Molecular Dissection of CRC Primary Tumors and Their Matched Liver
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Mechanism of Action Through an IFN Type I-Independent Responses To
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 is online at: average * The Journal of Immunology , 12 of which you can access for free at: 2012; 188:3088-3098; Prepublished online 20 from submission to initial decision 4 weeks from acceptance to publication February 2012; doi: 10.4049/jimmunol.1101764 http://www.jimmunol.org/content/188/7/3088 MF59 and Pam3CSK4 Boost Adaptive Responses to Influenza Subunit Vaccine through an IFN Type I-Independent Mechanism of Action Elena Caproni, Elaine Tritto, Mario Cortese, Alessandro Muzzi, Flaviana Mosca, Elisabetta Monaci, Barbara Baudner, Anja Seubert and Ennio De Gregorio J Immunol cites 33 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription http://www.jimmunol.org/content/suppl/2012/02/21/jimmunol.110176 4.DC1 This article http://www.jimmunol.org/content/188/7/3088.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2012 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Supplementary Material DNA Methylation in Inflammatory Pathways Modifies the Association Between BMI and Adult-Onset Non- Atopic
Supplementary Material DNA Methylation in Inflammatory Pathways Modifies the Association between BMI and Adult-Onset Non- Atopic Asthma Ayoung Jeong 1,2, Medea Imboden 1,2, Akram Ghantous 3, Alexei Novoloaca 3, Anne-Elie Carsin 4,5,6, Manolis Kogevinas 4,5,6, Christian Schindler 1,2, Gianfranco Lovison 7, Zdenko Herceg 3, Cyrille Cuenin 3, Roel Vermeulen 8, Deborah Jarvis 9, André F. S. Amaral 9, Florian Kronenberg 10, Paolo Vineis 11,12 and Nicole Probst-Hensch 1,2,* 1 Swiss Tropical and Public Health Institute, 4051 Basel, Switzerland; [email protected] (A.J.); [email protected] (M.I.); [email protected] (C.S.) 2 Department of Public Health, University of Basel, 4001 Basel, Switzerland 3 International Agency for Research on Cancer, 69372 Lyon, France; [email protected] (A.G.); [email protected] (A.N.); [email protected] (Z.H.); [email protected] (C.C.) 4 ISGlobal, Barcelona Institute for Global Health, 08003 Barcelona, Spain; [email protected] (A.-E.C.); [email protected] (M.K.) 5 Universitat Pompeu Fabra (UPF), 08002 Barcelona, Spain 6 CIBER Epidemiología y Salud Pública (CIBERESP), 08005 Barcelona, Spain 7 Department of Economics, Business and Statistics, University of Palermo, 90128 Palermo, Italy; [email protected] 8 Environmental Epidemiology Division, Utrecht University, Institute for Risk Assessment Sciences, 3584CM Utrecht, Netherlands; [email protected] 9 Population Health and Occupational Disease, National Heart and Lung Institute, Imperial College, SW3 6LR London, UK; [email protected] (D.J.); [email protected] (A.F.S.A.) 10 Division of Genetic Epidemiology, Medical University of Innsbruck, 6020 Innsbruck, Austria; [email protected] 11 MRC-PHE Centre for Environment and Health, School of Public Health, Imperial College London, W2 1PG London, UK; [email protected] 12 Italian Institute for Genomic Medicine (IIGM), 10126 Turin, Italy * Correspondence: [email protected]; Tel.: +41-61-284-8378 Int. -

Typhoid-Like Disease Mutants Confer Susceptibility to Acute Induced STAT4
Altered IFN- −γ Mediated Immunity and Transcriptional Expression Patterns in N -Ethyl-N-Nitrosourea−Induced STAT4 Mutants Confer Susceptibility to Acute This information is current as Typhoid-like Disease of September 25, 2021. Megan M. Eva, Kyoko E. Yuki, Shauna M. Dauphinee, Jeremy A. Schwartzentruber, Michal Pyzik, Marilène Paquet, Mark Lathrop, Jacek Majewski, Silvia M. Vidal and Danielle Malo Downloaded from J Immunol 2014; 192:259-270; Prepublished online 27 November 2013; doi: 10.4049/jimmunol.1301370 http://www.jimmunol.org/content/192/1/259 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2013/11/27/jimmunol.130137 Material 0.DC1 References This article cites 76 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/192/1/259.full#ref-list-1 by guest on September 25, 2021 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. -

