 1 yard of concrete (3500 psi) Please Note: We sell many colors of POWDER to match liquid colors as well! Please Call or Ask for PRICES! Brickform Color Hardener (40 Colors) Brickform Color Hardener is available in 60 lb. pails. Competitors' colors may be matched with minimum quantity and lead time. Estimated coverage - 80-120 square feet per 60 lb. unit Standard Colors- $41.95 per 60 lb. pail Except Smokey Blue- $141.95 per 60 lb. pail Brickform Antique Release (40 Colors) Colors are available in 30 lb. pails only. Estimated coverage - 800-1,000 square feet per 30 lb. unit Standard Colors- $72.95- 30 lb. pail Except Smokey Blue- $220.95 per 30 lb. -
Liquid Vs Pellet Color Is a Critical Feature in Consumer Packaging That Enables Brands to Create Differentiation and Recognizable Identity on Shelf
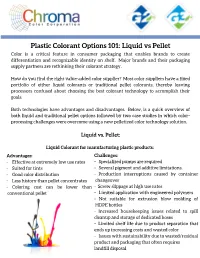
Plastic Colorant Options 101: Liquid vs Pellet Color is a critical feature in consumer packaging that enables brands to create differentiation and recognizable identity on shelf. Major brands and their packaging supply partners are rethinking their colorant strategy. How do you find the right value-added color supplier? Most color suppliers have a fixed portfolio of either liquid colorants or traditional pellet colorants, thereby leaving processors confused about choosing the best colorant technology to accomplish their goals. Both technologies have advantages and disadvantages. Below, is a quick overview of both liquid and traditional pellet options followed by two case studies in which color- processing challenges were overcome using a new pelletized color technology solution. Liquid vs. Pellet: Liquid Colorant for manufacturing plastic products: Ad vantages: Challenges: - Effective at extremely low use rates - Specialized pumps are required - Suited for tints - Several pigment and additive limitations. - Good color distribution - Production interruptions caused by container - Less history than pellet concentrates changeover - Coloring cost can be lower than - Screw slippage at high use rates conventional pellet - Limited application with engineered polymers - Not suitable for extrusion blow molding of HDPE bottles - Increased housekeeping issues related to spill cleanup and storage of dedicated hoses - Limited shelf life due to product separation that ends up increasing costs and wasted color - Issues with sustainability due to wasted/residual -

General Brochure
FLAME LIGHT UV RETARDANTS ANTIOXIDANTS STABILIZERS ABSORBERS PLASTIC ADDITIVES TAILOR MADE FORMULATIONS GREENCHEMICALS POLICY OUR GOAL is to develop and promote improved Flame Retardant solutions! Environmental friendly: Halogen free, with low dosage, dust free, migration free. CONTENTS OUR FLAME RETARDANTS PRODUCTS: Masterbatches, powder blends, compacted blends, cold extruded pellets, dropped beads. BROMINATED FLAME RETARDANTS PAG. 08 HALOGEN FREE FLAME RETARDANTS PAG. 10 MASTERBATCHES POWDER BLENDS COMPACTED BLENDS COLD EXTRUDED LIQUID DISPERSIONS INORGANIC FLAME RETARDANTS PAG. 13 PELLETS FLAME RETARDANTS FORMULATIONS PAG. 14 MAIN ACTIVITIES: OTHER PRODUCTS: • XPS, EPS, X-EPS • Antioxidants ANTIOXIDANTS PAG. 16 • XPE, XPU • Uv • Engineering Thermoplastics • Processing aids • Reactive flame retardants • Colors. UV ABSORBERS - LIGHT STABILIZERS PAG. 18 ONE SHOT FORMULATIONS PAG. 21 GREENCHEMICALS is very active in the substitution of SVHC molecules and provides optimized solutions considering: OPTICAL BRIGHTENERS PAG. 22 • Fire Performance and thermal stability • Superior Environmental and health profile (more sustainable) SMA PAG. 22 • Compatibility with polymeric matrix • Cost/Performance PROCESS AID & STABILIZERS PAG. 22 GREENCHEMICALS Srl complies with REACH, CLP, SVHC, Food Contact, RoHS PROCESS AID & PEROXIDES PAG. 23 regulations and is determined to pursue the continuous improvement in all aspects of its work. QUALITY MANAGEMENT SYSTEM Greenchemicals’ decision to adopt a Quality Management System (QMS) of ISO 9001 is to improve -
Additives for Polyolefins: Getting the Most out of Polypropylene
