Breath-Testing Has Developed Into an Important Diagnostic Tool In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Fructose Hydrogen Breath Test: Nothing Behind the Sweet Fog?
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2019 The Fructose Hydrogen Breath Test: Nothing Behind the Sweet Fog? Misselwitz, Benjamin ; Fox, Mark DOI: https://doi.org/10.1159/000491747 Posted at the Zurich Open Repository and Archive, University of Zurich ZORA URL: https://doi.org/10.5167/uzh-161035 Journal Article Published Version Originally published at: Misselwitz, Benjamin; Fox, Mark (2019). The Fructose Hydrogen Breath Test: Nothing Behind the Sweet Fog? Digestion, 99(3):191-193. DOI: https://doi.org/10.1159/000491747 Editorial Digestion Published online: September 13, 2018 DOI: 10.1159/000491747 The Fructose Hydrogen Breath Test: Nothing Behind the Sweet Fog? a b Benjamin Misselwitz Mark Fox a Division of Gastroenterology and Hepatology, University Hospital Zurich, University of Zurich, Zurich, Switzerland; b Abdominal Center: Gastroenterology, St. Claraspital, Basel, Switzerland Fructose consumption has steadily increased in West- “malabsorption,” assessed by high H2 values in expiratory ern countries, with adolescents consuming up to 70 g of air and (ii) symptoms after oral fructose challenge (“in- fructose per day [1]. Apples, pears or grapes contain ~8 g tolerance”). To date, the clinical impact of FHBT remains fructose per 100 g; however, most fructose intake is de- unclear. rived from processed sugars in many contemporary foods A paper in this issue of Digestion addresses this ques- and sweetened beverages. Fructose is 1.5–2.5 times sweet- tion (Helwig et al. [6], Digestion, 2018). The authors er than glucose; however, it fails to activate normal satiety analyze 562 consecutive 50 g FHBT. -

Indiana University Health Gi Motility Lab & Gastric
INDIANA UNIVERSITY HEALTH GI MOTILITY LAB & GASTRIC ELECTRICAL STIMULATION PROGRAM HYDROGEN BREATH TEST HYDROGEN BREATH TEST- A hydrogen breath test provides information about the digestion of certain sugars or carbohydrates, such as milk sugar (lactose) or fruit sugar (fructose). This will help determine if you are intolerant to certain sugars. This is a very simple and non-painful test to do. But it does require some planning and preparation on your part. Please follow all instruction as listed below. How Do I Prepare For The Procedure? 1. For two weeks before your test a. You cannot take any antibiotics b. You cannot take any probiotics (over-the-counter). 2. For one week before your test, do not take any laxatives or stool softeners (for example Colace, Milk of Magnesia, Ex-Lax) or stool bulking agents (for example Metamucil or Citrucel) if possible. You should also not undergo any test that requires cleansing of the bowel, such as colonoscopy or barium enema. 3. For 48 hours prior to your test, do not take Prokinetic drugs (metoclopramide [Reglan], domperidone [Motilium], erythromycin, azithromycin) and opiate pain meds (hydrocodone, oxycodone, morphine, hydromorphone). 4. For 48 hours prior to your test avoid beans, pasta, fiber cereals, and high fiber foods. 5. The day before your test: a. You may consume only the following foods and drinks: plain white bread, plain white rice, plain white potatoes, baked or broiled chicken, fish, or turkey, eggs, clear chicken or beef broth, water, non-flavored black coffee or tea. b. Only salt and pepper may be used to flavor your food. -
Implementation and Interpretation of Hydrogen Breath Tests
IOP PUBLISHING JOURNAL OF BREATH RESEARCH J. Breath Res. 2 (2008) 046002 (9pp) doi:10.1088/1752-7155/2/4/046002 Implementation and interpretation of hydrogen breath tests Alexander Eisenmann1, Anton Amann2,4, Michael Said3, Bettina Datta1 and Maximilian Ledochowski1,4,5 1 Department of Clinical Nutrition, Medical Hospital of Innsbruck, Austria 2 Department of Anesthesia and General Intensive Care, Medical University of Innsbruck, Austria 3 Department of Medicine, Military Hospital 2, Innsbruck, Austria 4 Breath Research Unit of the Austrian Academy of Sciences, Dammstr 22, 6850 Dornbirn, Austria E-mail: [email protected] Received 29 May 2008, in final form 2 July 2008 Published 24 July 2008 Online at stacks.iop.org/JBR/2/046002 Abstract Hydrogen breath tests are non-invasive and safe diagnostic tools used to investigate functional intestinal disorders. For the diagnosis of fructose or lactose malabsorption as well