Anti-Cd172b / SIRPB1 Antibody (ARG55858)
Product datasheet [email protected] ARG55858 Package: 100 μl anti-CD172b / SIRPB1 antibody Store at: -20°C Summary Product Description Rabbit Polyclonal antibody recognizes CD172b / SIRPB1 Tested Reactivity Hu Tested Application IHC-P, WB Host Rabbit Clonality Polyclonal Isotype IgG Target Name CD172b / SIRPB1 Antigen Species Human Immunogen KLH-conjugated synthetic peptide corresponding to aa. 17-43 (N-terminus) of Human CD172b / SIRPB1. Conjugation Un-conjugated Alternate Names SIRP-beta-1 isoform 3; CD172b; SIRP-BETA-1; Signal-regulatory protein beta-1 isoform 3 Application Instructions Application table Application Dilution IHC-P 1:25 WB 1:1000 Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Positive Control A375 Calculated Mw 43 kDa Properties Form Liquid Purification Purification with Protein A and immunogen peptide. Buffer PBS and 0.09% (W/V) Sodium azide Preservative 0.09% (W/V) Sodium azide Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C or below. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. Note For laboratory research only, not for drug, diagnostic or other use. www.arigobio.com 1/2 Bioinformation Database links GeneID: 10326 Human Swiss-port # O00241 Human Gene Symbol SIRPB1 Gene Full Name signal-regulatory protein beta 1 Background The protein encoded by this gene is a member of the signal-regulatory-protein (SIRP) family, and also belongs to the immunoglobulin superfamily. -

Supplementary Table 1
Supplementary Table 1. 492 genes are unique to 0 h post-heat timepoint. The name, p-value, fold change, location and family of each gene are indicated. Genes were filtered for an absolute value log2 ration 1.5 and a significance value of p ≤ 0.05. Symbol p-value Log Gene Name Location Family Ratio ABCA13 1.87E-02 3.292 ATP-binding cassette, sub-family unknown transporter A (ABC1), member 13 ABCB1 1.93E-02 −1.819 ATP-binding cassette, sub-family Plasma transporter B (MDR/TAP), member 1 Membrane ABCC3 2.83E-02 2.016 ATP-binding cassette, sub-family Plasma transporter C (CFTR/MRP), member 3 Membrane ABHD6 7.79E-03 −2.717 abhydrolase domain containing 6 Cytoplasm enzyme ACAT1 4.10E-02 3.009 acetyl-CoA acetyltransferase 1 Cytoplasm enzyme ACBD4 2.66E-03 1.722 acyl-CoA binding domain unknown other containing 4 ACSL5 1.86E-02 −2.876 acyl-CoA synthetase long-chain Cytoplasm enzyme family member 5 ADAM23 3.33E-02 −3.008 ADAM metallopeptidase domain Plasma peptidase 23 Membrane ADAM29 5.58E-03 3.463 ADAM metallopeptidase domain Plasma peptidase 29 Membrane ADAMTS17 2.67E-04 3.051 ADAM metallopeptidase with Extracellular other thrombospondin type 1 motif, 17 Space ADCYAP1R1 1.20E-02 1.848 adenylate cyclase activating Plasma G-protein polypeptide 1 (pituitary) receptor Membrane coupled type I receptor ADH6 (includes 4.02E-02 −1.845 alcohol dehydrogenase 6 (class Cytoplasm enzyme EG:130) V) AHSA2 1.54E-04 −1.6 AHA1, activator of heat shock unknown other 90kDa protein ATPase homolog 2 (yeast) AK5 3.32E-02 1.658 adenylate kinase 5 Cytoplasm kinase AK7 -

Genome Wide Methylome Alterations in Lung Cancer
RESEARCH ARTICLE Genome Wide Methylome Alterations in Lung Cancer Nandita Mullapudi1☯, Bin Ye2☯, Masako Suzuki3, Melissa Fazzari3, Weiguo Han1, Miao K. Shi1, Gaby Marquardt1, Juan Lin4, Tao Wang5, Steven Keller6, Changcheng Zhu7, Joseph D. Locker7¤, Simon D. Spivack1,3,5* 1 Department of Medicine/Pulmonary, Albert Einstein College of Medicine, Bronx, New York, United States of America, 2 Department of Bioinformatics, Albert Einstein College of Medicine, Bronx, New York, United States of America, 3 Department of Genetics, Albert Einstein College of Medicine, Bronx, New York, United States of America, 4 Department of Epidemiology & Population Health, Division of Biostatistics, Albert Einstein College of Medicine, Bronx, New York, United States of America, 5 Department of Epidemiology & Population Health, Albert Einstein College of Medicine, Bronx, New York, United States of America, 6 Department of Cardiovascular &Thoracic Surgery, Montefiore Medical Center, Bronx, New York, United States of America, a11111 7 Department of Pathology, Montefiore Medical Center, Bronx, New York, United States of America ☯ These authors contributed equally to this work. ¤ Current address: Department of Pathology, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, United States of America * [email protected] OPEN ACCESS Abstract Citation: Mullapudi N, Ye B, Suzuki M, Fazzari M, Han W, Shi MK, et al. (2015) Genome Wide Aberrant cytosine 5-methylation underlies many deregulated elements of cancer. Among Methylome Alterations in -