ADDITIVES FOR POLYOLEFINS PLASTICS DESIGN LIBRARY (PDL) PDL HANDBOOK SERIES Series Editor: Sina Ebnesajjad, PhD ([email protected]) President, FluoroConsultants Group, LLC Chadds Ford, PA, USA www.FluoroConsultants.com The PDL Handbook Series is aimed at a wide range of engineers and other professionals working in the plastics indus- try, and related sectors using plastics and adhesives. PDL is a series of data books, reference works, and practical guides covering plastics engineering, applications, proces- sing, and manufacturing, and applied aspects of polymer science, elastomers, and adhesives. Recent titles in the series Biopolymers: Processing and Products, Michael Niaounakis (ISBN: 9780323266987) Biopolymers: Reuse, Recycling, and Disposal, Michael Niaounakis (ISBN: 9781455731459) Carbon Nanotube Reinforced Composites, Marcio Loos (ISBN: 9781455731954) Extrusion, 2e, John Wagner and Eldridge Mount (ISBN: 9781437734812) Fluoroplastics, Volume 1, 2e, Sina Ebnesajjad (ISBN: 9781455731992) Handbook of Biopolymers and Biodegradable Plastics, Sina Ebnesajjad (ISBN: 9781455728343) Handbook of Molded Part Shrinkage and Warpage, Jerry Fischer (ISBN: 9781455725977) Handbook of Polymer Applications in Medicine and Medical Devices, Kayvon Modjarrad and Sina Ebnesajjad (ISBN: 9780323228053) Handbook of Thermoplastic Elastomers, Jiri G. Drobny (ISBN: 9780323221368) Handbook of Thermoset Plastics, 2e, Hanna Dodiuk and Sidney Goodman (ISBN: 9781455731077) High Performance Polymers, 2e, Johannes Karl Fink (ISBN: 9780323312226) Introduction -

US5132743.Pdf
|||||||||||||| US00532743A United States Patent (19) 11) Patent Number: 5,132,743 Bujese et al. 45) Date of Patent: Jul. 21, 1992 54 INTERMEDIATE TRANSFER SURFACE AND 59-91465 5/1984 Japan. METHOD OF COLOR PRINTING 2-106530 4/1990 Japan . (75) Inventors: David P. Bujese; Peter E. Materazzi, OTHER PUBLICATIONS both of Southington, Conn. Article entitled "Fluorosilicone and Conductive Sili 73) Assignee: Olin Corporation, Cheshire, Conn. cones' from Rubber World Magazine, vol. 200, No. 3, Jun. 1989. 21 Appl. No.: 546,287 Japanese Patent Publication 59-77467(A), issued May 2, 22 Filed; Jun. 29, 1990 1984, assigned to Konishiroku Shashin Kogyo KK-Ab (51) Int. Cl. ............................................. GO3G 15/16 Stract. (52) U.S. C. ..................................... 355/274; 355/271 Japanese Patent Publication 56-165173(A), published (58) Field of Search ............... 355/274, 275,271, 277, Dec. 18, 1991, assigned to Ricoh K.K.-Abstract. 355/273, 272, 279, 256, 257; 430/126, 48; Primary Examiner-A. T. Grimley 428/244, 323, 282, 421 Assistant Examiner-Thu Dang 56 References Cited Attorney, Agent, or Firm-Ralph D'Alessandro U.S. PATENT DOCUMENTS 57 ABSTRACT 3,591,276 7/1971 Byrne. an improved intermediate transfer surface employing a 3,893,761 7/1975 Buchan et al. conductive material dispersed in a fluorosilicone layer is 3,923,392 12/1975 Buchan et al. provided for use in electrostatic color image transfers. 3,957,367 3/1976 Goel .................................... 355/279 The intermediate transfer surface is heat and solvent 4,095,886 6/1978 Koeleman et al. 4,453,820 6/1984 Suzuki ................................. 355/279 resistant and retains its electrical conductivity upon 4.58,976 5/1985 Tarumi et al. -

DUPONT™ RYNITE® PET THERMOPLASTIC RESINS MOLDING GUIDE Table of Contents
DUPONT™ RYNITE® PET THERMOPLASTIC RESINS MOLDING GUIDE Table of Contents 1. PROCESSING GUIDELINE SUMMARY . 1 Drying Considerations . 1 Mold Temperatures . 1 Shrinkage Considerations . 1 Cylinder and Melt Temperatures . 1 Operating Conditions . 1 2. SAFE HANDLING INFORMATION . 2 Safety Precautions . 2 3. DRYING GUIDELINES . 3 Effects of Moisture . 3 Moisture Absorption . 3 Hopper Dryer Conditions . 3 4. MOLDING EQUIPMENT—MOLDS . 4 Mold Temperature Control . 4 Basic Recommendations . 4 Mechanical Structure . 5 Conventional Runner System and Gate Layout . 5 Hot Runner Systems . 8 Venting . 9 Draft Angles . 9 Sharp Corners . 9 5. MOLDING EQUIPMENT—INJECTION UNIT . 10 Screw . 10 Check Ring or Back Flow Valve . 10 Corrosion/abrasion . 10 Nozzles . 