as for the detection of small intestinal bacterial overgrowth syndrome, hydrogen breath tests are even regarded as gold standard. However, standardization of the testing procedure and the interpretation of the test results are still lacking. In this paper, reliable information on the implementation of the most common hydrogen breath tests and precise guidelines for the interpretation of the test results are presented. (Some figures in this article are in colour only in the electronic version) 1. Introduction sugar molecules, which, as part of a fermentation reaction, are initially broken down into short-chain fatty acids (SCFA), At present, it is known that the exhaled breath of human beings carbon dioxide (CO2) and hydrogen (H2), as illustrated in contains at least 2000 different substances and that, apart from figure 1. -
A Zero Carbohydrate, Carnivore Diet Can Normalize Hydrogen Positive Small Intestinal Bacterial Overgrowth Lactulose Breath Tests: a Case Report
A Zero Carbohydrate, Carnivore Diet can Normalize Hydrogen Positive Small Intestinal Bacterial Overgrowth Lactulose Breath Tests: A Case Report Peter Martin FunMed Gothenburg Sweden Martina Johansson ( [email protected] ) Institution for Medicine and health https://orcid.org/0000-0001-7031-2892 Annelie Ek FunMed Gothenburg Research article Keywords: Zero carbohydrate, carnivore diet, small intestinal bacterial overgrowth, SIBO, lactulose hy-drogen breath testing, nutritional intervention. Posted Date: January 19th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-148500/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/13 Abstract Background: Small intestinal bacterial overgrowth (SIBO) is a clinical condition characterized by an excessive bacterial growth in the small intestine. Clinical symptoms might be non-specic (dyspepsia, bloating or abdominal discomfort). Nevertheless, SIBO can cause severe malabsorption, serious malnutrition, immune reactions, and deciency syndromes. This retrospective case report introduces six patients with positive lactulose hydrogen SIBO breath tests. The patients chose between different therapeutic options and willingly consented to a nutritional intervention, based on a zero carbohydrate, zero bre, carnivore diet, extended over two to six weeks of time. The rationale for this dietary approach was based on the idea that opportunistic, carbohydrate favouring bacteria and methanogens proliferate in the small intestines if the natural barriers in the digestive tract have been weakened due to stress, illness, medication, etc. A zero carbohydrate, carnivore diet, consisting of animal fats and protein, could essentially eliminate these carbohydrate favouring bacteria through starvation while still providing plenty of both calories and nutrients. -

Hydrogen Breath Test – Patient Instructions For
Hydrogen Breath Test – Patient Preparation Any queries, please call WCH Gastroenterology Breath Testing Service: 08 8161 7275 These instructions apply to breath tests for Lactose, Fructose or Sucrose Malabsorption and also for the Lactulose breath test. The Lactulose test is used to determine whether a patient is a hydrogen producer or to detect a Small Bowel Bacterial Overgrowth. Only 1 test can be done each day. Failure to follow the preparation may lead to an inconclusive result requiring the test(s) to be repeated. COST: These tests incur a cost. FOR 4 WEEKS BEFORE YOUR TEST: No antibiotics No colonoscopy FOR 2 WEEKS BEFORE YOUR TEST: No concentrated Probiotics such as IBS Support, Inner Health Plus or VSL#3 No enemas THE DAY BEFORE YOUR TEST: FOODS TO AVOID SUGGESTED FOODS INCLUDE High fibre foods – wholegrain cereals and Low fibre foods - White bread, white rice, rice wholegrain breads, bran, oats noodles, rice crackers Honey, peanut butter, jam Rice Bubbles, Cornflakes, pancakes Pasta, tofu, processed meats Lactose-free milk, hard cheeses, margarine, Fermented foods eg yoghurt, soy, kombucha Nuttelex, vegemite Soft drinks, sports drinks, fruit juice, cordial Black tea (not herbal), coffee, water Legumes - beans, peas, lentils, nuts, corn Chicken, fish, seafood, lean beef, eggs Dried fruit, pears, stone fruit, canned fruit, Fresh fruit (1 handful per 3 hr period) avocado eg melon, citrus, banana, berries Onions, garlic, cabbage, celery, broccoli Peeled vegetables eg. carrot, cucumber, Fibre supplements and laxatives zucchini, -

Hydrogen/Methane Breath Test What Is the Hydrogen/Methane Breath Test?