HIT'ndrive: Patient-Specific Multi-Driver Gene Prioritization for Precision Oncology
Downloaded from genome.cshlp.org on October 3, 2021 - Published by Cold Spring Harbor Laboratory Press HIT’nDRIVE: Patient-Specific Multi-Driver Gene Prioritization for Precision Oncology Raunak Shrestha1,2,∗, Ermin Hodzic3,∗, Thomas Sauerwald4, Phuong Dao5, Kendric Wang2, Jake Yeung2, Shawn Anderson2, Fabio Vandin6, Gholamreza Haffari7, Colin C. Collins2,8, and S. Cenk Sahinalp2,3,9,† 1Bioinformatics Training Program, University of British Columbia, Vancouver, BC, Canada. 2Laboratory for Advanced Genome Analysis, Vancouver Prostate Centre, Vancouver, BC, Canada. 3School of Computing Science, Simon Fraser University, Burnaby, BC, Canada. 4Computer Laboratory, University of Cambridge, Cambridge, UK. 5National Center for Biotechnology Information, NLM, NIH, Bethesda, MD, USA. 6Department of Information Engineering, University of Padova, Padova, Italy. 7Faculty of Information Technology, Monash University, Melbourne, Australia. 8Department of Urologic Sciences, University of British Columbia, Vancouver, BC, Canada. 9School of Informatics and Computing, Indiana University, Bloomington, IN, USA. *Co-first authors †Correspondence: [email protected] Running Title: Computational prioritization of cancer driver genes Keywords: Driver gene prediction, random walk facility location, multi-hitting time, driver based phenotype inference, driver module, precision oncology Corresponding Author: S. Cenk Sahinalp School of Computing Science, Simon Fraser University Burnaby, BC V5A 1S6, Canada Email: [email protected] School of Informatics and Computing, Indiana University, Bloomington, IN 47405, USA Email: [email protected] Downloaded from genome.cshlp.org on October 3, 2021 - Published by Cold Spring Harbor Laboratory Press Abstract Prioritizing molecular alterations that act as drivers of cancer remains a crucial bottleneck in therapeutic development. Here we introduce HIT’nDRIVE, a computational method that integrates genomic and transcriptomic data to identify a set of patient-specific, sequence-altered genes, with sufficient collective influence over dysregulated transcripts. -