11 Accumulator for Thin Wall Applications . 11 6. MOLDING PARAMETERS—START-UP AND SHUTDOWN PROCEDURES . 11 Purging . 11 Start-up . 12 Shutdown . 12 Interruptions . 12 7. MOLDING PARAMETERS—MOLDING . 12 Melt and Cylinder Temperature . 12 Cavity Mold Temperature . 13 Injection Phase . 13 Pack or Hold Pressure Phase . 13 Screw Retraction Phase . 14 Recommended Processing Parameters . 14 8. MATERIAL BEHAVIOR . 15 Chemical Structure . 15 Flow Length . 15 Shrinkage . 15 Shrinkage of Rynite® PET . 15 Post-Mold Shrinkage . 16 9. AUXILIARY OPERATIONS . 16 Regrind . 16 Coloring . 16 Important note . 17 10. TROUBLESHOOTING GUIDE . 17 1. PROCESSING GUIDELINE SUMMARY Shrinkage Considerations Rynite® PET thermoplastic polyester resins and other DuPont Shrinkage in semi-crystalline resins such as Rynite® PET is thermoplastic resins may be processed on conventional due to: injection molding machines using standard industry practices . • Crystallization of the polymer Specific attention to processing details will enhance quality and productivity . This summary represents a key subset of the • Thermal contraction of the part as it cools to room detailed molding information found in the remainder of this temperature molding guide . -
The Dynisco Extrusion Processors Handbook 2Nd Edition
The Dynisco Extrusion Processors Handbook 2nd edition Written by: John Goff and Tony Whelan Edited by: Don DeLaney Acknowledgements We would like to thank the following people for their contributions to this latest edition of the DYNISCO Extrusion Processors Handbook. First of all, we would like to thank John Goff and Tony Whelan who have contributed new material that has been included in this new addition of their original book. In addition, we would like to thank John Herrmann, Jim Reilly, and Joan DeCoste of the DYNISCO Companies and Christine Ronaghan and Gabor Nagy of Davis-Standard for their assistance in editing and publication. For the fig- ures included in this edition, we would like to acknowledge the contributions of Davis- Standard, Inc., Krupp Werner and Pfleiderer, Inc., The DYNISCO Companies, Dr. Harold Giles and Eileen Reilly. CONTENTS SECTION 1: INTRODUCTION TO EXTRUSION Single-Screw Extrusion . .1 Twin-Screw Extrusion . .3 Extrusion Processes . .6 Safety . .11 SECTION 2: MATERIALS AND THEIR FLOW PROPERTIES Polymers and Plastics . .15 Thermoplastic Materials . .19 Viscosity and Viscosity Terms . .25 Flow Properties Measurement . .28 Elastic Effects in Polymer Melts . .30 Die Swell . .30 Melt Fracture . .32 Sharkskin . .34 Frozen-In Orientation . .35 Draw Down . .36 SECTION 3: TESTING Testing and Standards . .37 Material Inspection . .40 Density and Dimensions . .42 Tensile Strength . .44 Flexural Properties . .46 Impact Strength . .47 Hardness and Softness . .48 Thermal Properties . .49 Flammability Testing . .57 Melt Flow Rate . .59 Melt Viscosity . .62 Measurement of Elastic Effects . .64 Chemical Resistance . .66 Electrical Properties . .66 Optical Properties . .68 Material Identification . .70 SECTION 4: THE SCREW AND BARREL SYSTEM Materials Handling . -

Conference Proceedings
Conference Proceedings Plastics Are Shaping Tomorrow Today April 18-21,1988 Society of Plastics Engineers IMG, POLYMER MO DIFIERS&ADDmV ES, THERMOPLA STICS, FAILURE ANALYSIS, COM PUTERSINPLAS TICS, MATERIALS & FOAMS, ENER GETIC PROCESS ING, POLYMERS COLOR & APPEAR ANCE, ENERGE TIC, DISPOSING & RECYCLING OF PLASTIC ALLOYS & BLE NDS, PLASTICS IN ELECTRONICS &PHOTOTRONICS 46th ANNUAL iCHNICAL CONFERENCE & EXHIBITS Contents COLOR AND APPEARANCE DIVISION Synthetic Complex Metal Oxide Pigments for Plastics 2 J. Hackman, The Shepherd Color Co. Colored Luminescence—The Next Frontier 7 T. Mahany II, Eldon Enterprises Ltd. Liquid Color in PET Packaging 10 D. Peacock, PDI The Effects of Metal Ions on Daylight Fluorescent Pigments in Plastic Systems 12 J. Cook, Day-Glo Color Corp. Colorants for Polymers Regulation as Indirect Food Additives 16 G. McCowin, Food and Drug Administration Refractive Index—A Key to Understanding Color Differences 18 B. Donald, Dow Chemical