Hydrogen/Methane Breath Test What is the Hydrogen/Methane Breath Test? The hydrogen/methane breath test is a test that uses the measurement of hydrogen in the breath to diagnose several conditions that cause gastrointestinal symptoms. Large amounts of hydrogen may be produced where there is a problem with the digestion or absorption of food in the small intestine that allows more unabsorbed food to reach the colon or when the colon bacteria move back into the small intestine. Some of the hydrogen produced by the bacteria, whether in the small intestine or the colon, is absorbed into the blood flowing through the wall of the small intestine and colon. The hydrogen-containing blood travels to the lungs where the hydrogen is released and exhaled in the breath where it can be measured. When is Hydrogen Breath Testing Used? • The first condition for which hydrogen breath testing is used is for diagnosing bacterial overgrowth of the small bowel, a condition in which larger-than-normal numbers of colonic bacteria are present in the small intestine. • The second condition for which hydrogen breath testing is used is when dietary sugars are not digested normally. The most common sugar that is poorly digested is lactose, the sugar in milk. Individuals who are unable to properly digest lactose are referred to as lactose intolerant. • The third condition for which hydrogen breath testing is used is for diagnosing rapid passage of food through the small intestine. All three of these conditions may cause abdominal pain, abdominal bloating and distention, flatulence (passing gas in large amounts) and diarrhea. -
Fructose Intolerance
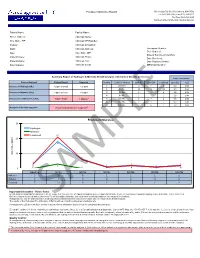
Fructose Intolerance Report 561 Virginia Rd, Ste 100, Concord, MA 01742 Tel (617) 608-3832 | Fax (617) 860-6617 Toll Free (844) 681-9449 Kathleen O'Neil-Smith, M.D., Medical Director Patient Name: Facility Name: Street Address: Clinician Name: City, State, ZIP: Clinician NPI Number: Gender: Clinician Account #: DOB: Clinician Address: Accession Number: Date Ordered: Age: City, State, ZIP: Date of Service (Collection): Patient Phone: Clinician Phone: Date Received: Patient Mobile: Clinician Fax: Date Reported (Final): Patient Email: Clinician Email: MR/Chart Number: Summary Report of Hydrogen & Methane Breath Analysis with Carbon Dioxide Correction Sample Normalization1 Gasses Analyzed Patient Result Expected Number Collection Interval ppm H2 ppm CH4 Combined ppm CO2 fCO2 1 Baseline 3 0 3 3.3 1.66 Increase in Hydrogen (H2) 15 ppm (normal) < 20 ppm 2 30 Min. 18 3 21 3.3 1.66 Increase in Methane (CH4) 3 ppm (normal) < 12 ppm 3 60 Min. 6 0 6 2.9 1.89 4 90 Min. 1 0 1 3.8 1.44 3 Increase in combined H2 & CH4 18 ppm (high) < 15 ppm 5 120 Min. 2 0 2 3.6 1.52 6 150 Min. 1 0 1 3.7 1.48 7 180 Min. 2 0 2 3.4 1.61 Analysis of the data suggests Fructose intolerance is suspected3 Fructose Intolerance 30 Hydrogen Methane Combined 21 20 18 Gas Value (ppm) 10 6 6 3 2 2 3 3 1 1 2 2 0 0 0 10 0 01 0 Baseline 30 Min 60 Min 90 Min 120 Min 150 Min 180 Min Hydrogen 3 18 6 1 2 1 2 Methane 0 3 0 0 0 0 0 Combined 3 21 6 1 2 1 2 Important Information - Please Read: Breath analysis standards for abnormal tests are suggested if an increase of 20ppm for Hydrogen (H 2), 12ppm for Methane (CH4), or a combined 15ppm for Hydrogen (H2) & Methane (CH4) is detected. -

Hydrogen Breath Test for Small Intestinal Bacterial Overgrowth (SIBO) Using Glucose
PRINCESS ALEXANDRA HOSPITAL Procedure SECTION: Clinical Procedure No. 02130/v1/01/2018 PROCEDURE TITLE: Hydrogen Breath Test for Small Intestinal Bacterial Overgrowth (SIBO) using Glucose Review Officer: Senior Scientist, PURPOSE Gastroenterology and Hepatology What is the hydrogen breath test? The hydrogen breath test is a simple painless and non-invasive test Review Summary: v1 used to identify an abnormal growth of bacteria in the small intestine. Applicable To: All Gastroenterology and Hepatology Department Laboratory Staff What is bacterial overgrowth in the intestine? Normally, only small amounts of bacteria are found in the intestine. If Date Introduced: 01/2018 there is