HIT'ndrive: Patient-Specific Multidriver Gene Prioritization for Precision Oncology
Downloaded from genome.cshlp.org on October 4, 2021 - Published by Cold Spring Harbor Laboratory Press Method HIT’nDRIVE: patient-specific multidriver gene prioritization for precision oncology Raunak Shrestha,1,2,10 Ermin Hodzic,3,10 Thomas Sauerwald,4 Phuong Dao,5 Kendric Wang,2 Jake Yeung,2 Shawn Anderson,2 Fabio Vandin,6 Gholamreza Haffari,7 Colin C. Collins,2,8 and S. Cenk Sahinalp2,3,9 1Bioinformatics Training Program, University of British Columbia, Vancouver, British Columbia, Canada V6T 1Z4; 2Laboratory for Advanced Genome Analysis, Vancouver Prostate Centre, Vancouver, British Columbia, Canada V6H 3Z6; 3School of Computing Science, Simon Fraser University, Burnaby, British Columbia, Canada V5A 1S6; 4Computer Laboratory, University of Cambridge, Cambridge CB3 0FD, United Kingdom; 5National Center for Biotechnology Information, National Library of Medicine, National Institutes of Health, Bethesda, Maryland 20894, USA; 6Department of Information Engineering, University of Padova, 35131 Padova, Italy; 7Faculty of Information Technology, Monash University, Melbourne 3800, Australia; 8Department of Urologic Sciences, University of British Columbia, Vancouver, British Columbia, Canada V5Z 1M9; 9School of Informatics and Computing, Indiana University, Bloomington, Indiana 47408, USA Prioritizing molecular alterations that act as drivers of cancer remains a crucial bottleneck in therapeutic development. Here we introduce HIT’nDRIVE, a computational method that integrates genomic and transcriptomic data to identify a set of patient-specific, sequence-altered genes, with sufficient collective influence over dysregulated transcripts. HIT’nDRIVE aims to solve the “random walk facility location” (RWFL) problem in a gene (or protein) interaction network, which differs from the standard facility location problem by its use of an alternative distance measure: “multihitting time,” the expected length of the shortest random walk from any one of the set of sequence-altered genes to an expression-altered target gene. -
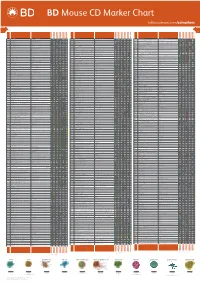
Mouse CD Marker Chart Bdbiosciences.Com/Cdmarkers
BD Mouse CD Marker Chart bdbiosciences.com/cdmarkers 23-12400-01 CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD1d CD1.1, CD1.2, Ly-38 Lipid, Glycolipid Ag + + + + + + + + CD104 Integrin b4 Laminin, Plectin + DNAX accessory molecule 1 (DNAM-1), Platelet and T cell CD226 activation antigen 1 (PTA-1), T lineage-specific activation antigen 1 CD112, CD155, LFA-1 + + + + + – + – – CD2 LFA-2, Ly-37, Ly37 CD48, CD58, CD59, CD15 + + + + + CD105 Endoglin TGF-b + + antigen (TLiSA1) Mucin 1 (MUC1, MUC-1), DF3 antigen, H23 antigen, PUM, PEM, CD227 CD54, CD169, Selectins; Grb2, β-Catenin, GSK-3β CD3g CD3g, CD3 g chain, T3g TCR complex + CD106 VCAM-1 VLA-4 + + EMA, Tumor-associated mucin, Episialin + + + + + + Melanotransferrin (MT, MTF1), p97 Melanoma antigen CD3d CD3d, CD3 d chain, T3d TCR complex + CD107a LAMP-1 Collagen, Laminin, Fibronectin + + + CD228 Iron, Plasminogen, pro-UPA (p97, MAP97), Mfi2, gp95 + + CD3e CD3e, CD3 e chain, CD3, T3e TCR complex + + CD107b LAMP-2, LGP-96, LAMP-B + + Lymphocyte antigen 9 (Ly9), -

SUPPLEMENTARY APPENDIX a Clinico-Molecular Predictor Identifies Follicular Lymphoma Patients at Risk of Early Transformation After First-Line Immunotherapy
SUPPLEMENTARY APPENDIX A clinico-molecular predictor identifies follicular lymphoma patients at risk of early transformation after first-line immunotherapy Chloé B. Steen, 1,2 Ellen Leich, 3 June H. Myklebust, 2,4 Sandra Lockmer, 5 Jillian F. Wise, 2,4 Björn E. Wahlin, 5 Bjørn Østenstad, 6 Knut Liestøl, 1,7 Eva Kimby, 5 Andreas Rosenwald, 3 Erlend B. Smeland, 2,4 Harald Holte, 4,6 Ole Christian Lingjærde 1,4,8,* and Marianne Brodtkorb 2,4,6,* *OCL and MB contributed equally to this study. 1Department of Informatics, University of Oslo, Oslo, Norway; 2Department of Cancer Immunology, Institute for Cancer Research, Oslo University Hospital, Oslo, Norway; 3Institute of Pathology, University of Wu rzburg and Comprehensive Cancer Centre Mainfranken, Germany; 4KG Jebsen Centre for B-Cell Ma - lignancies, Institute for Clinical Medicine, University of Ö slo, Oslo, Norway; 5Division of Haematology, Department of Medicine at Huddinge, Karolinska Insti - tute and University Hospital, Stockholm, Sweden; 6Department of Oncology, Oslo University Hospital, Oslo, Norway; 7Institute for Cancer Genetics and Informatics, Oslo University Hospital, Oslo, Norway; and 8Department of Cancer Genetics, Institute for Cancer Research, Oslo University Hospital, Oslo, Nor - way Correspondence: OLE C. LINGJÆRDE - [email protected] MARIANNE BRODTKORB - [email protected] doi:10.3324/haematol.2018.209080 SUPPLEMENTAL MATERIAL For the paper: Steen CB, Leich E, Myklebust JH, Lockmer S, Wise JF, Wahlin B, Østenstad B, Liestøl K, Kimby E, Rosenwald A, Smeland EB, Holte H, Lingjærde OC and Brodtkorb M. A clinico- molecular predictor identifies follicular lymphoma patients at risk of early transformation after first-line immunotherapy Contents: 1.