Co. R. Mathew, Americhem, Inc. The Effect of Concentrate Viscosity Characteristics on Color Development in LLDPE Film 22 R Patet, Colortech Inc. W. Baker, Queen's University Concentrates of Minerals, Additives, and Pigments Using Low MW Polypropylene Carriers 24 L. Bourland, ARCO Chemical Co. Color Stability of Pigmented Polystyrene 28 D. Holtzen, £ /. du Pont de Nemours & Co., Inc. EXTRUSION DIVISION Extrusion Characteristics of Polypropylene Resins 34 C. Cheng, Exxon Chemical Co. Analysis of Slump in Plastic Pipe Extrusion 38 A. Giacomin, Texas A&M University S. Doshi, McGill University Product Liability—Who Pays for It? , 41 R. Gregory, Robert Gregory Associates, Inc. Evaluating Extruder Screw Performance 45 E. Steward and W. Kramer, Crompton & Knowles Corp. On-Line Additive Injection in the Extrusion Process 51 S. -
Just Add Liquid
JUST ADD LIQUID Quick guide to ColorMatrix™ liquid color for plastics and silicones THE RIGHT COLORANT FOR YOU Understanding which colorant technology best suits your particular product application will help ensure you gain maximum performance and value from your colorant processing. Avient is able to service customers globally with a full range of solid masterbatch and liquid colorant solutions to meet your product requirements. This ‘quick guide’ focuses specifically on ColorMatrix™ liquid colorant systems, providing a practical overview of factors to consider when selecting a colorant solution. Whether you are using color for functional or aesthetic purposes, careful consideration of each of the following points will prove valuable in your color selection and implementation: • Is your color formulation and polymer fully compatible and optimized for your production process? • How efficiently can you specify, trial and implement a new color? • How stable, consistent and repeatable is your color processing? • How quickly can you change colors during processing? • What level of technical support do you receive from your colorant supplier? • Does your colorant meet all the regulatory requirements of your intended market? LIQUID COLOR Liquid colorant systems are increasingly used throughout the world in an expanding range of VERSATILITY polymers and product applications. POLYMERS PROCESSES COLOR TYPES* • PET • Injection Stretch • Tints • Polyolefins Blow Molding (ISBM) • Translucents • PVC • Injection molding • Opaques • Extrusion Blow • Special effects Molding (EBM) • Additive additions • Extrusion Sheet, (functional colors) Fiber, Film Specialized liquid color dispersions for Silicones are also available. More information can be found at avient.com. *available from Avient THE MAGIC OF LIQUID COLOR Liquid color is a uniform dispersion of color pigment or dye into a liquid carrier material. -

(12) Patent Application Publication (10) Pub. No.: US 2010/0204395 A1 Rajaraman (43) Pub
US 20100204395A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0204395 A1 Rajaraman (43) Pub. Date: Aug. 12, 2010 (54) LIQUID COLOR CONCENTRATE FOR Related U.S. Application Data POLYESTER ARTICLES (60) Provisional application No. 60/974,616, filed on Sep. (75) Inventor: Hari Rajaraman, Chardon, OH 24, 2007. (US) Publication Classification Correspondence Address: POLYONE CORPORATION (51) Int. Cl. AVON LAKE, OH 44012 (US) C09D 5/00 (2006.01) (73) Assignee: PolyOne Corporation, Avon Lake, (52) U.S. Cl. .................................... 524/559; 106/287.26 OH (US) (57) ABSTRACT (21)21) Appl. NoNo.: 12/679,6279 A liquid color concentrate is disclosed, having a polyalkylene (22) PCT Filed: Sep. 23, 2008 polyol carrier, colorant; and optionally other functional addi 9 tives. The colorant can be one or more pigments, one or more (86). PCT No.: PCT/US08/77311 dyes, or combination thereof. The liquid color concentrate is compatible with polyalkylene terephthalate resins, especially S371 (c)(1), to make colored polyester beverage bottles and other polyes (2), (4) Date: Mar. 23, 2010 ter articles. US 2010/0204395 A1 Aug. 12, 2010 LIQUID COLOR CONCENTRATE FOR 0011. Another feature of the present invention is that the POLYESTER ARTICLES colorant can include pigment(s), dye(s), or both as needed by the polymer engineer and product designer to achieve desired CLAIM OF PRIORITY color effects. 0012. Other features will become apparent from a descrip 0001. This application claims priority from U.S. Provi tion of the embodiments of the invention. sional Patent Application Ser. No. 60/974,616 bearing Attor ney Docket Number 12007018 and filed on Sep. -