a significant increase in the amount of bacteria, food and Next Review Date: 01/2021 nutrients are poorly absorbed. Bacterial overgrowth can result from a slow transit of food through the bowels or from certain medications. Authority: Director of Gastroenterology Symptoms may include abdominal pain, bloating, gas, and diarrhoea. and Hepatology Replaces: New procedure OUTCOME OF THE PROCEDURE This procedure will minimise inconclusive or failed tests and the need Key Words: hydrogen breath test, SIBO, glucose, lactose for the patients to repeat the test at a later date. AUTHOR ISED TO UNDERTAKE THE PROCEDURE Who can do the procedure, what qualifications or training are required? CONTRAINDICATIONS The hydrogen breath test cannot be done following a colonoscopy, barium enema, or any tests that require a bowel prep to be given, since this alters the microbiota profile. Should a bowel prep be undertaken, the Hydrogen breath test should be performed at least 4 weeks post bowel prep to allow the bacteria to re- colonise. -

The Importance of Methane Breath Testing: a Review
Home Search Collections Journals About Contact us My IOPscience The importance of methane breath testing: a review This article has been downloaded from IOPscience. Please scroll down to see the full text article. 2013 J. Breath Res. 7 024001 (http://iopscience.iop.org/1752-7163/7/2/024001) View the table of contents for this issue, or go to the journal homepage for more Download details: IP Address: 72.248.48.173 The article was downloaded on 15/05/2013 at 16:31 Please note that terms and conditions apply. IOP PUBLISHING JOURNAL OF BREATH RESEARCH J. Breath Res. 7 (2013) 024001 (8pp) doi:10.1088/1752-7155/7/2/024001 TOPICAL REVIEW The importance of methane breath testing: a review B P J de Lacy Costello1, M Ledochowski2 and N M Ratcliffe1 1 University of the West of England, Institute of Biosensor Technology, Coldharbour lane, Frenchay, Bristol BS16 1QY, UK 2 Academy of Clinical Nutrition Anichstrasse, 17, A-6020 Innsbruck, Austria E-mail: [email protected] Received 23 October 2012 Accepted for publication 18 December 2012 Published 8 March 2013 Online at stacks.iop.org/JBR/7/024001 Abstract Sugar malabsorption in the bowel can lead to bloating, cramps, diarrhea and other symptoms of irritable bowel syndrome as well as affecting absorption of other nutrients. The hydrogen breath test is now a well established noninvasive test for assessing malabsorption of sugars in the small intestine. However, there are patients who can suffer from the same spectrum of malabsorption issues but who produce little or no hydrogen, instead producing relatively large amounts of methane. -

Breath Testing Referral Fax: 9469-5927 Fax: 9384-1043
RESERVOIR COBURG 73 -75 Pine Street 253 Moreland Road RESERVOIR PRIVATE HOSPITAL Reservoir VIC 3073 Coburg VIC 3058 Phone: 9460-8855 Phone: 9383-5597 Breath Testing Referral Fax: 9469-5927 Fax: 9384-1043 NORTHERN GASTRO HEALTH www.rphdayprocedurecentre.com.au HYDROGEN & METHANE BREATH TESTING PATIENT DETAILS: SYMPTOMS / ASSOCIATED CONDITIONS: Surname: Abdominal bloating First Name: Excessive flatulence Address: Diarrhoea Phone: Mobile: Irritable Bowel Syndrome DOB: Coeliac Disease Crohn’s Disease / Ulcerative Colitis BREATH TESTS & APPOINTMENT DATES: Small Intestine Bacterial Overgrowth Syndrome LACTULOSE Date: / / Other: LACTOSE Date: / / GLUCOSE Date: / / FRUCTOSE Date: / / SUCROSE Date: / / SORBITOL Date: / / REFERRING DR.: All patients should have a baseline Lactulose test Address: determine if they are a Hydrogen producer. Phone: Fax: For Bookings Call – Reservoir: 9460-8855 Signature: Date: / / Coburg: 9383-5597 (All tests start at 9.00am) PLEASE TURN OVER FOR PATIENT INSTRUCTIONS PRESENT THIS REFERRAL FORM WHEN YOU ATTEND FOR YOUR TEST l PATIENT INSTRUCTIONS 73-75 Pine Street, Reservoir VIC 3073 A Hydrogen Breath Test helps diagnose malabsorption of lactose/ fructose/ sorbitol/ glucose, and small bowel Phone: 9460-8855 Fax: 9469-5927 bacterial overgrowth. Malabsorption of sugars found in common food product may cause gastrointestinal symptoms such as bloating, abdominal pain, flatulence and diarrhoea. www.rphdayprocedurecentre.com.au The test is painless and non-invasive and involves measuring breath hydrogen levels for a period of up to 3 hours. Only one test can be done per day. Each test costs $75 with no Medicare rebate available. Tests are payable on the day by EFTPOS, Visa, Mastercard, Bankcard or Cash only. TEST PREPARATION – Below are medications, medical procedures and food products which must be avoided prior to testing : Following these instructions will ensure accurate and reliable results and will be checked on the day in order for your test to proceed. -

Hydrogen Breath Test
Hydrogen Breath Test What is a Hydrogen Breath Test? This is a test for bacterial overgrowth, or intolerance to lactose, fructose, or sucrose. Glucose is a sugar that will be broken down by bacteria (if present) in the small bowel with hydrogen or methane gas as a by-product. The breath sample will be analyzed for hydrogen or methane content to determine if you are able to properly break down the lactose, fructose, or sucrose, or if you have bacterial overgrowth. What can I expect from a Hydrogen Breath Test? This test requires that you drink a mixture of glucose, lactose, fructose, or sucrose in water. • Glucose is a sugar that will be broken down by bacteria (if present) in the small bowel with hydrogen as a by-product. • Lactose is the sugar found in milk and is normally broken down in the small bowel. • Sucrose is a common sugar found in foods such as candy. After drinking the solution, you will be asked to breathe into a plastic bag. Breath samples are obtained every 15 minutes for adults, and every 30 minutes for children. The breath sample will be analyzed for hydrogen content to determine if you are able to properly break down the lactose or sucrose, or if you have bacterial overgrowth. The test for glucose lasts about 2 hours and the test for lactose, fructose, and sucrose lasts about 2-3 hours. The test is performed in the Gastrointestinal Physiology Laboratory of the Medical Procedure Unit. How do I prepare for a Hydrogen Breath Test? Please follow the instructions below to ensure a successful test. -

Making Sense of Patients with Gas and Bloating of Undetermined Origin
GASTROINTESTINAL MOTILITY AND FUNCTIONAL BOWEL DISORDERS, SERIES #10 Richard W. McCallum, MD, FACP, FRACP (Aust), FACG Making Sense of Patients with Gas and Bloating of Undetermined Origin Juan Castro-Combs Evelyn Eichler Richard W. McCallum Unexplained bloating is one of the most common and bothersome gastroenterology complaints in gastrointestinal (GI) specialty and primary care clinics. Abdominal bloating is likely to present in association with other complaints including belching, flatulence, post-prandial distension, borborygmi, abdominal pain and diarrhea. Given the lack of a systematic approach to these complaints, symptomatic patients are often asked to keep a food diary and dietary modifications are suggested. If symptom resolution does not occur, further testing (blood and stool tests, imaging studies, endoscopic procedures) to rule out organic disorders is initiated. A “negative” or unremarkable work up often places patients into the “functional” GI disorder compartment. This article attempts to provide physicians with a simple and rational approach to unexplained abdominal bloating and to identify underdiagnosed entities that could be responsible for this symptom. INTRODUCTION bdominal bloating is a nonspecific term whose have been linked with different pathophysiologic definition varies among gastroenterologists with mechanisms that are not fully understood. Several an even broader meaning for patients in general. functional gastrointestinal disorders (functional A 1,2 1,2,3 Bloating can be defined as the objective abdominal dyspepsia, irritable bowel syndrome (IBS), distention originating from gas or as a subjective functional constipation1,2,4,5 and functional bloating6) feeling of abdominal distention or abdominal wall have bloating as a manifestation despite the absence tension without objective distension.