New to Using Color Concentrates? Follow These Tips to Improve Results
Tips and Techniques Reprinted From: PLASTICS TECHNOLOGY Magazine Highly-loaded color concentrates have been proving their mettle in terms of cost- performance in rigid packaging and building products. New to Using Color Concentrates? Follow These Tips to Improve Results With a focus on highly loaded color concentrates, here is a guide for processors of rigid packaging and building products on how to specify the appropriate colorant for these applications. As younger engineers and buyers enter the plastics industry, there or other sample parts in your resin that capture your vision of the is a need to provide the next generation with the right funda- end product. mental knowledge and One of the most important factors to keep in mind when By Ronald Harris and Hari Rajaraman awareness to produce designing a plastic product is that both the resin and color concen- Chroma Color Corp. high-quality colored trate must be suitable for the intended process, such as injection, plastic parts. Designers blow, compression molding or extrusion. This is because resins, and brand owners understand the importance of choosing the pigments, dyes, and additives must be able to withstand extreme right color to ensure their products stand out from the competi- heat exposure during the molding process, including shear heat tion. Yet they often may not have enough fundamental knowledge generated when a material flows into a mold. If the material on its and awareness to produce quality colored plastic parts, and so own is not sufficiently durable for its end-use environment, it will turn to their processing partners for help. -
Just Add Liquid
JUST ADD LIQUID Quick guide to ColorMatrix liquid color for plastics and silicones THE RIGHT COLORANT FOR YOU Understanding which colorant technology best suits your particular product application will help ensure you gain maximum performance and value from your colorant processing. PolyOne is able to service customers globally with a full range of solid masterbatch and liquid colorant solutions to meet your product requirements. This ‘quick guide’ focuses specifically on ColorMatrix liquid colorant systems, providing a practical overview of factors to consider when selecting a colorant solution. Liquid colorant systems are increasingly used Whether you are using color for functional or aesthetic purposes, careful consideration of LIQUID COLOR throughout the world in an expanding range each of the following points will prove valuable in your color selection and implementation: VERSATILITY of polymers and product applications. • Is your color formulation and polymer fully compatible and optimized for your production process? POLYMERS PROCESSES COLOR TYPES* • How efficiently can you specify, trial and implement a new color? • PET • Injection Stretch • Tints • How stable, consistent and repeatable is your color processing? • Polyolefins Blow Molding (ISBM) • Translucents • How quickly can you change colors during processing? • PVC • Injection molding • Opaques • What level of technical support do you receive from your colorant supplier? • Extrusion Blow • Special effects Molding (EBM) • Does your colorant meet all the regulatory requirements of your intended market? • Additive additions • Extrusion (functional colors) Sheet, Fiber, Film Liquid color dispersions for Silicones are also available from PolyOne’s GSDI product range which specializes in silicone color. Further information can be found at polyone.com *available from PolyOne THE MAGIC OF LIQUID COLOR Liquid color is a uniform dispersion of color pigment or dye into a liquid carrier material.